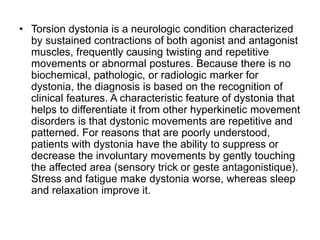
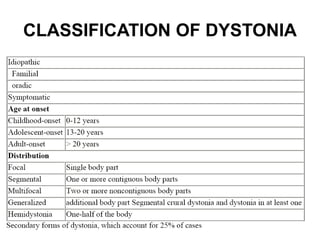
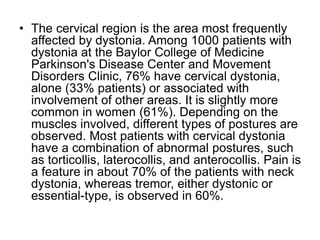
The document discusses various types of movement disorders including Parkinson's disease, parkinsonism, essential tremor, dystonia, and other tremors. It provides details on the symptoms, causes, diagnosis, and treatment of these conditions. Some key points include: tremor, bradykinesia, and rigidity are cardinal signs of parkinsonism; levodopa is commonly used to treat Parkinson's disease; drug-induced parkinsonism and Parkinson's disease can be clinically indistinguishable; cervical dystonia is the most common form of focal dystonia.