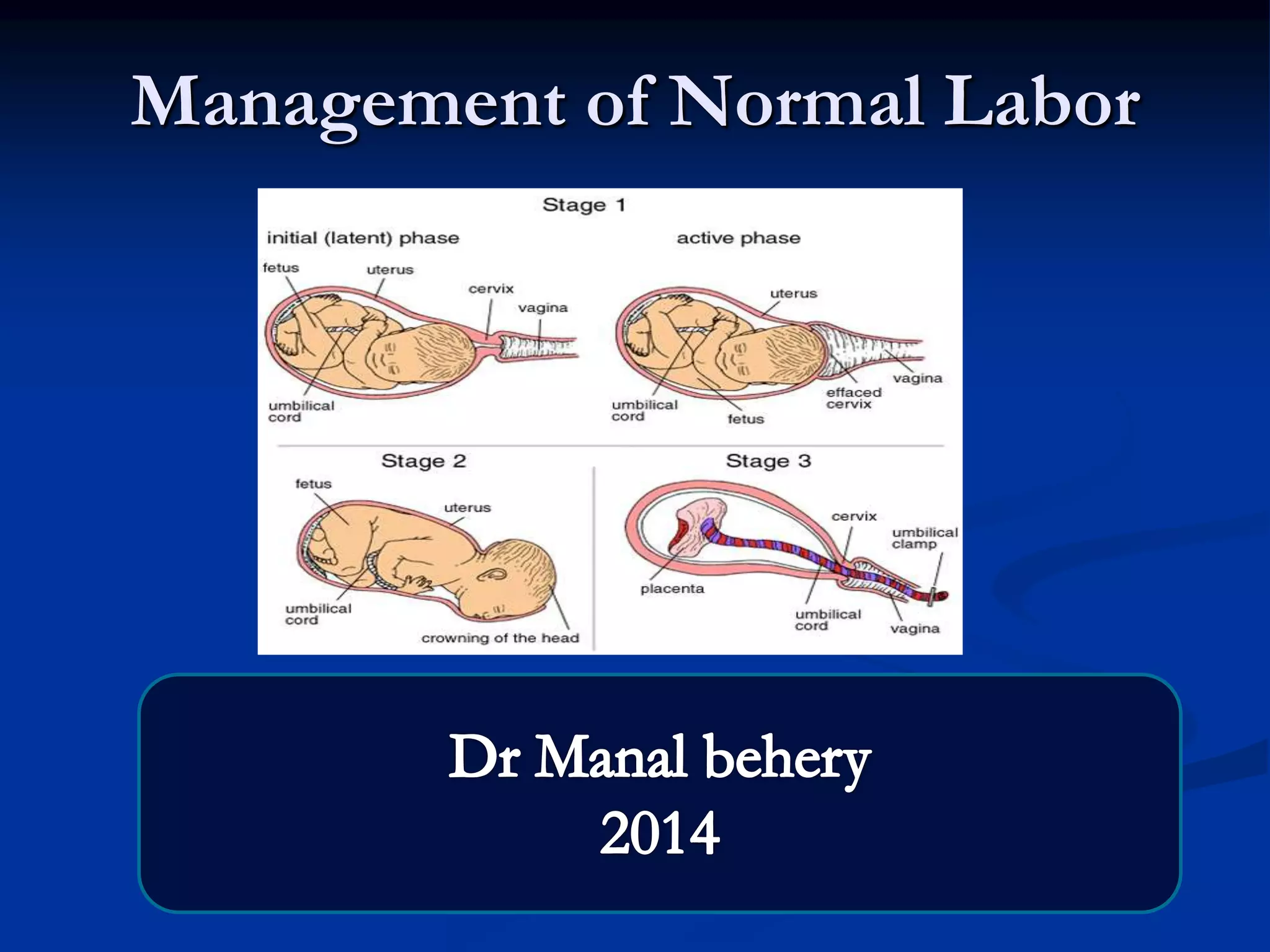
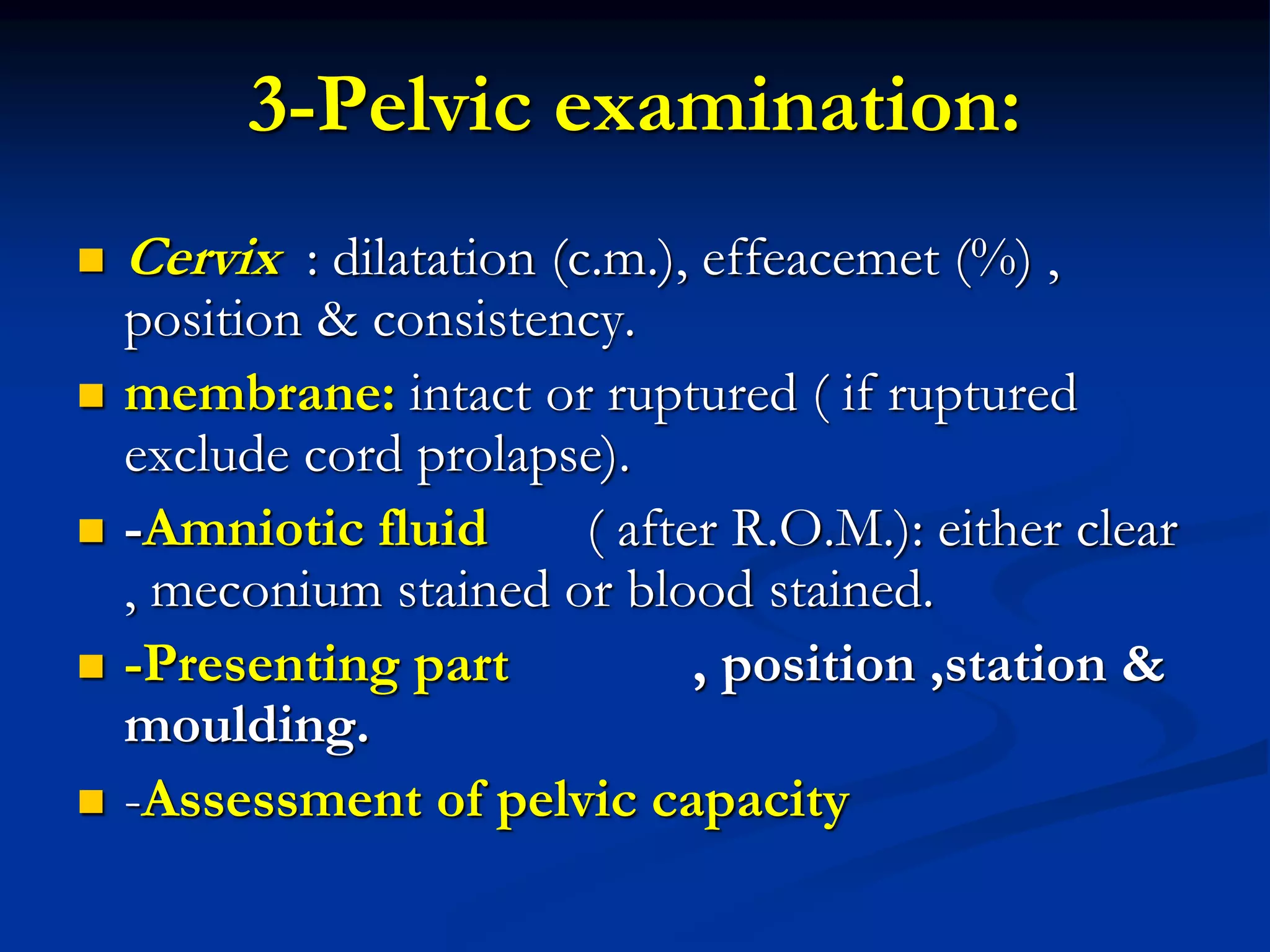
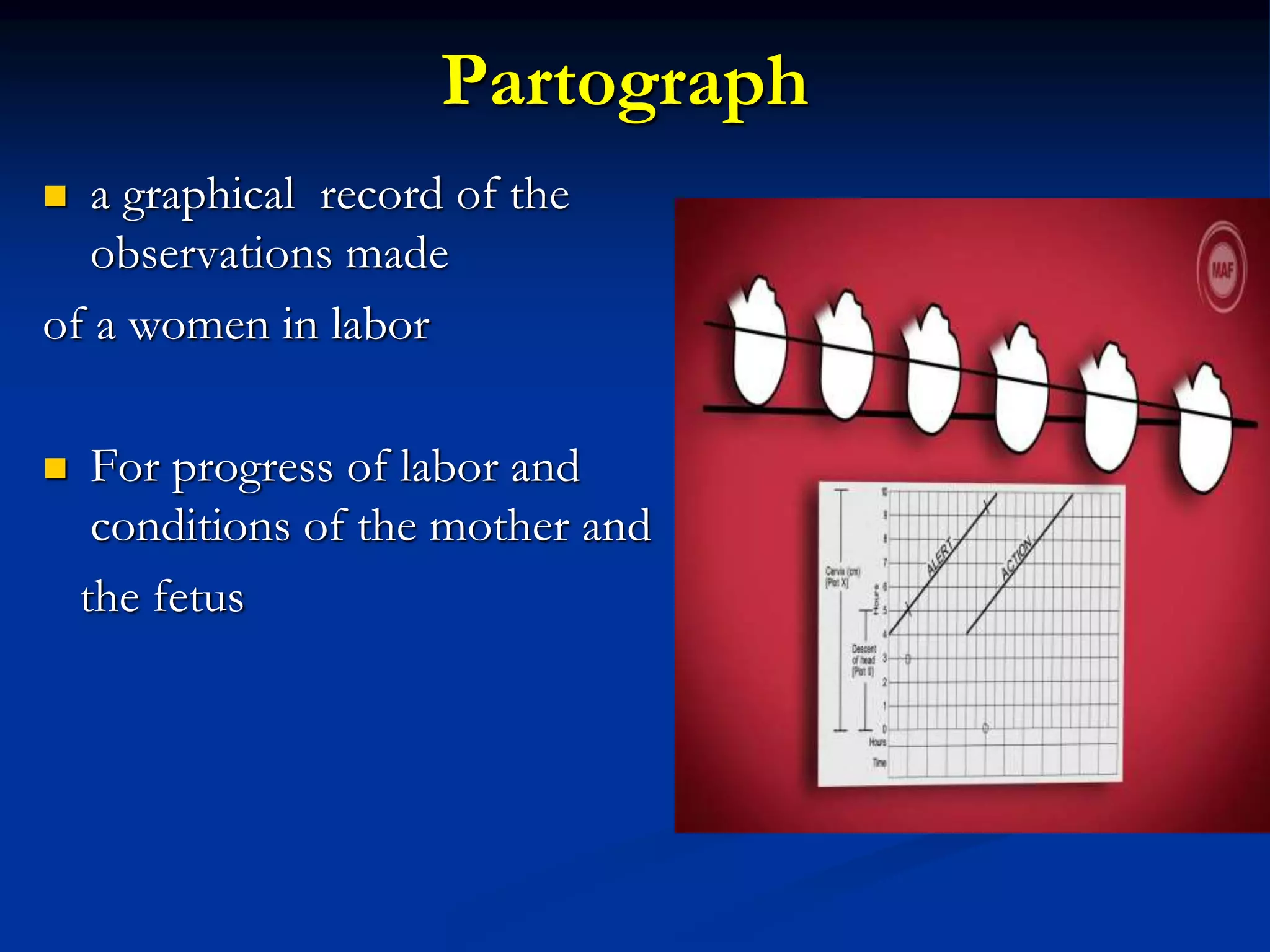
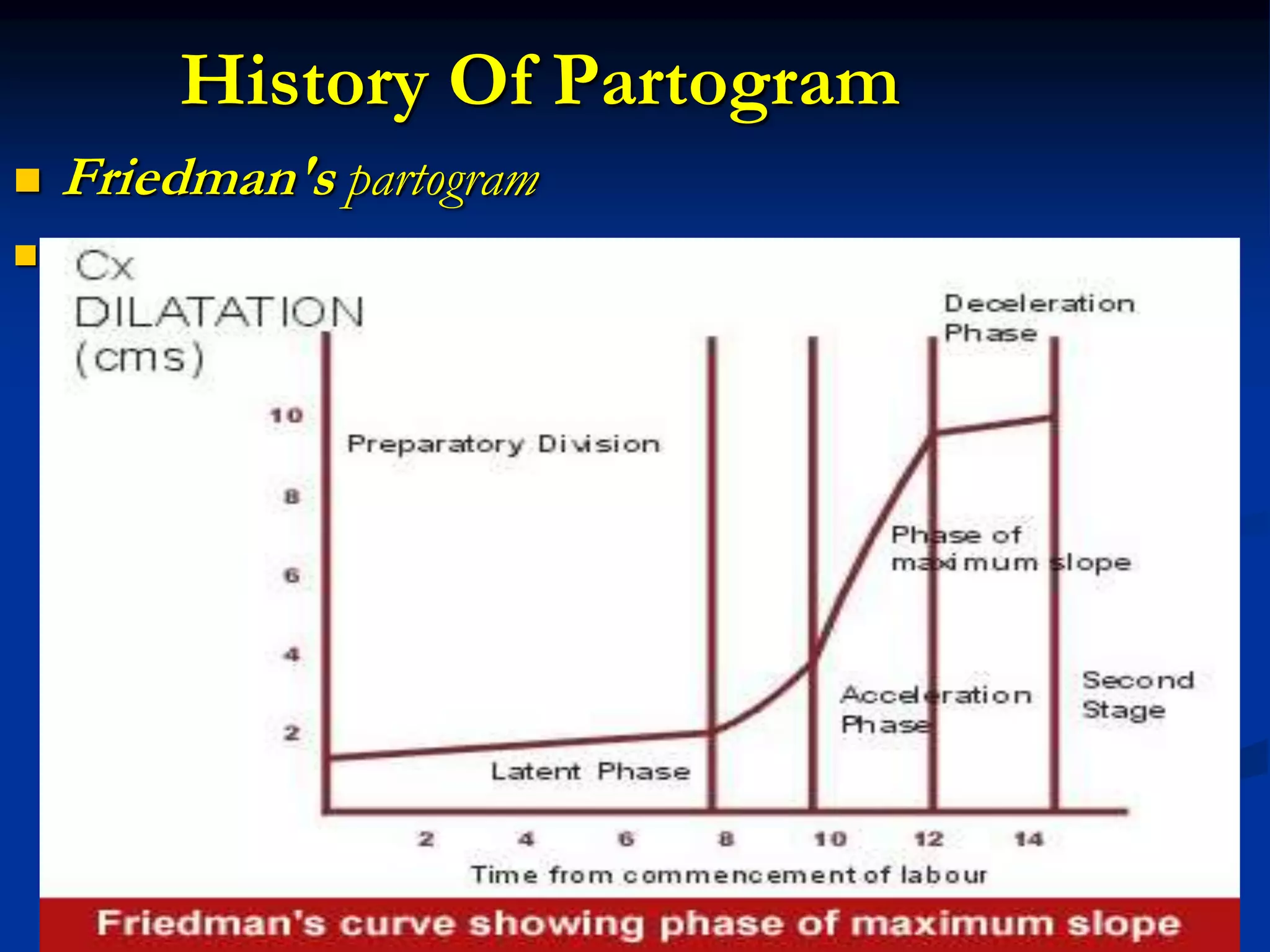
