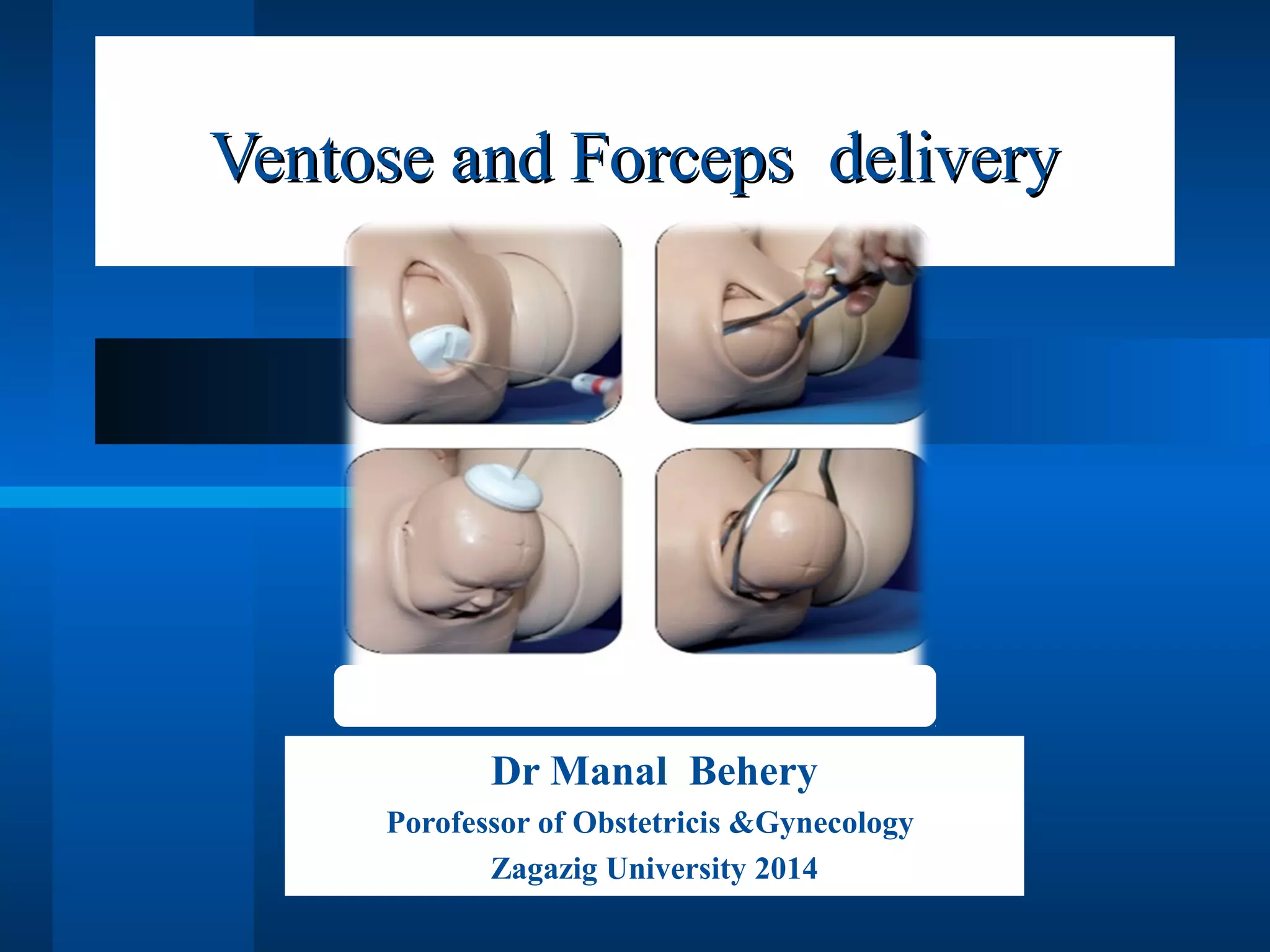
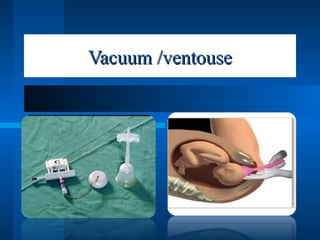
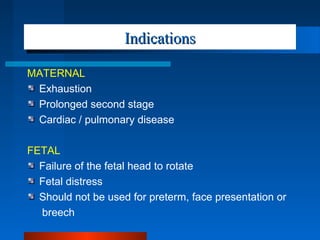
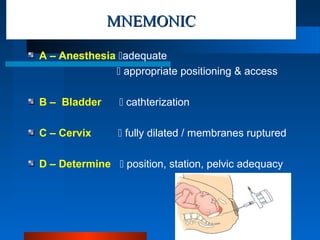
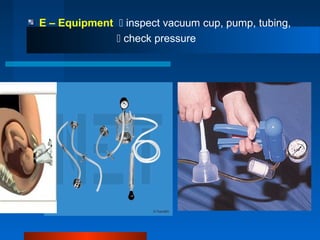
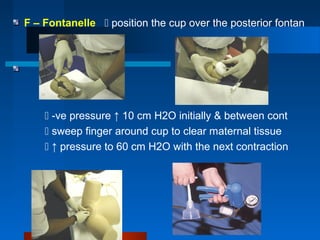
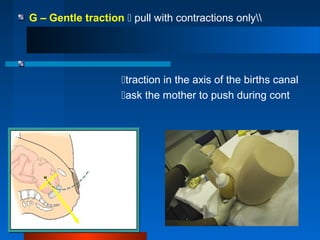
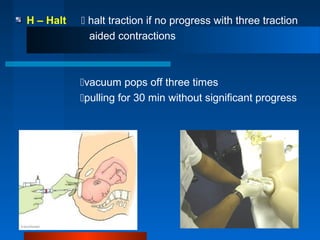
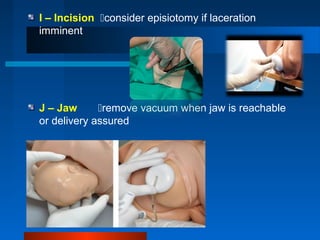
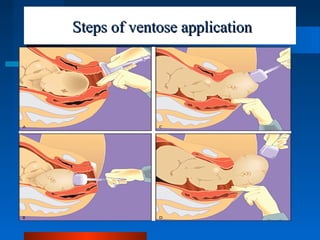
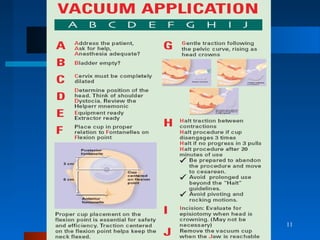
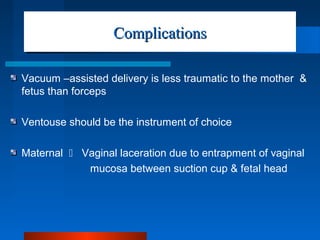
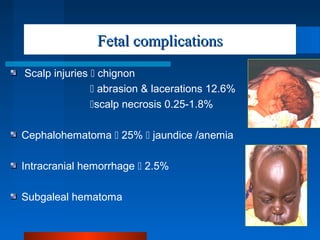
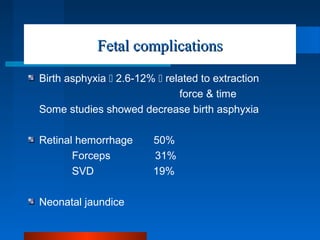
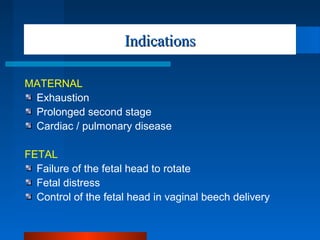
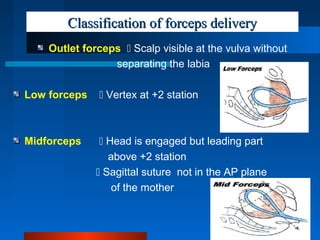
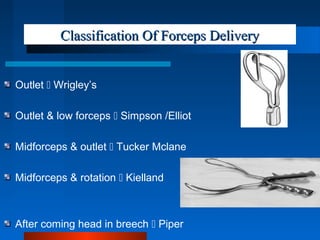
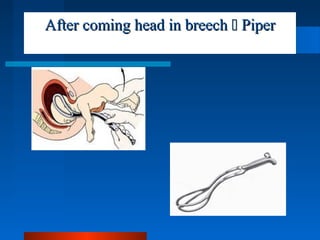