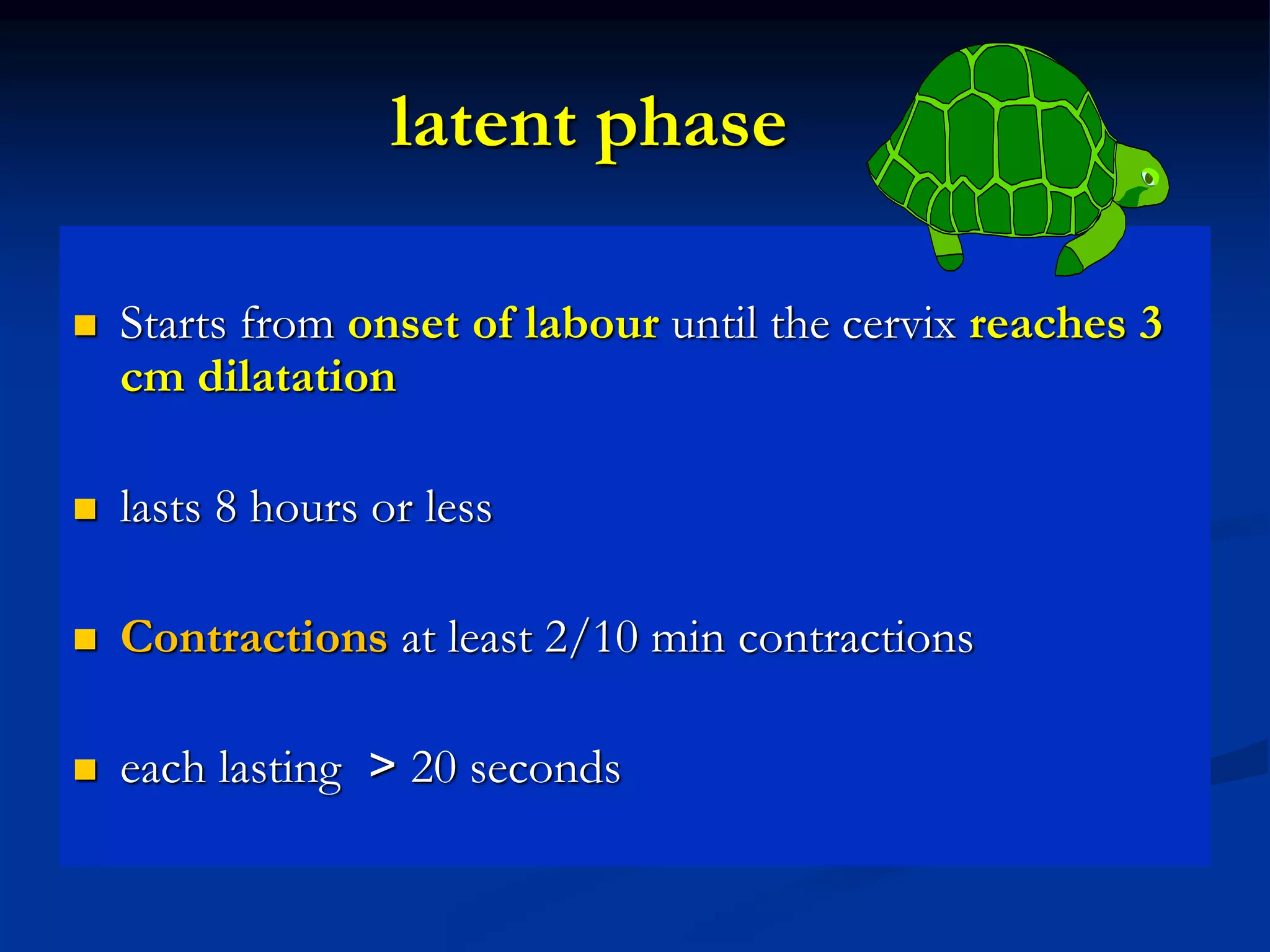
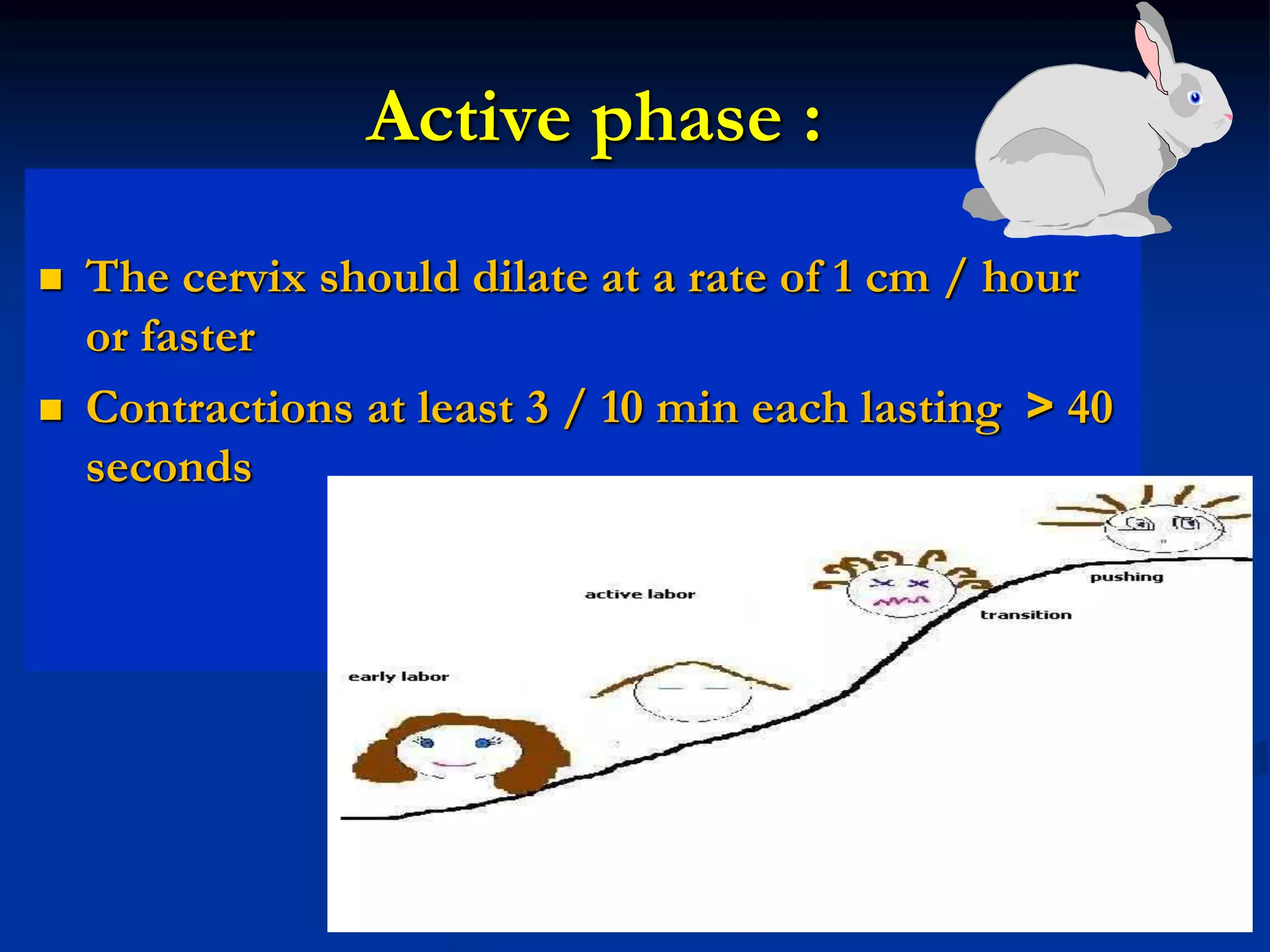
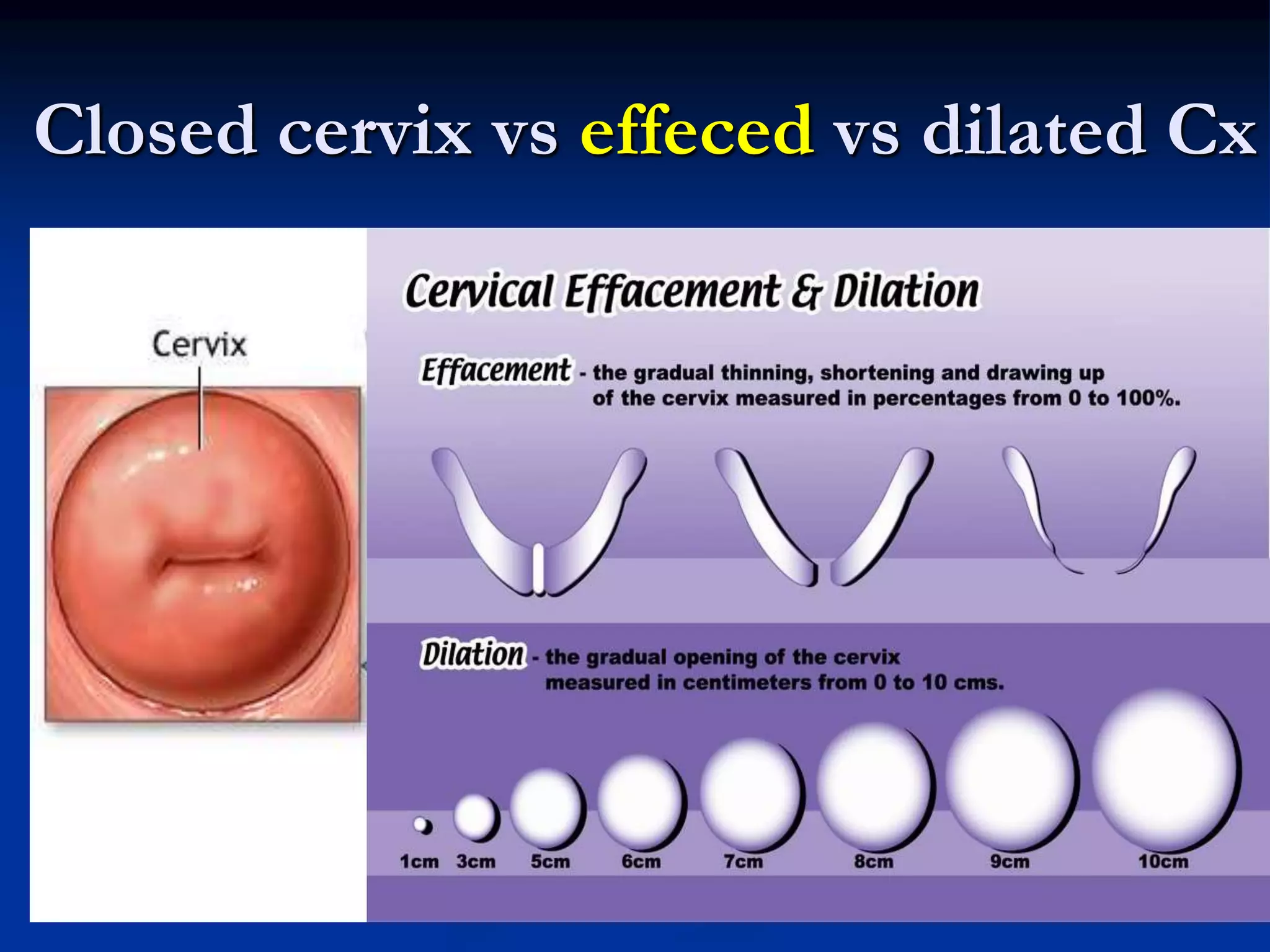
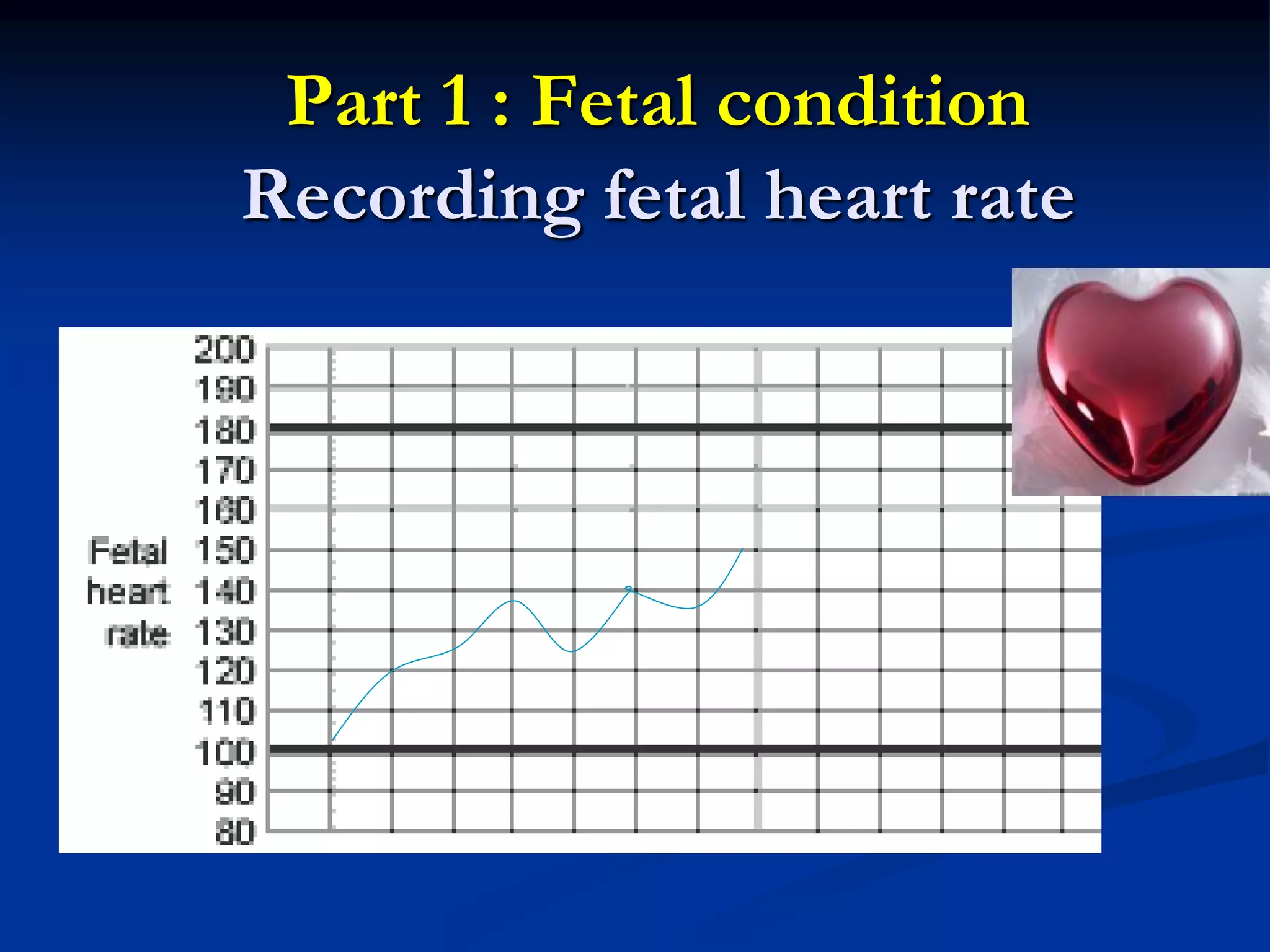
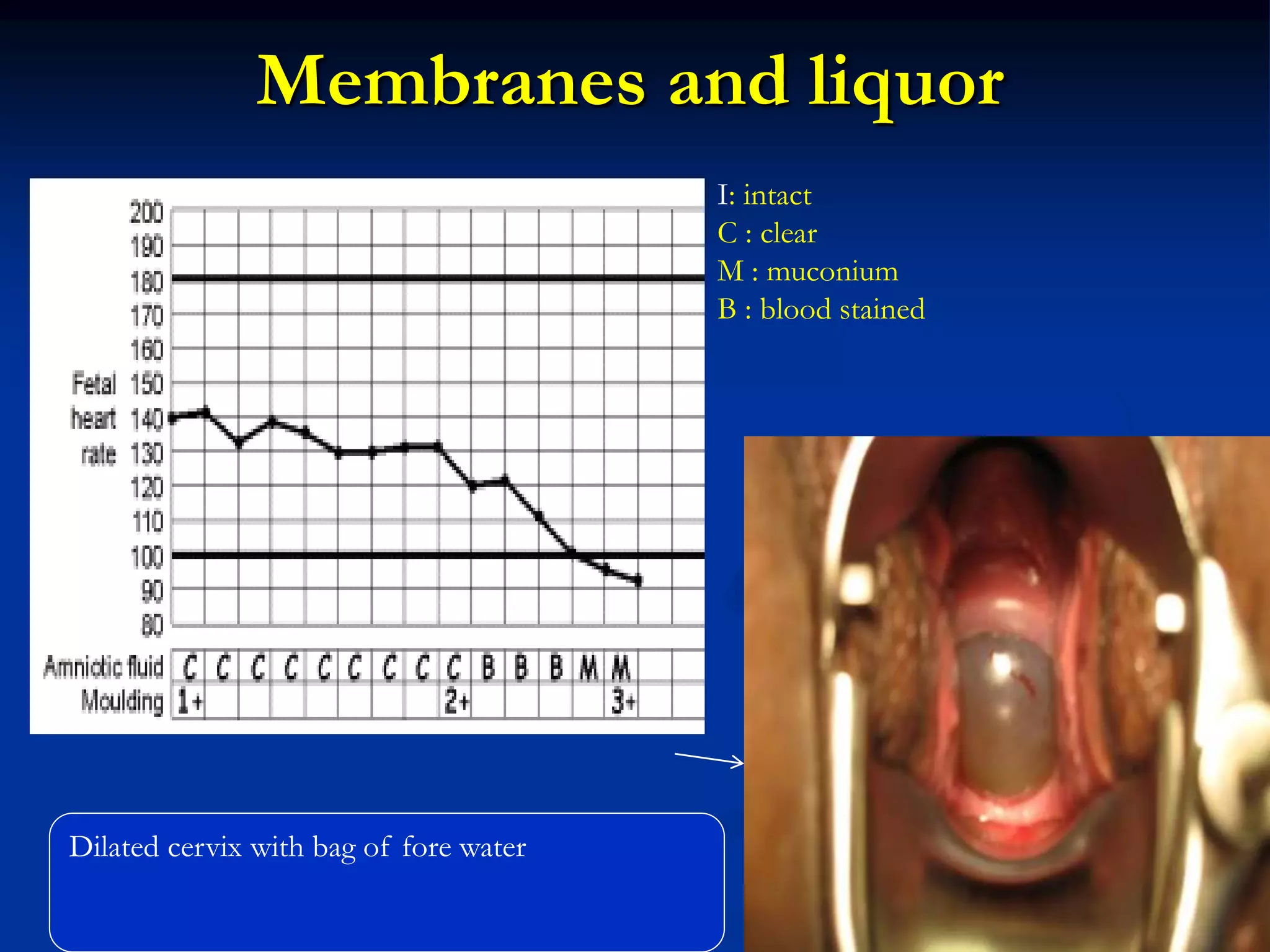
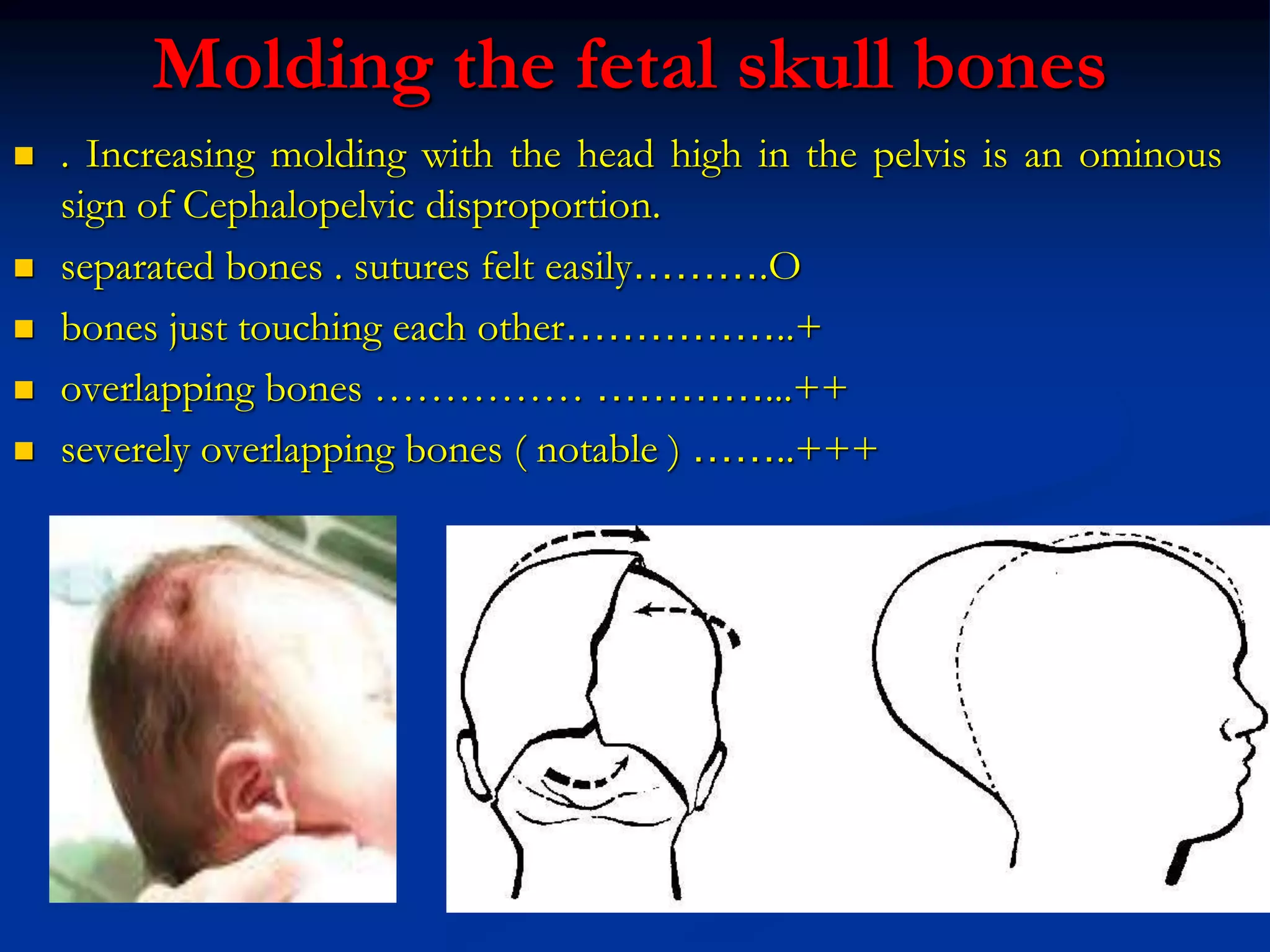
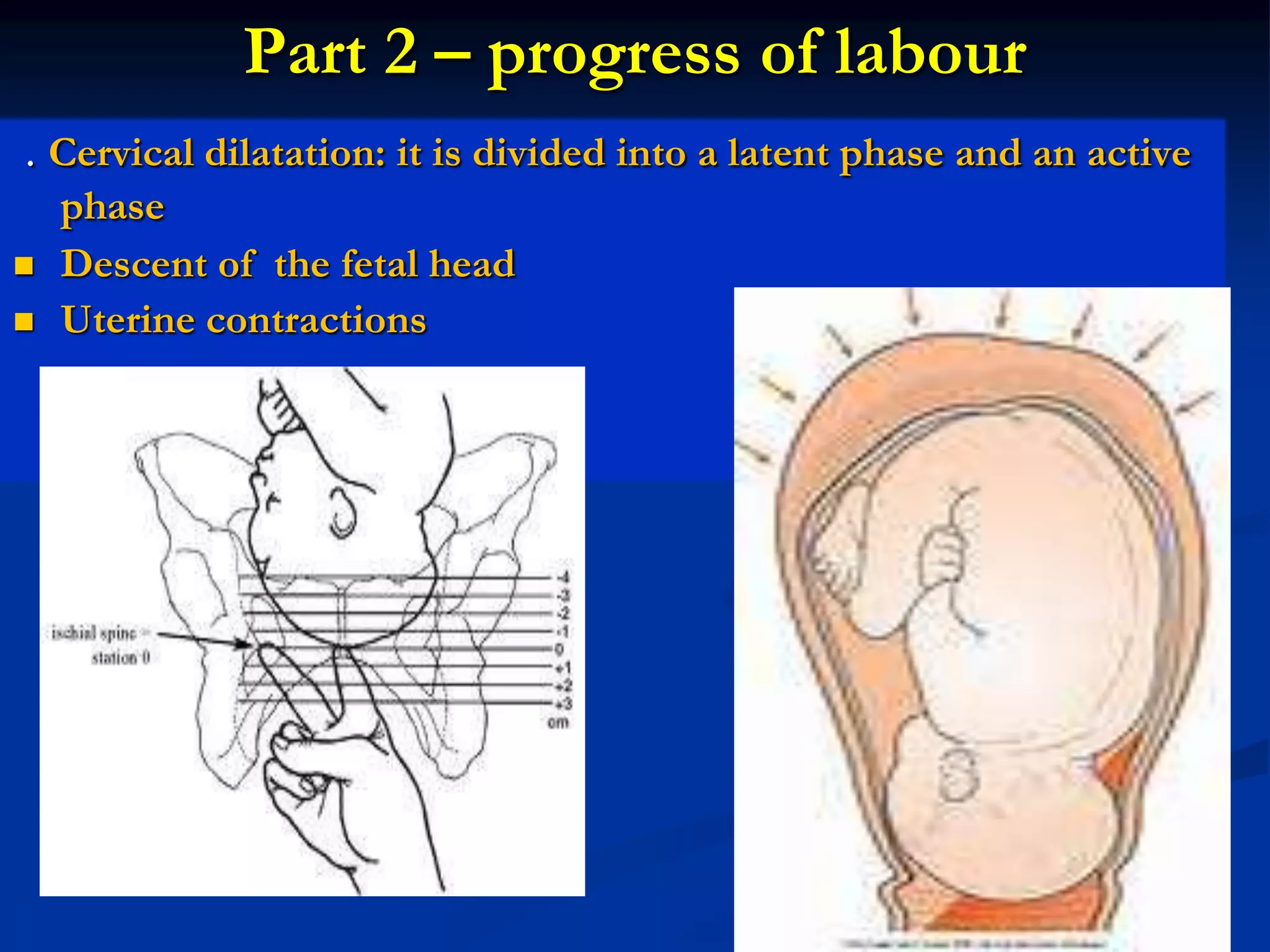
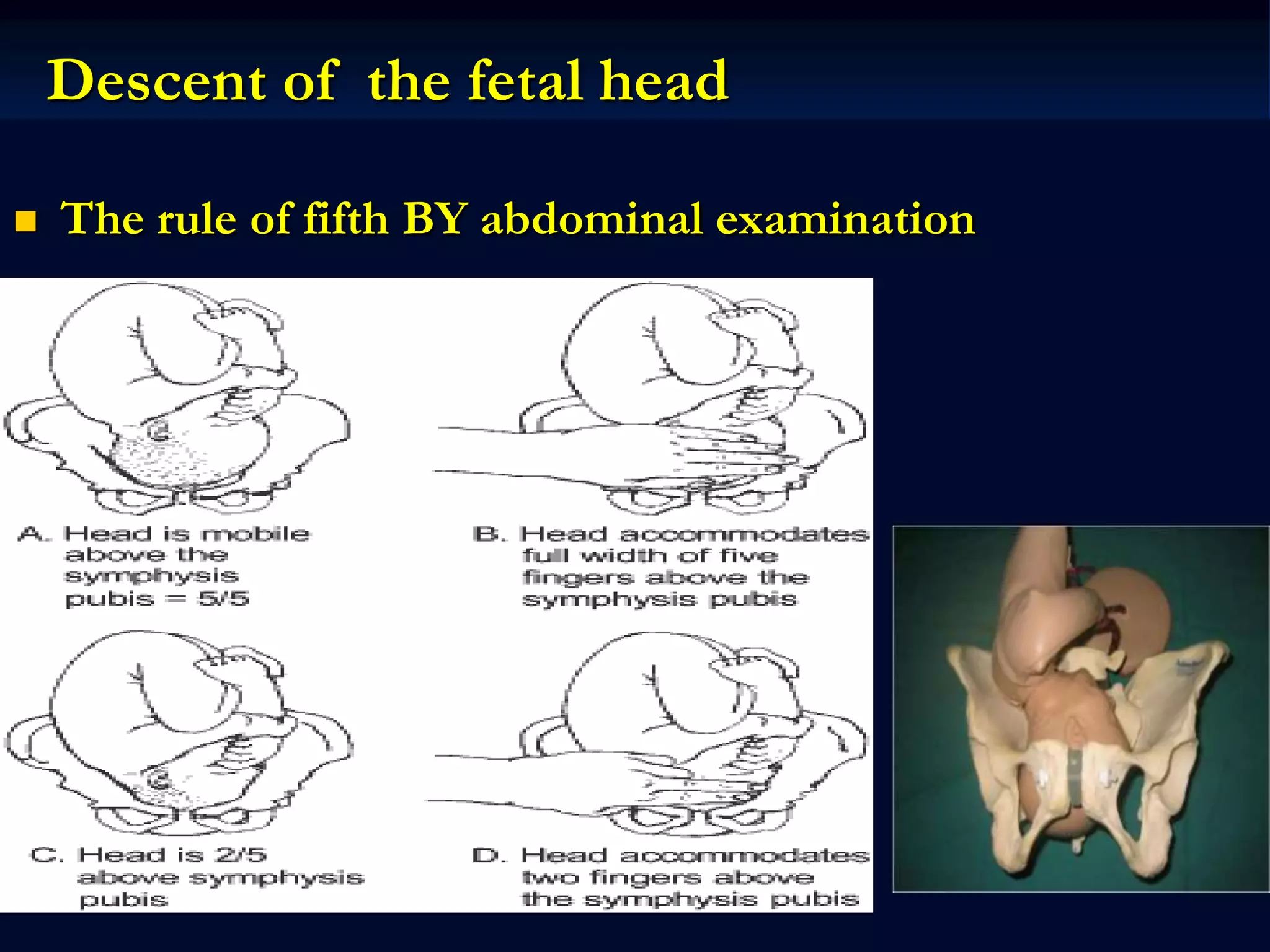
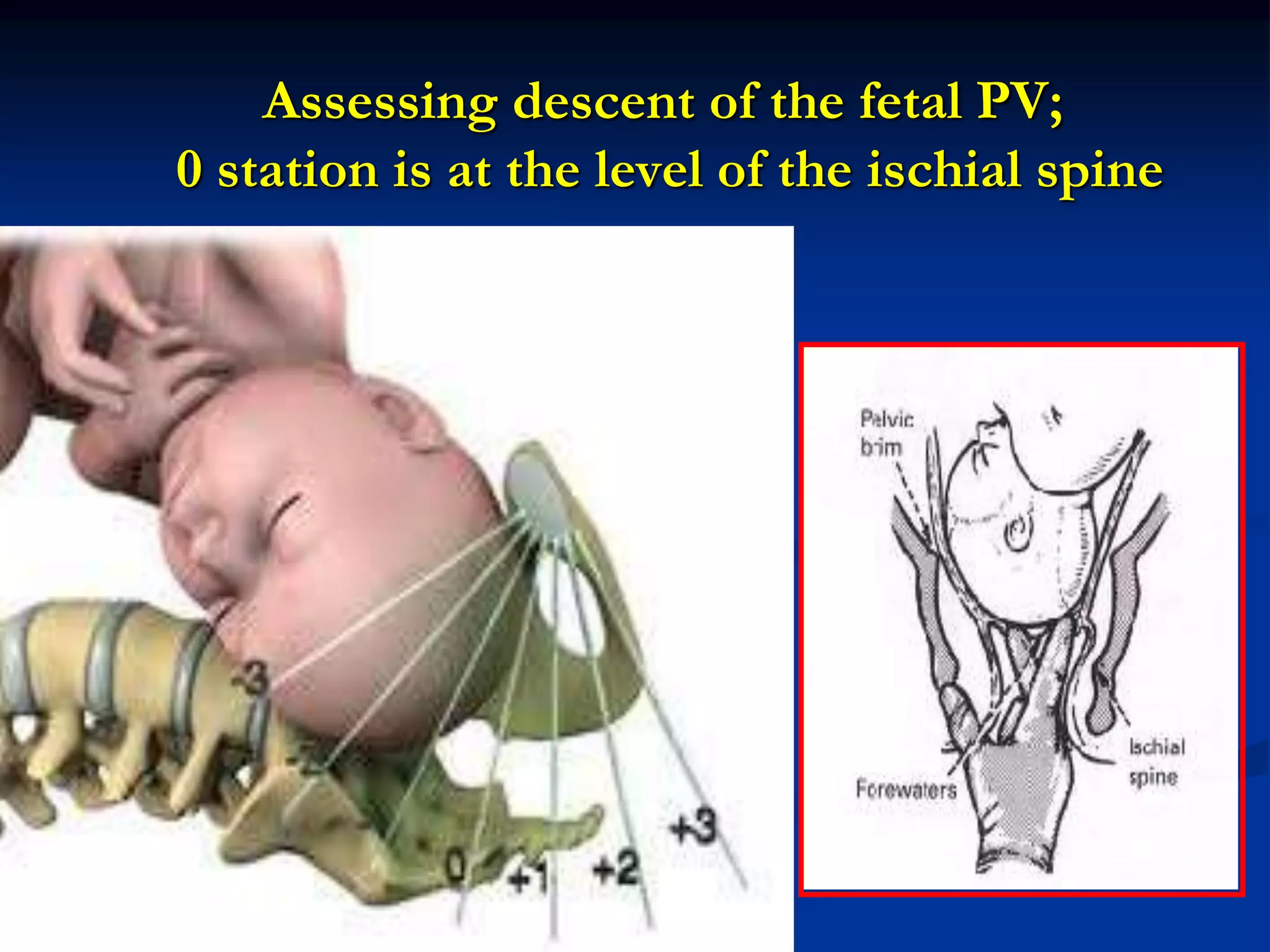