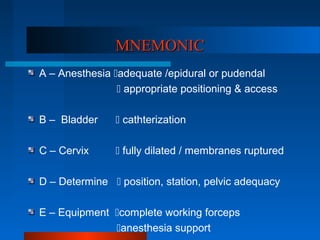
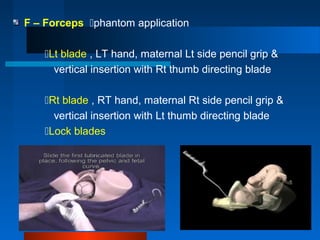
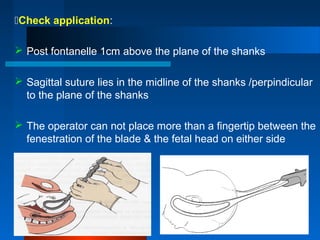
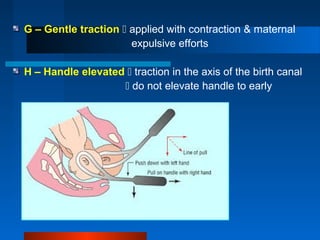
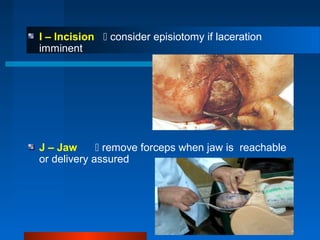
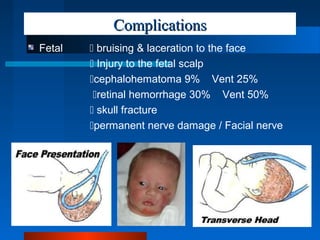
The document discusses the indications, procedures, and complications associated with ventouse and forceps deliveries in obstetrics. It outlines specific conditions under which these methods should be employed, along with mnemonics to guide the process and details of potential maternal and fetal complications. Ventouse is recommended as the preferred instrument due to its less traumatic nature, while forceps delivery is classified into different types based on the station and visibility of the fetal head.