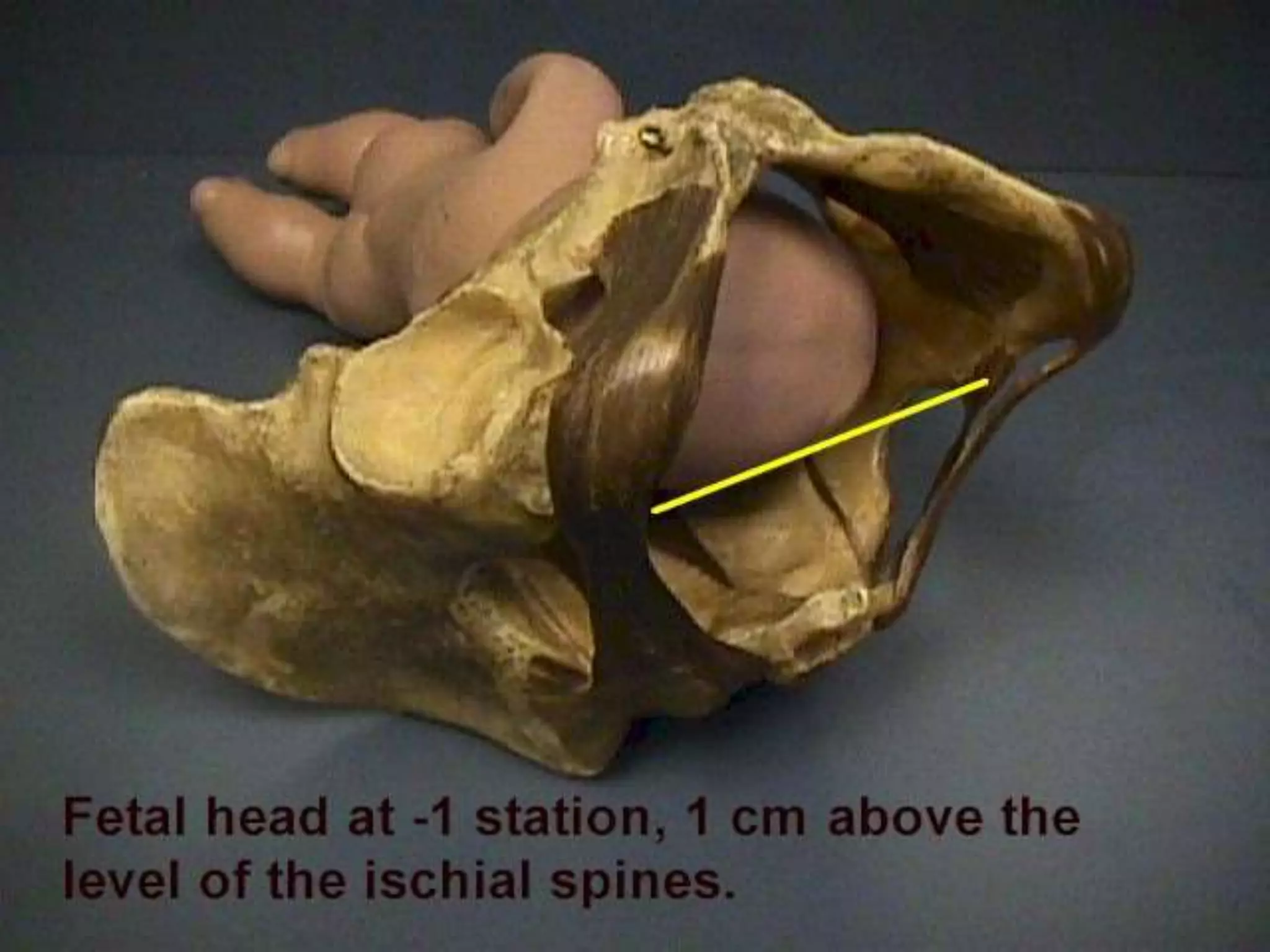
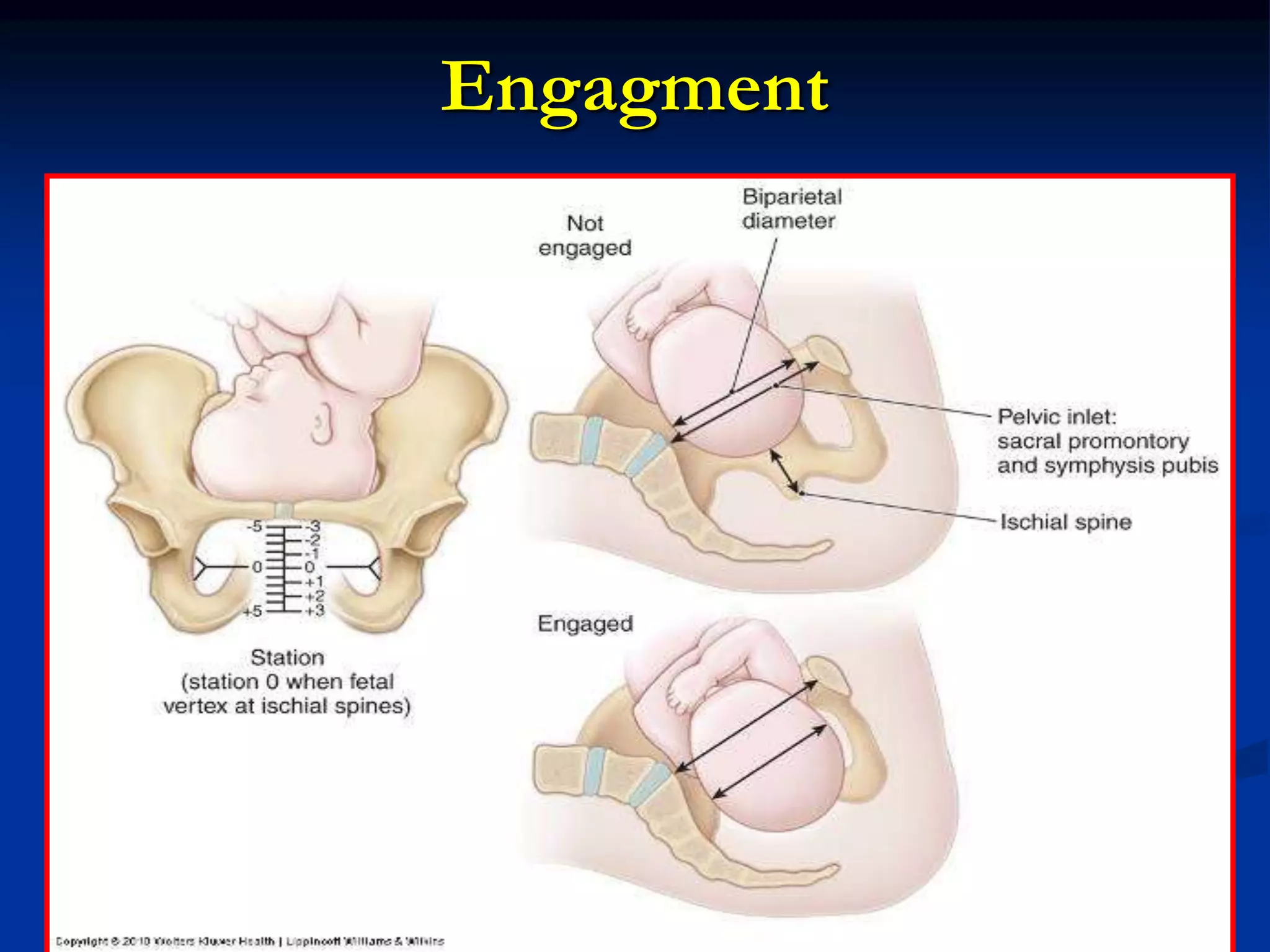
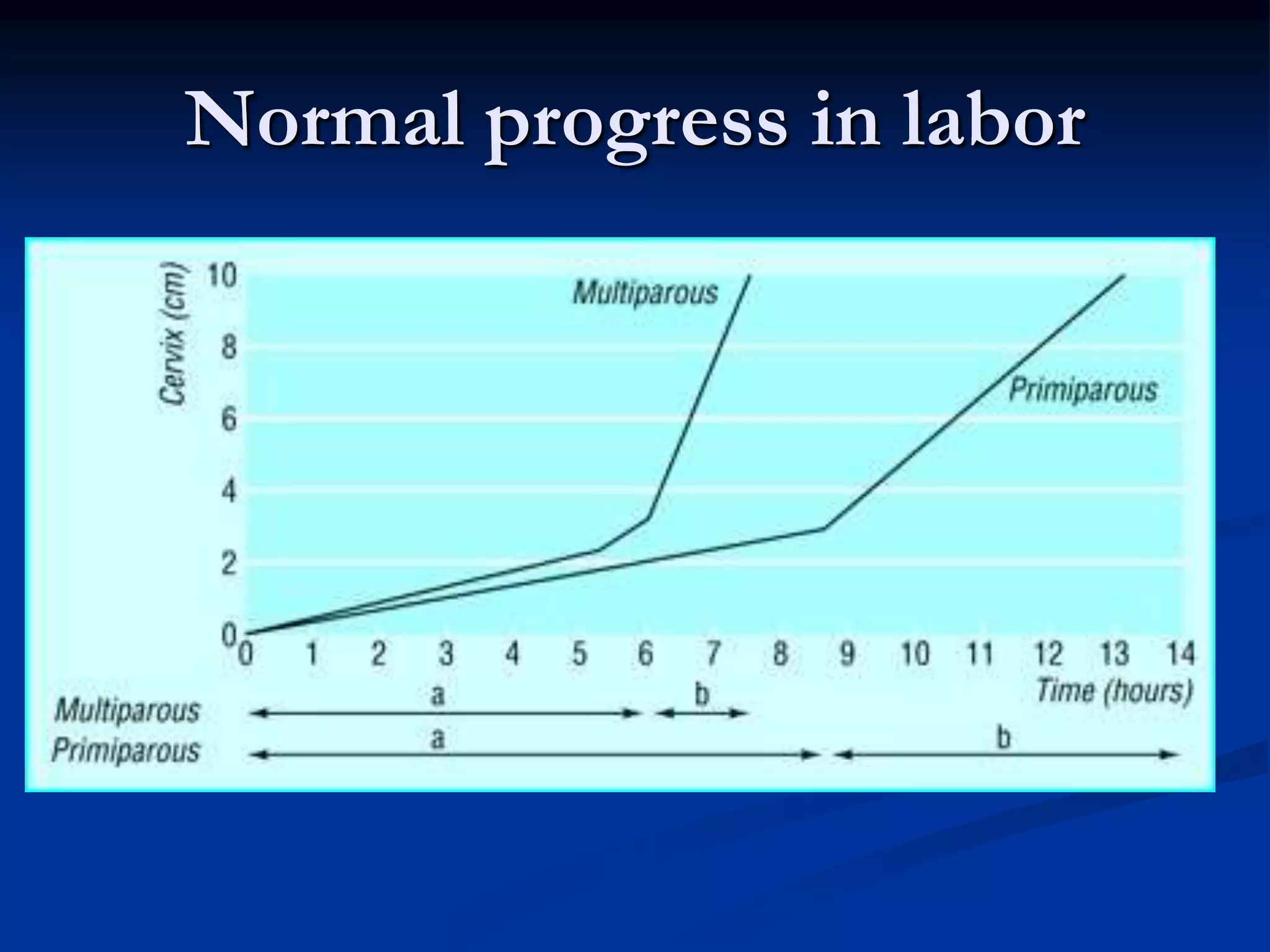
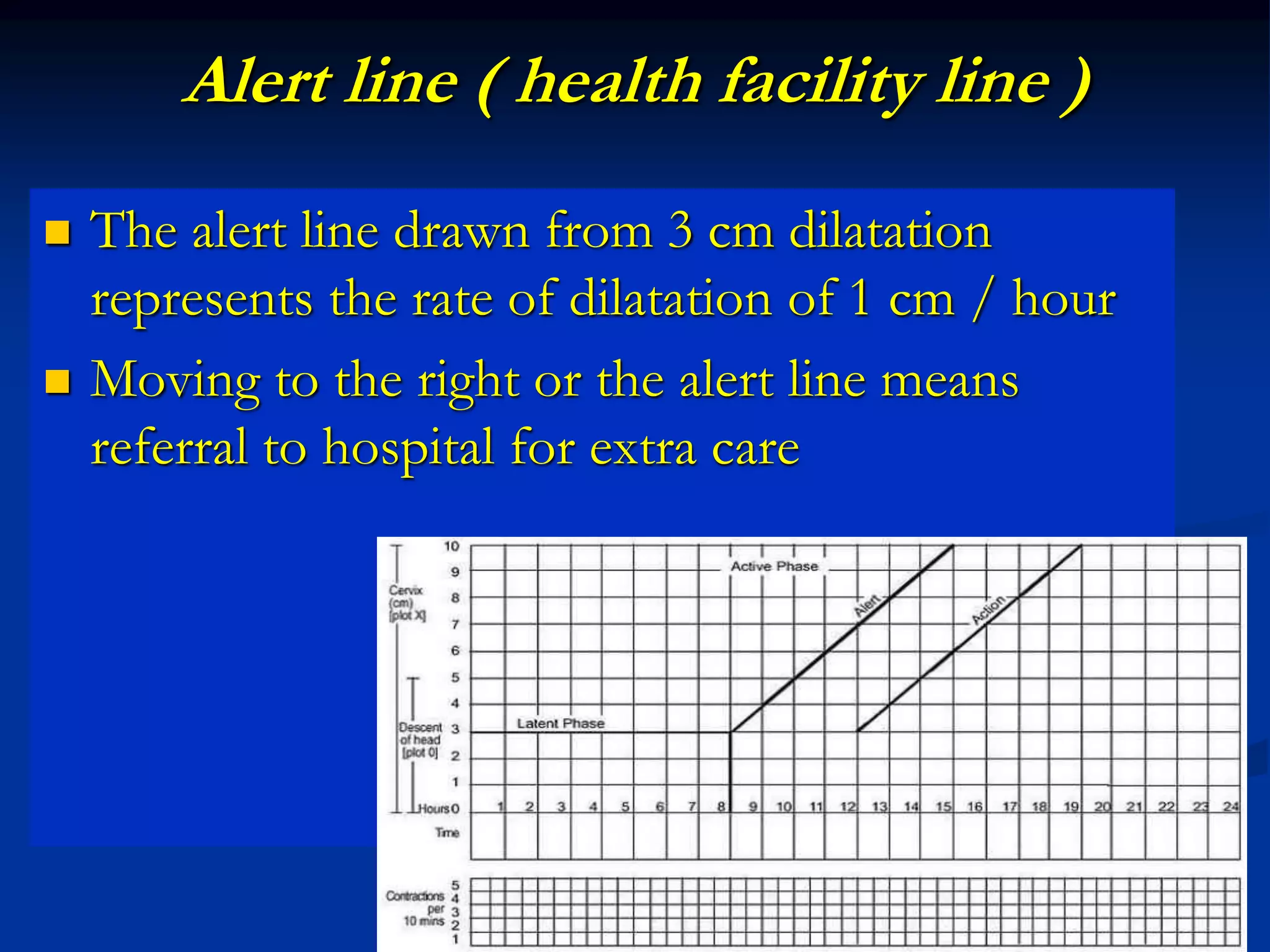
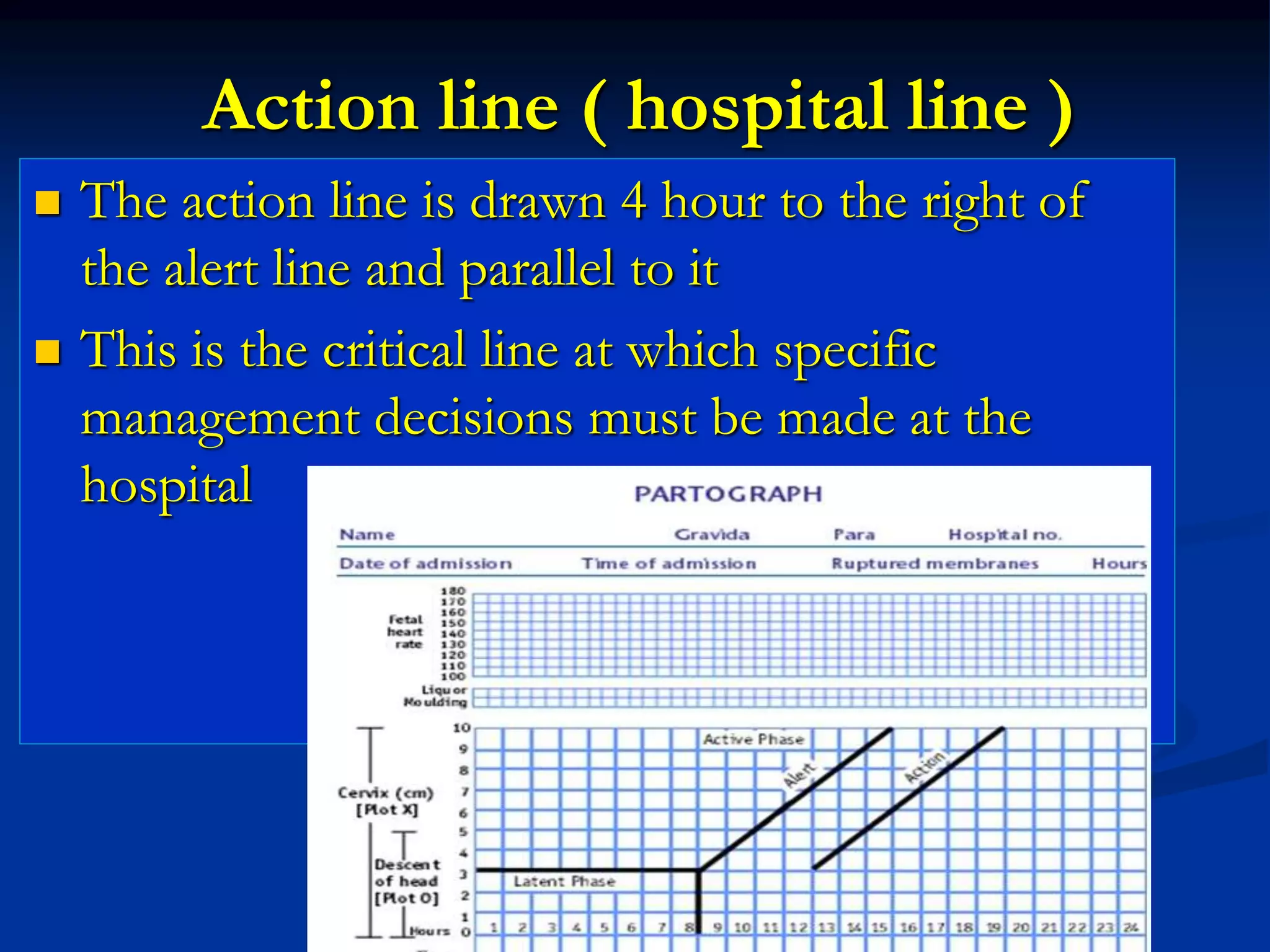
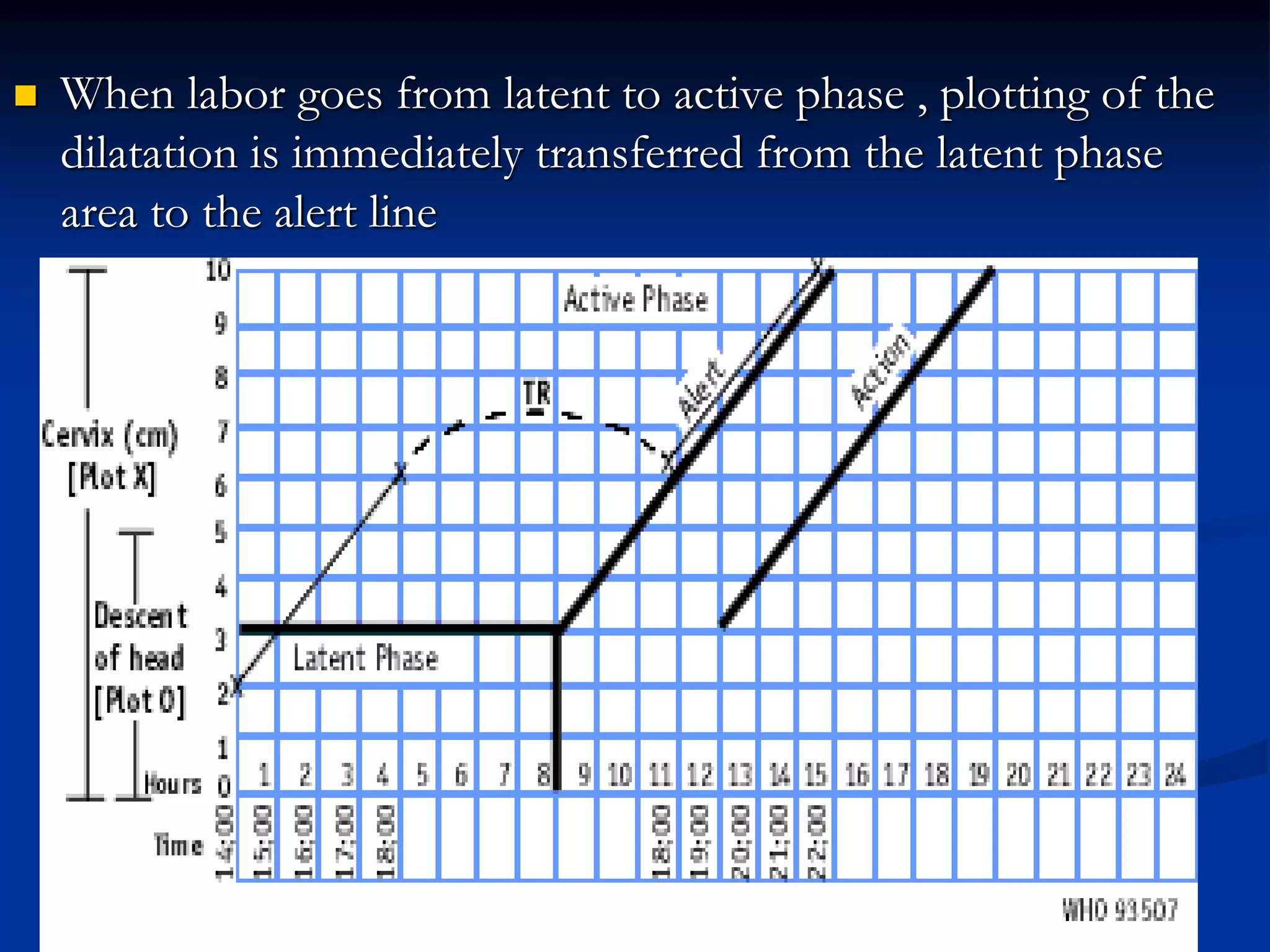
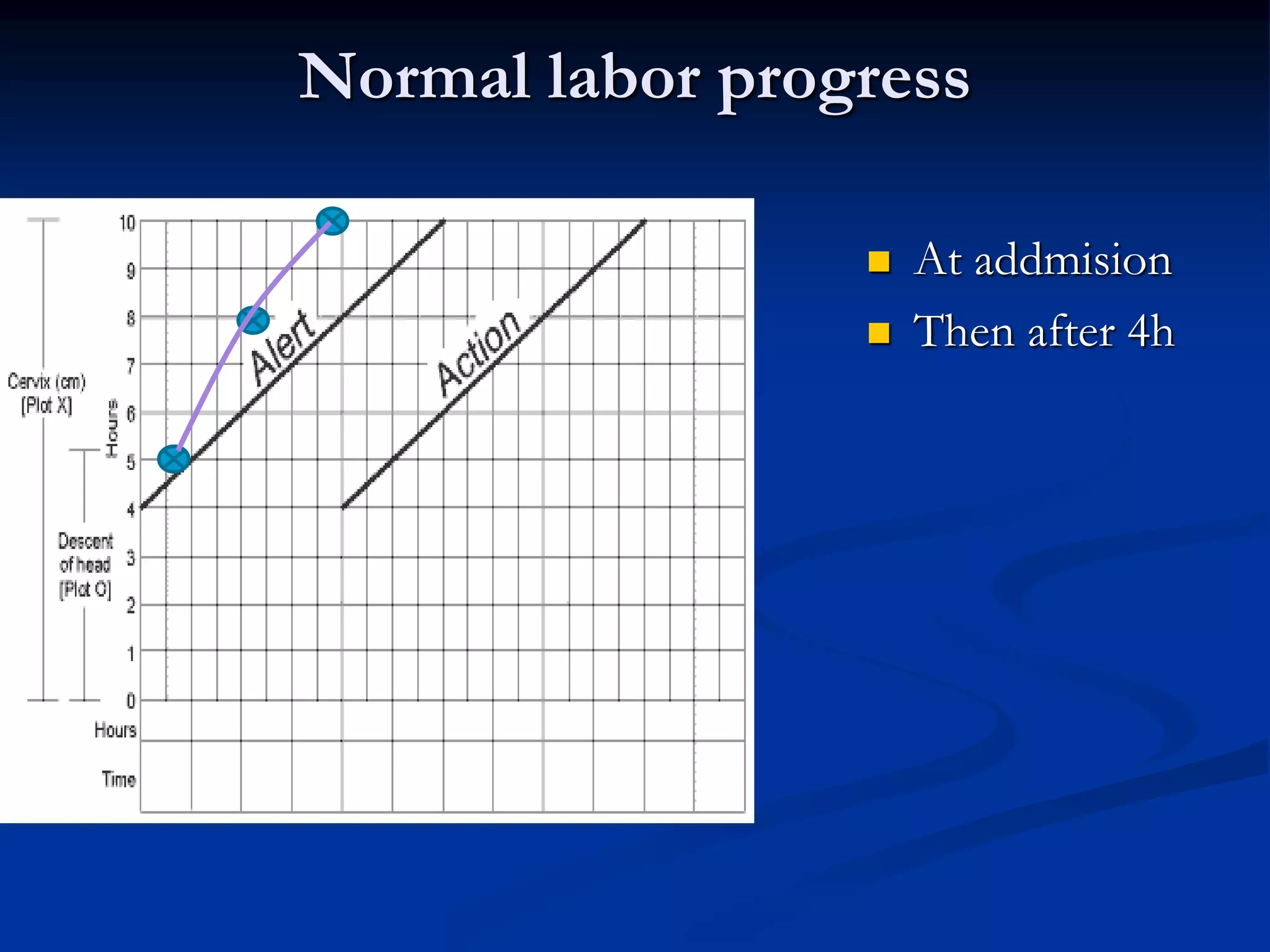
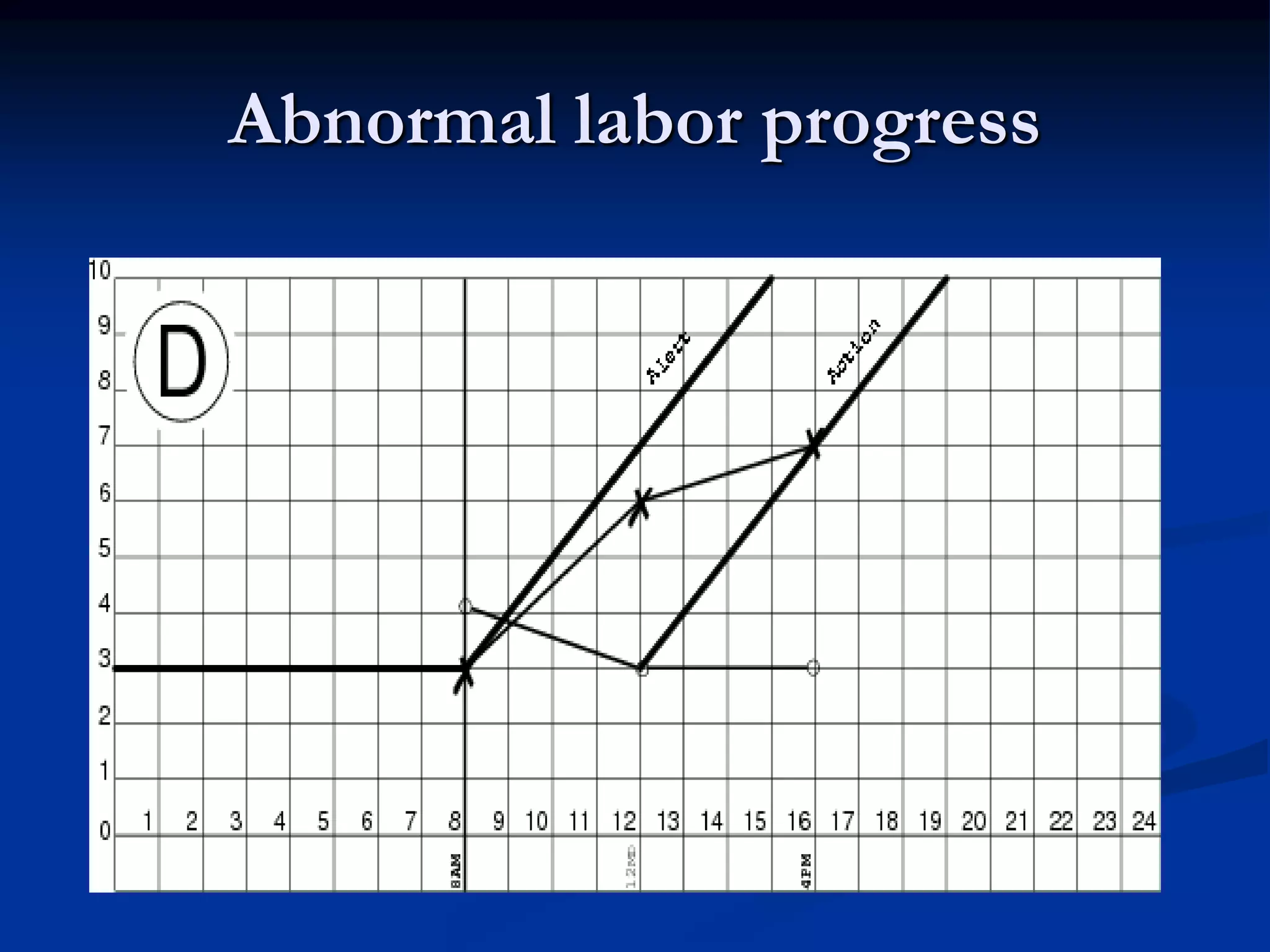
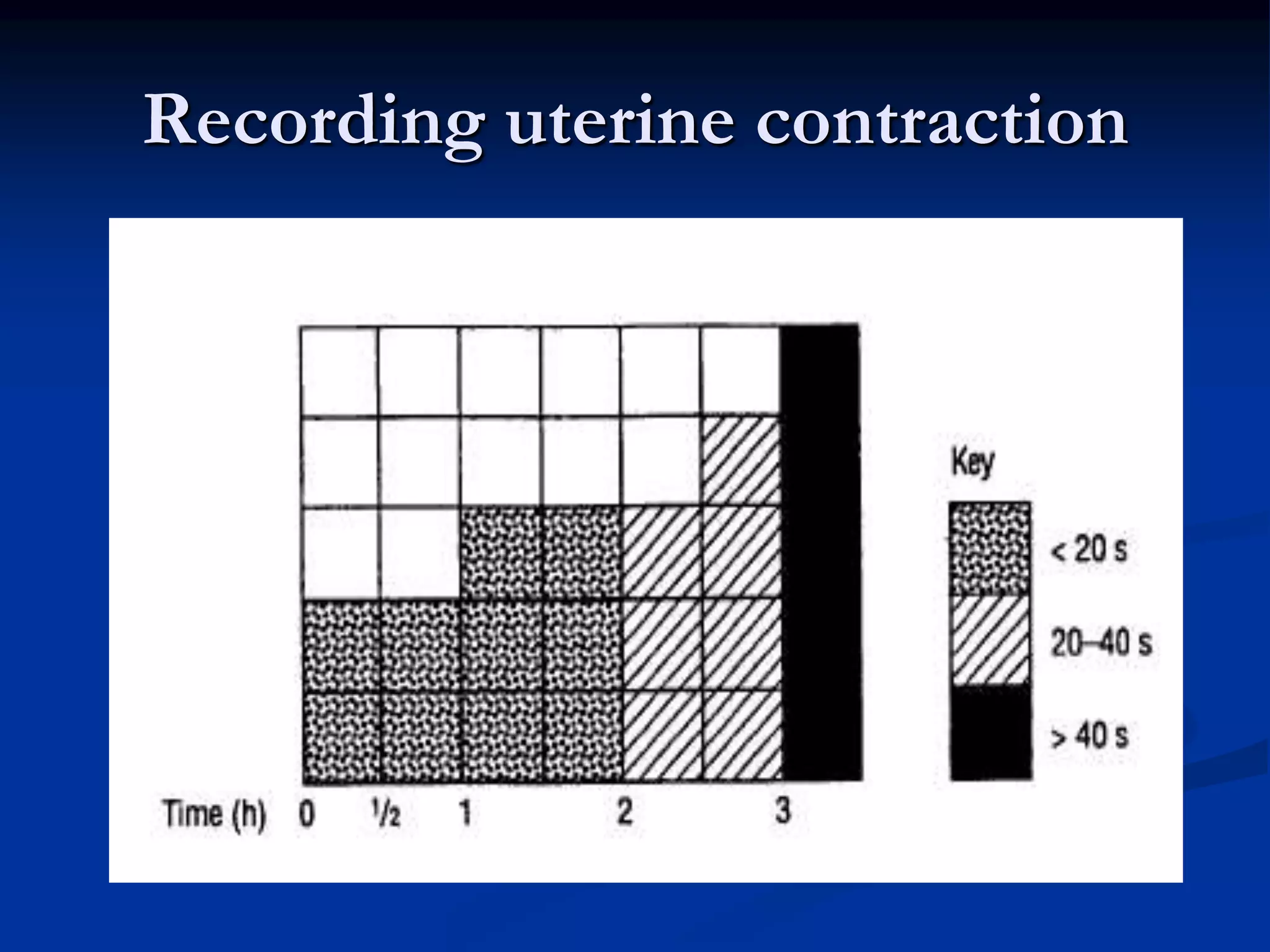
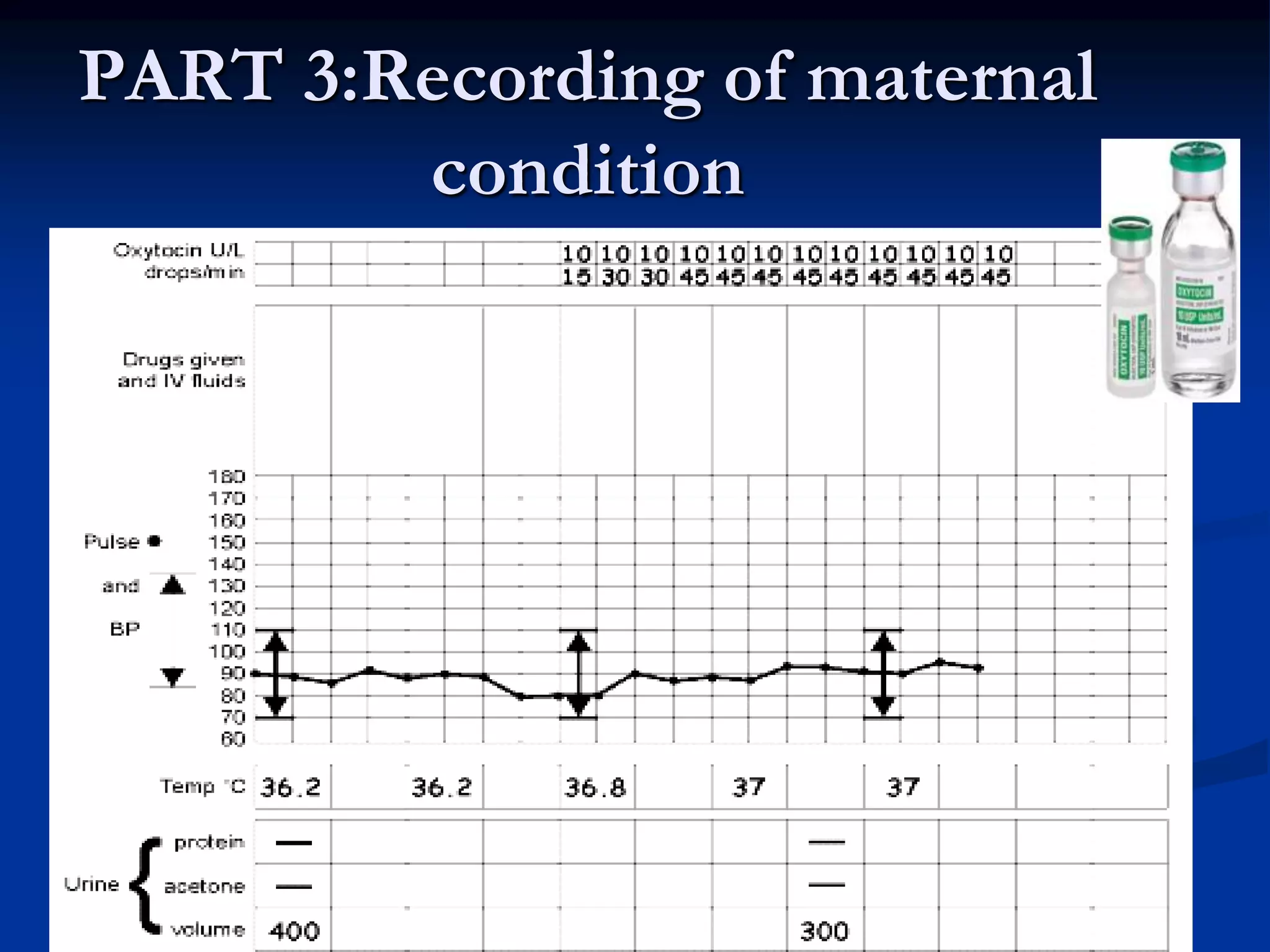
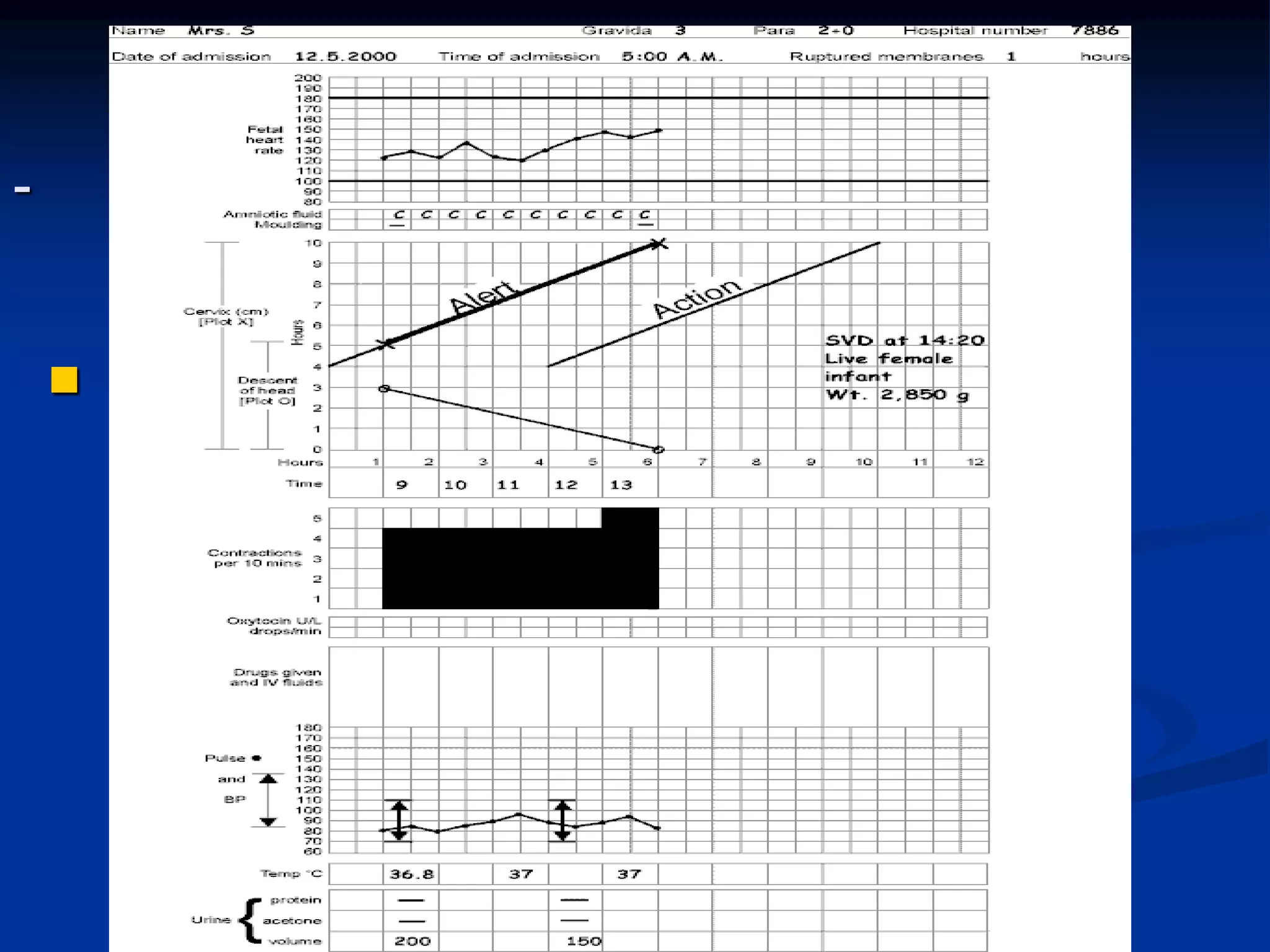
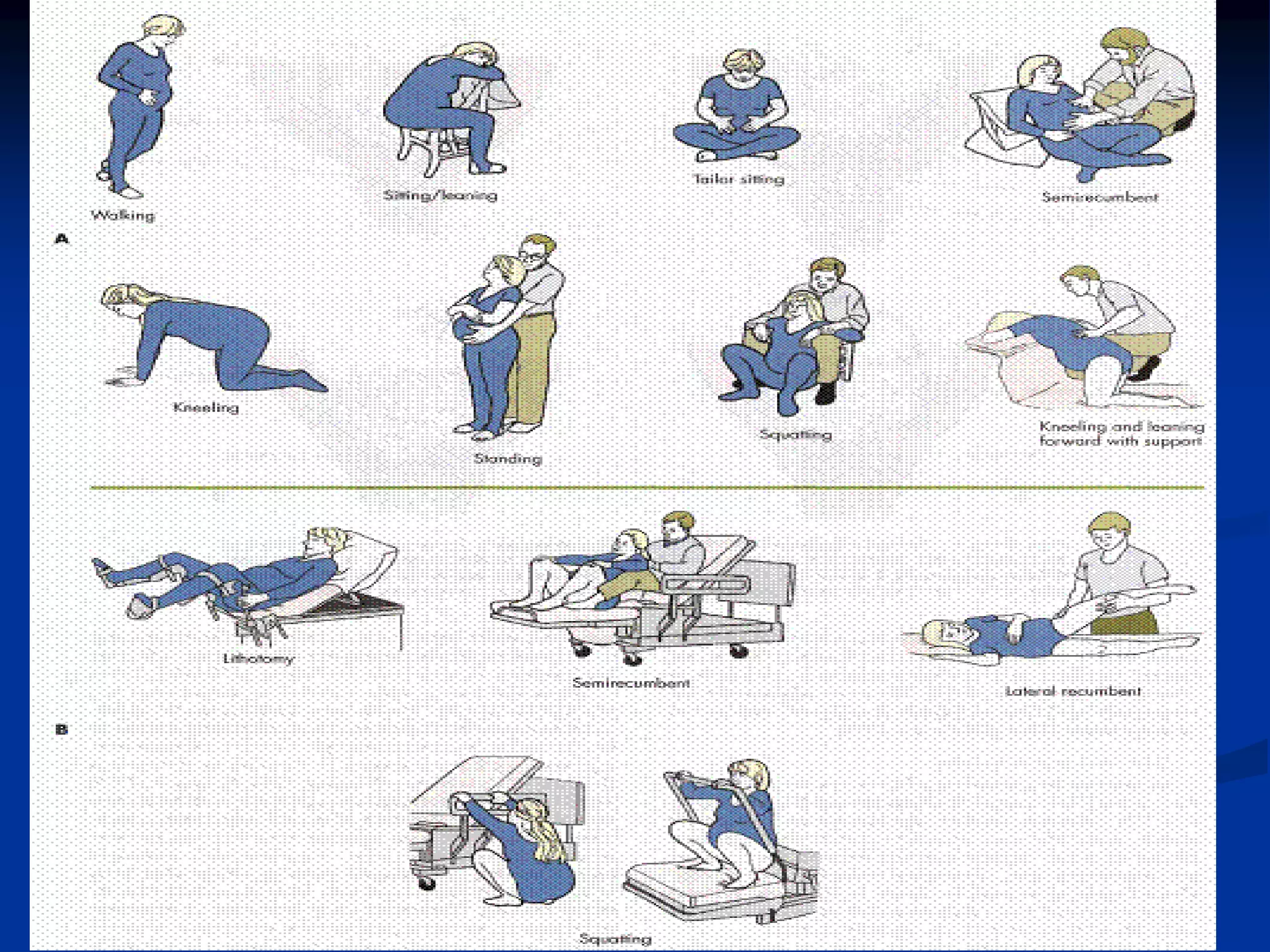
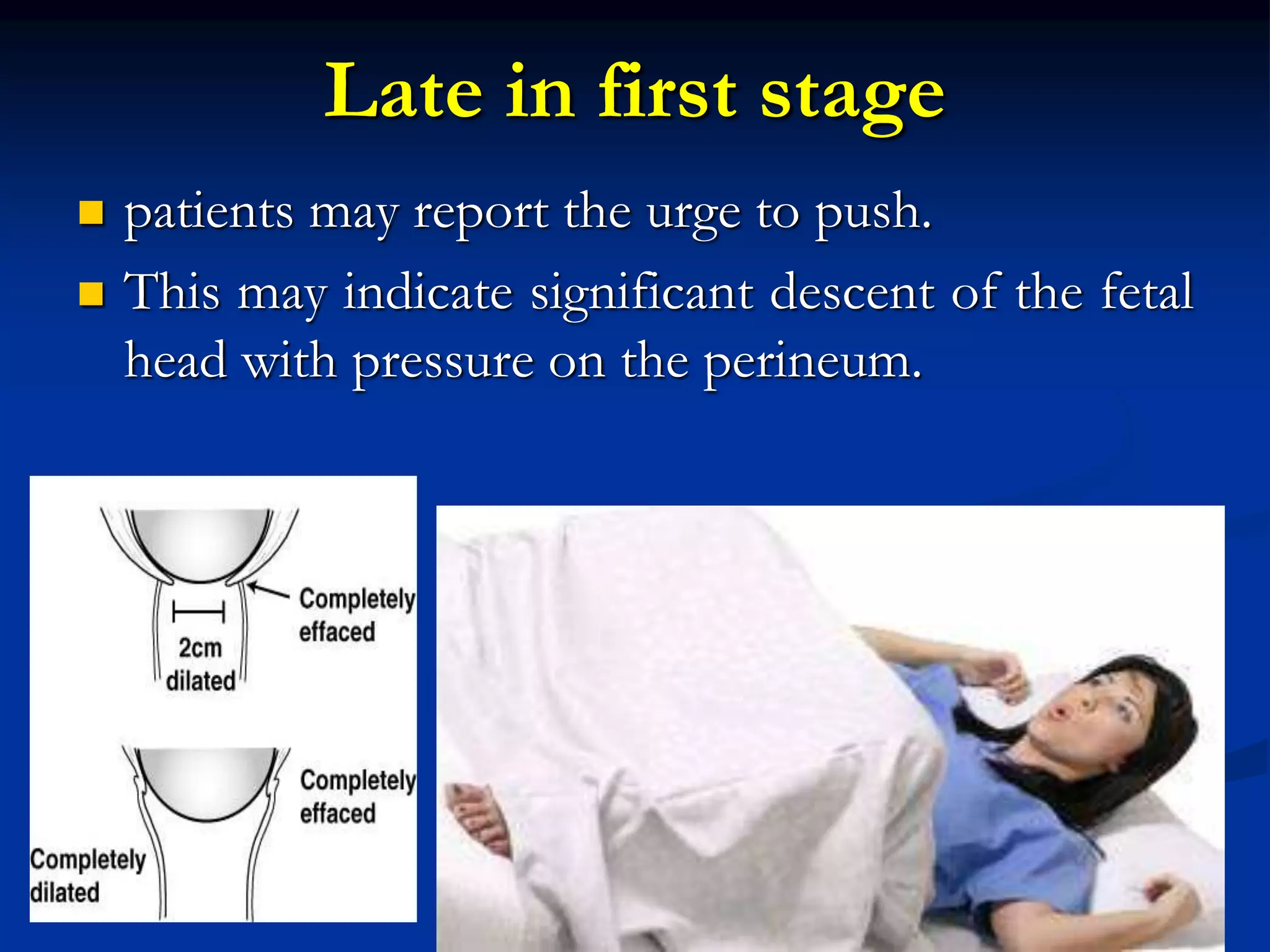
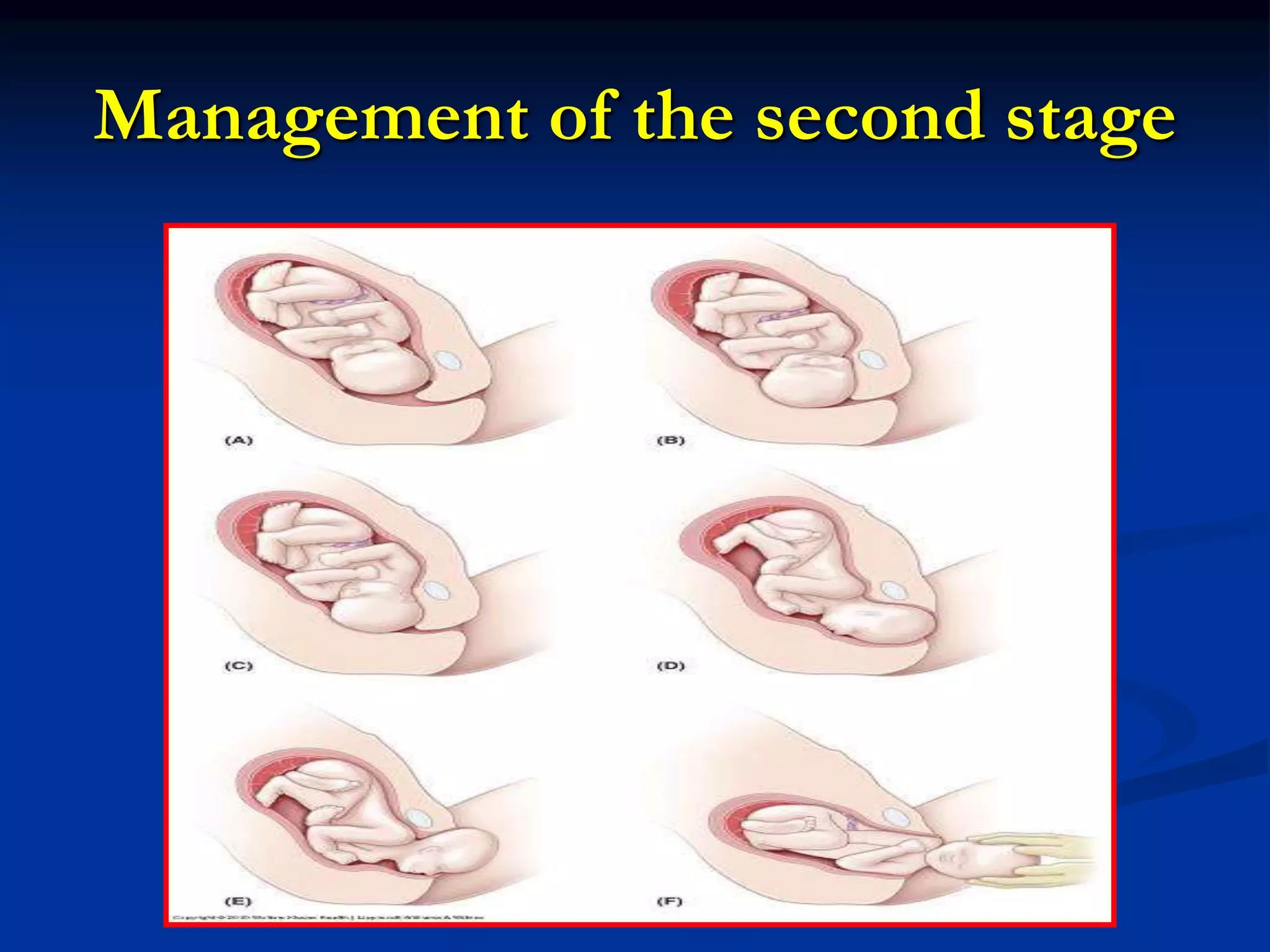
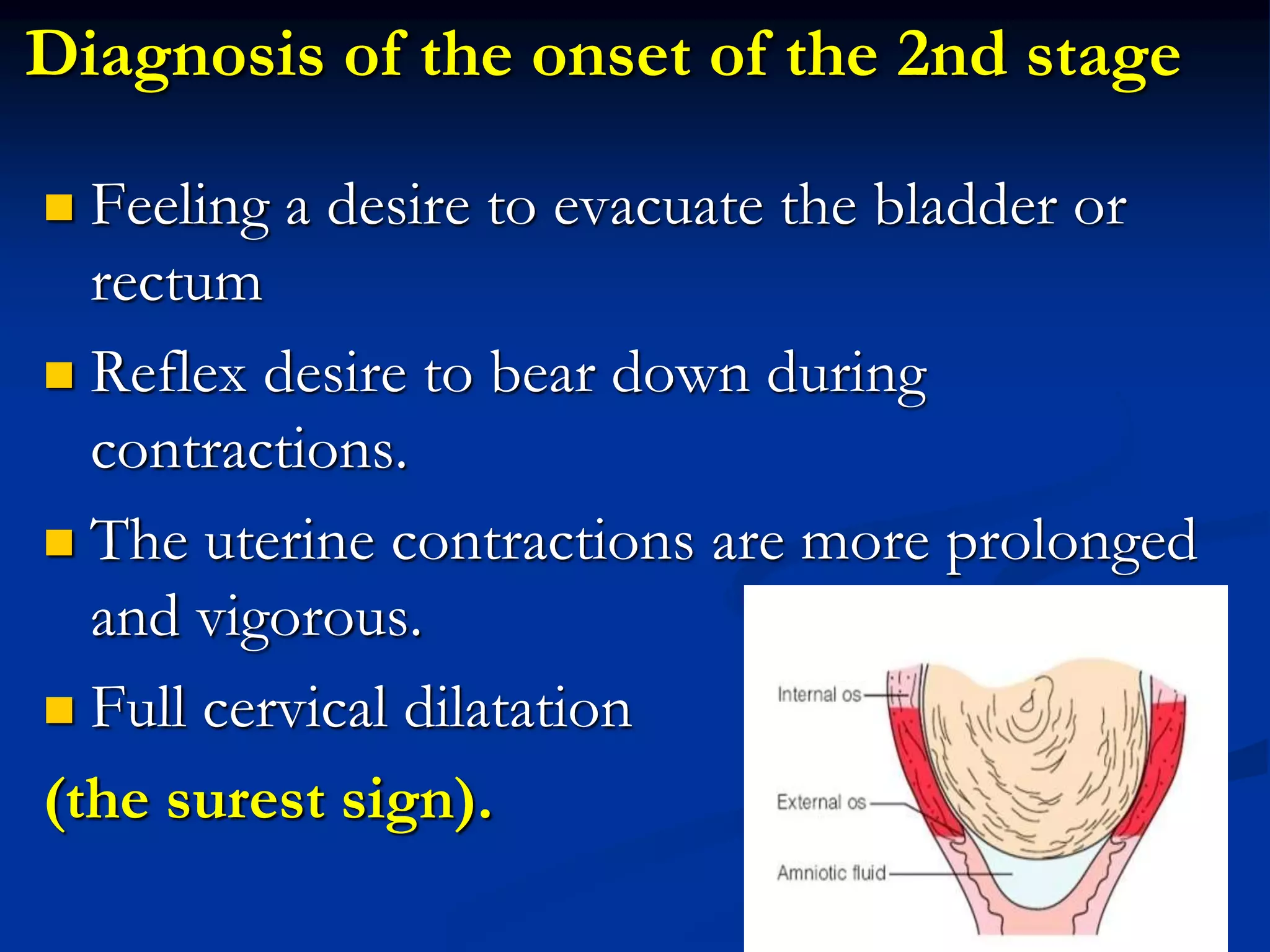
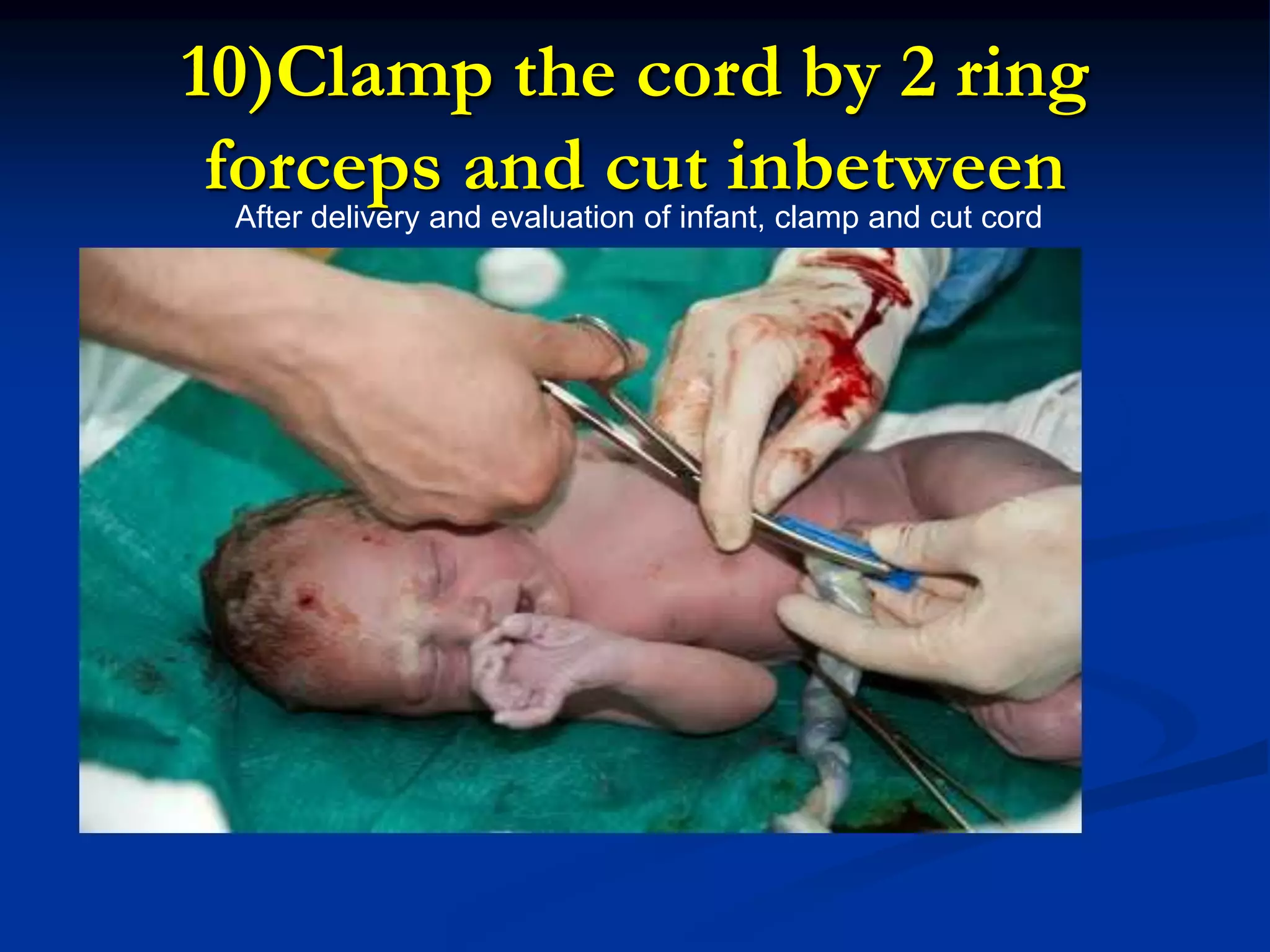
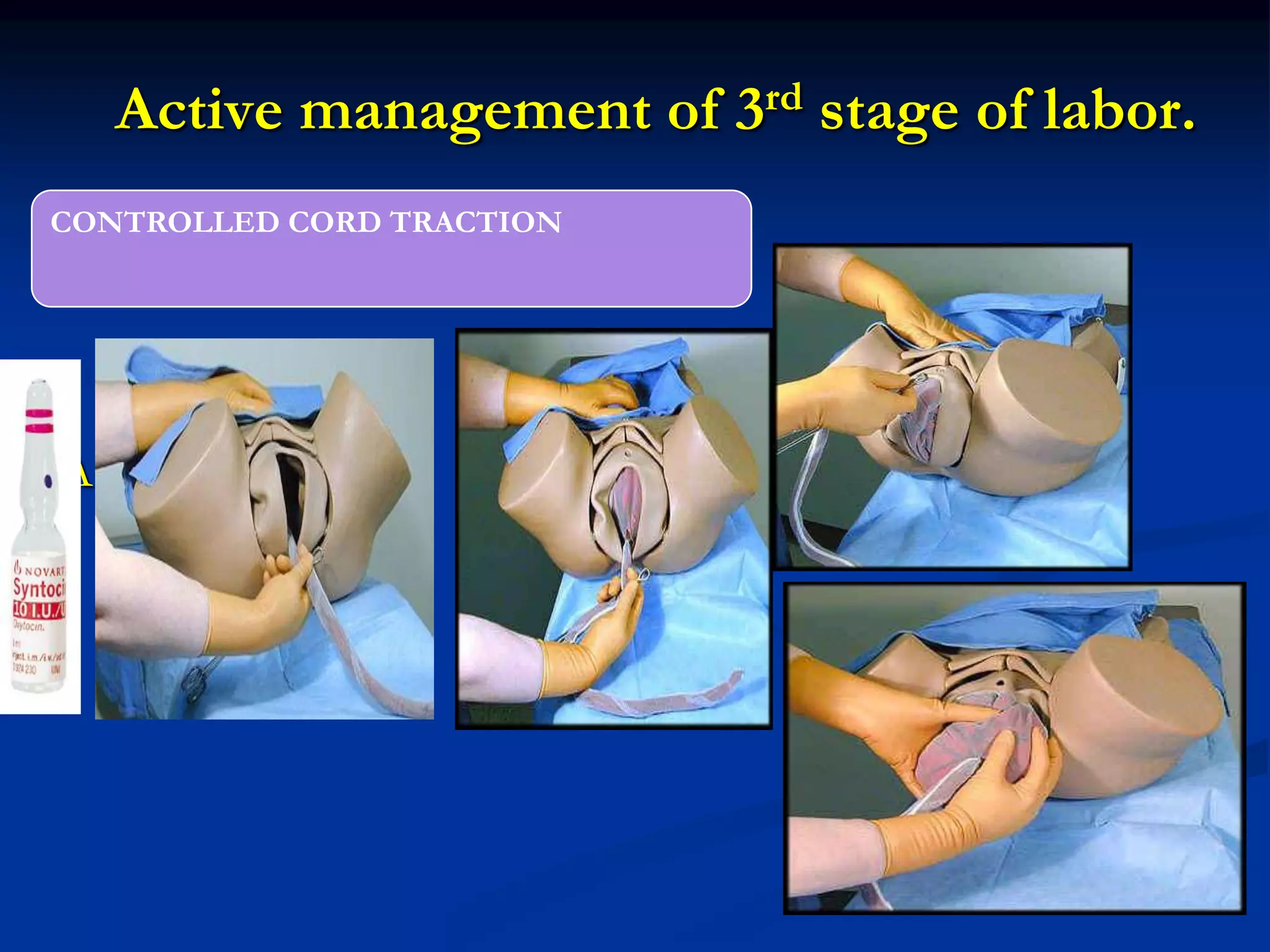
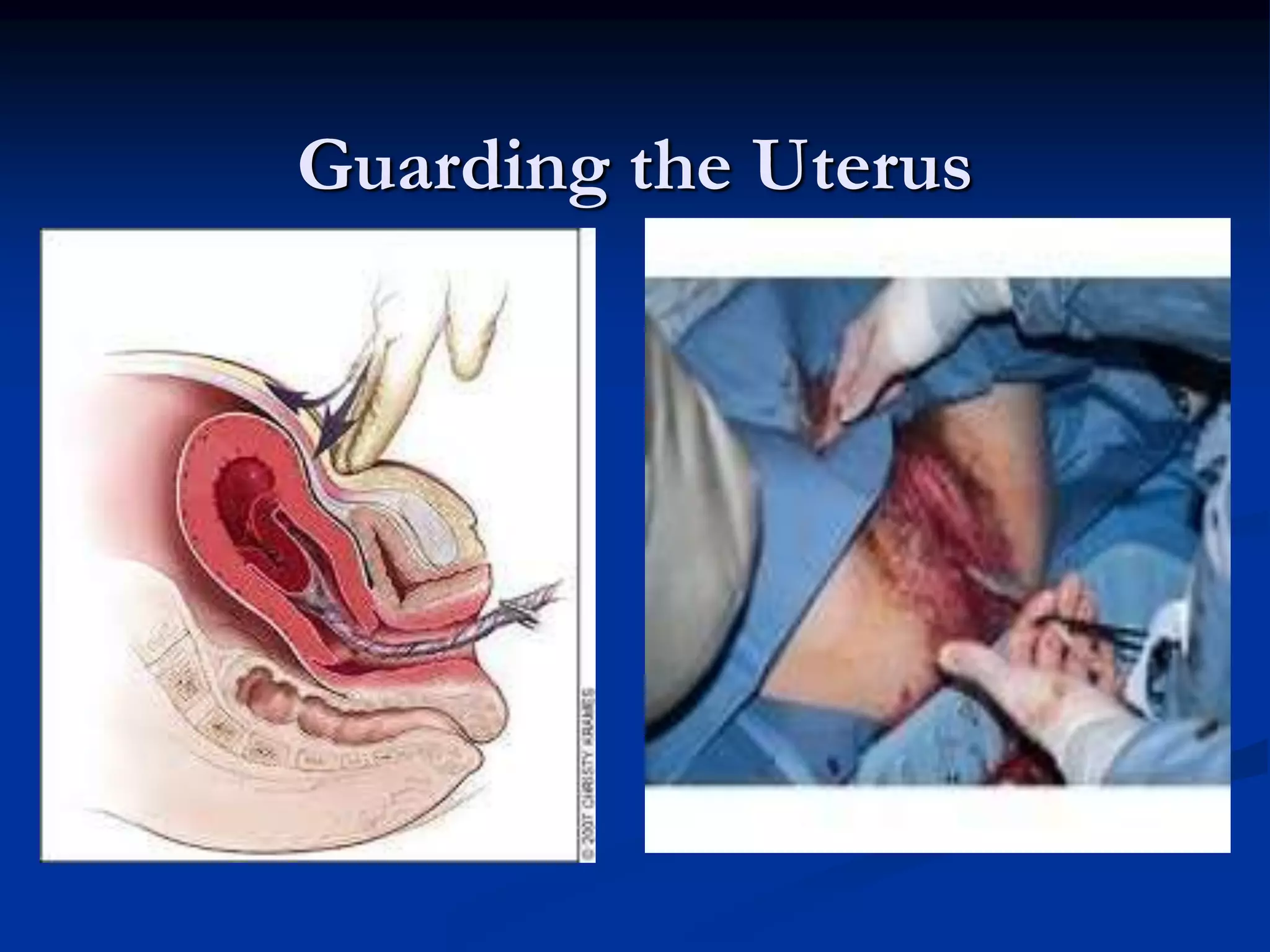
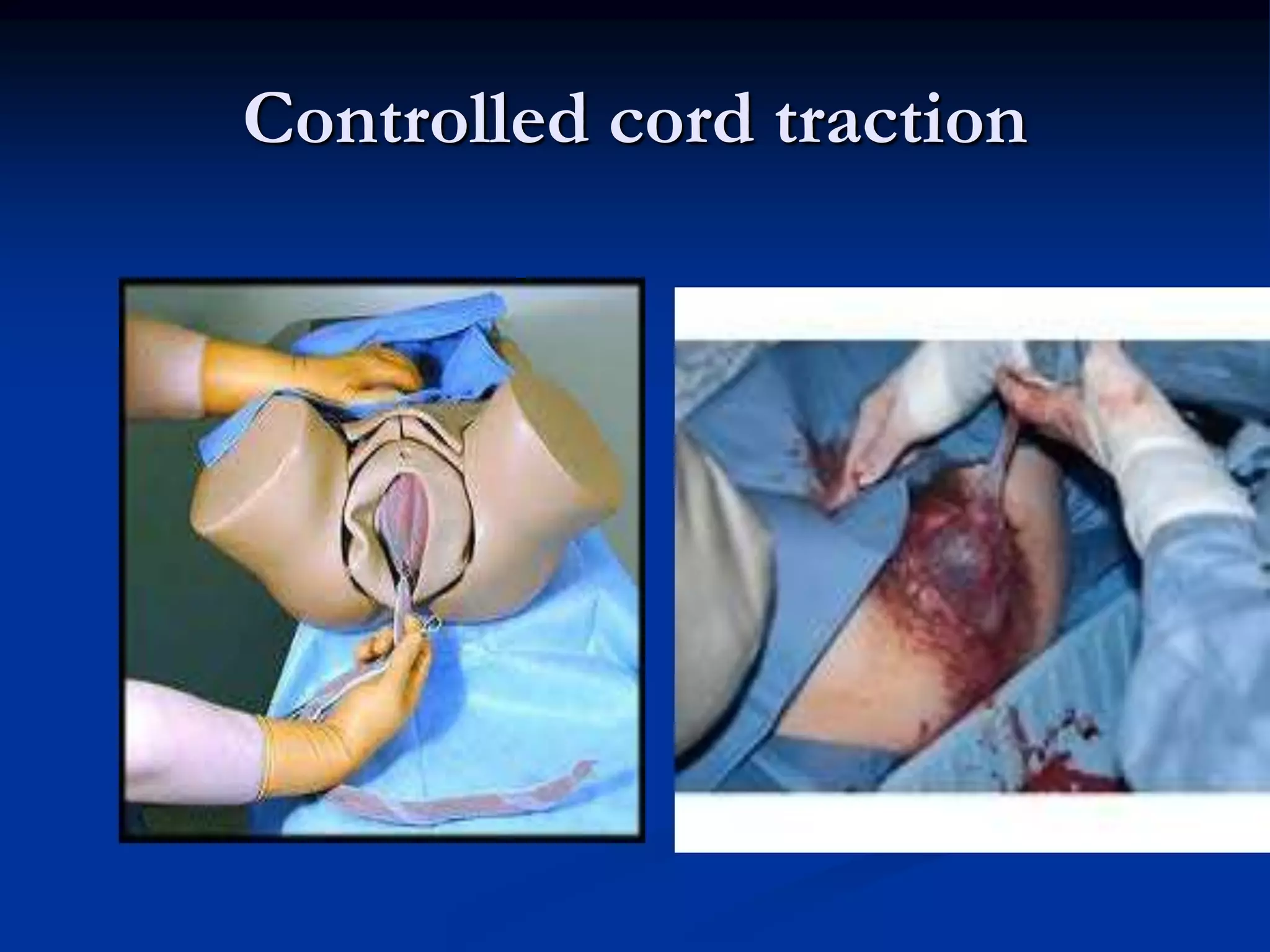
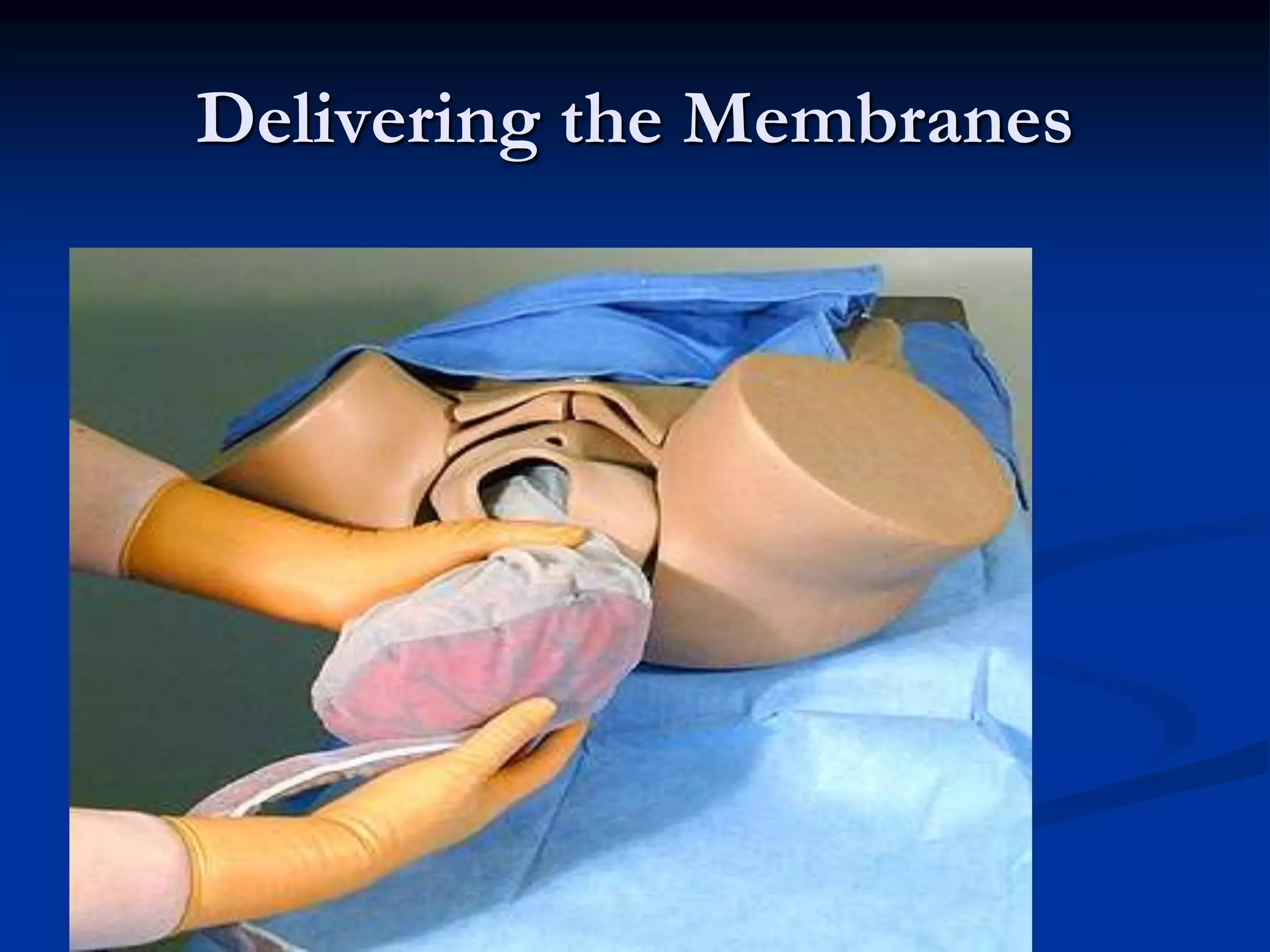
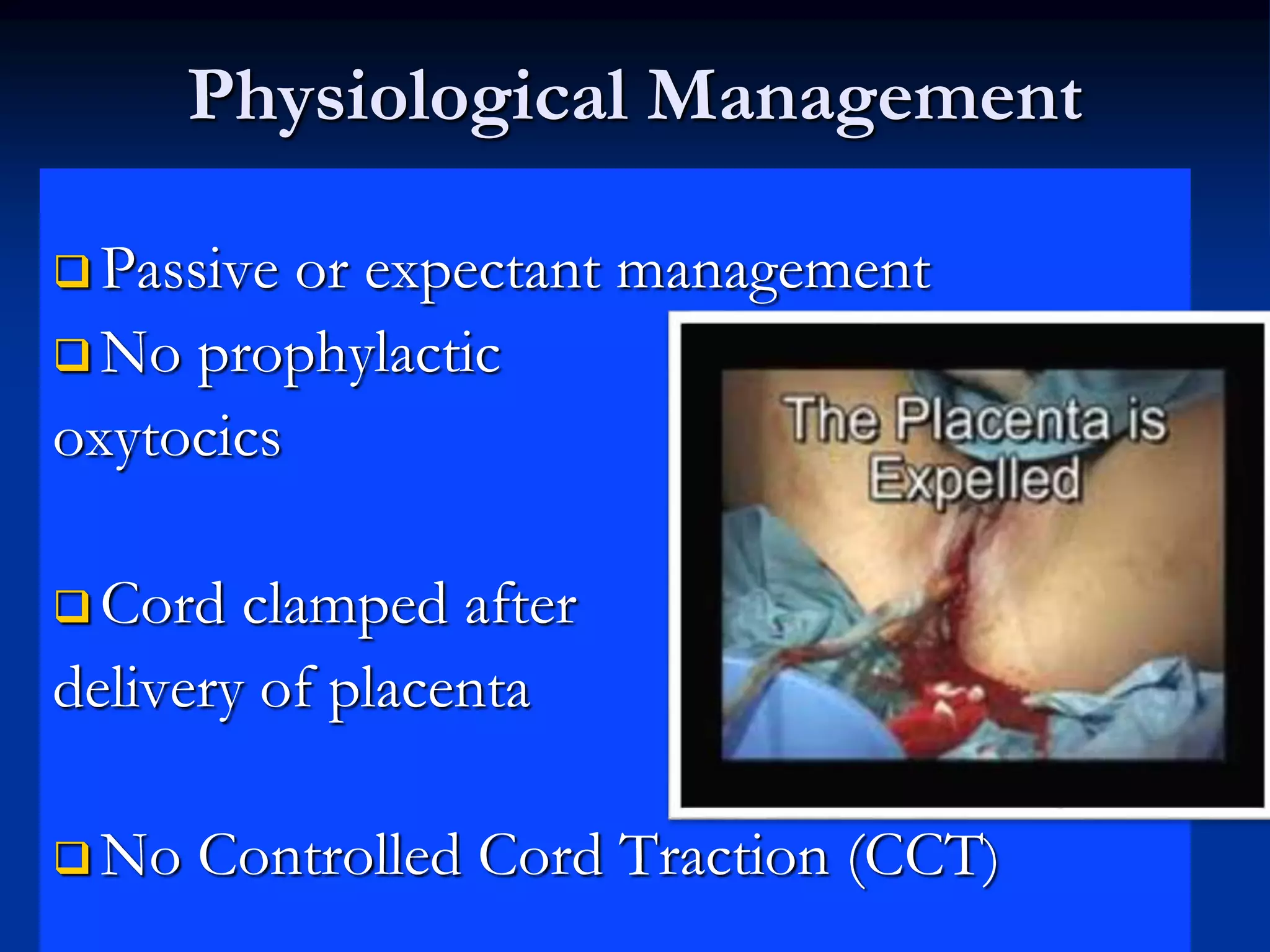
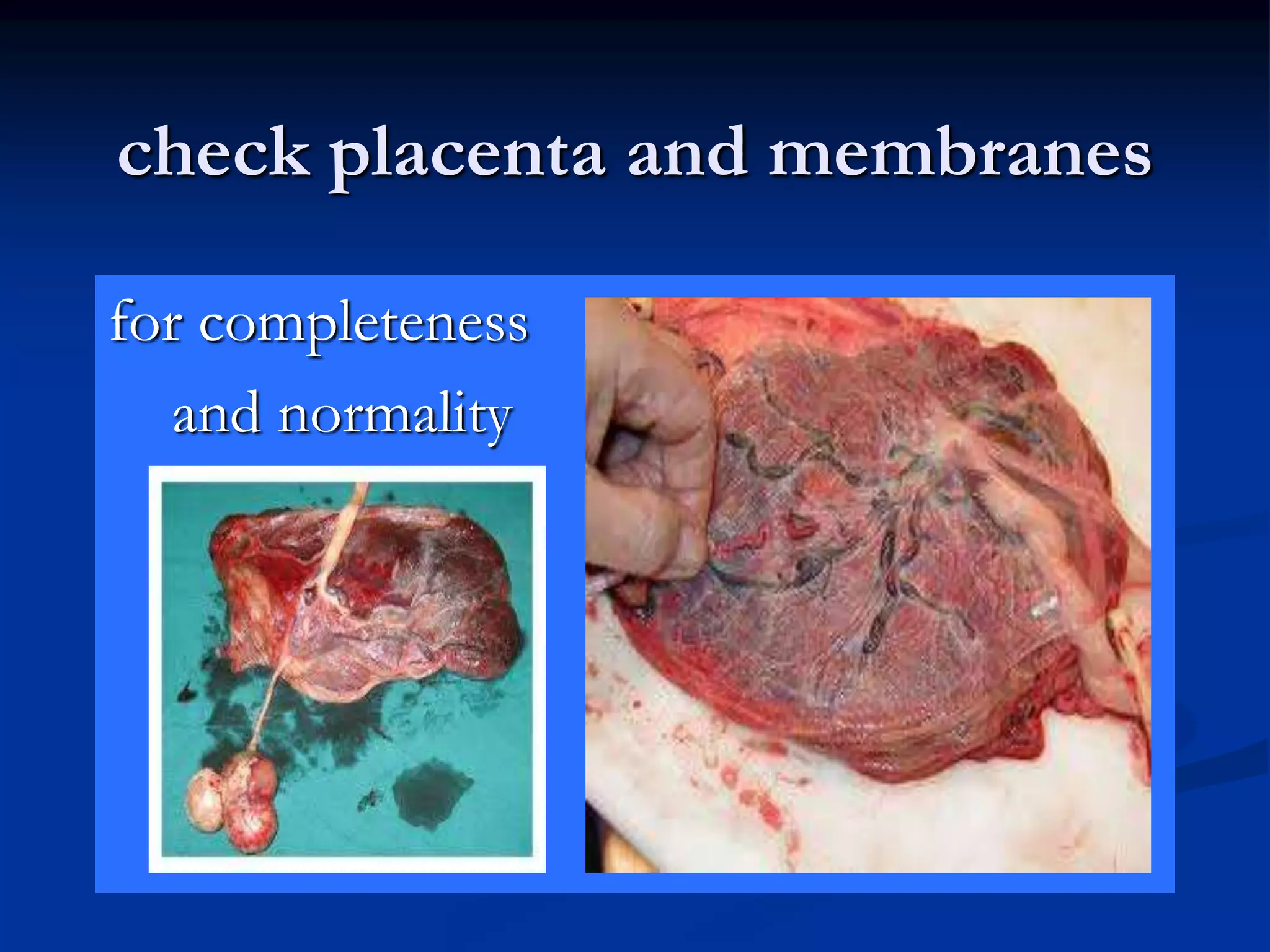
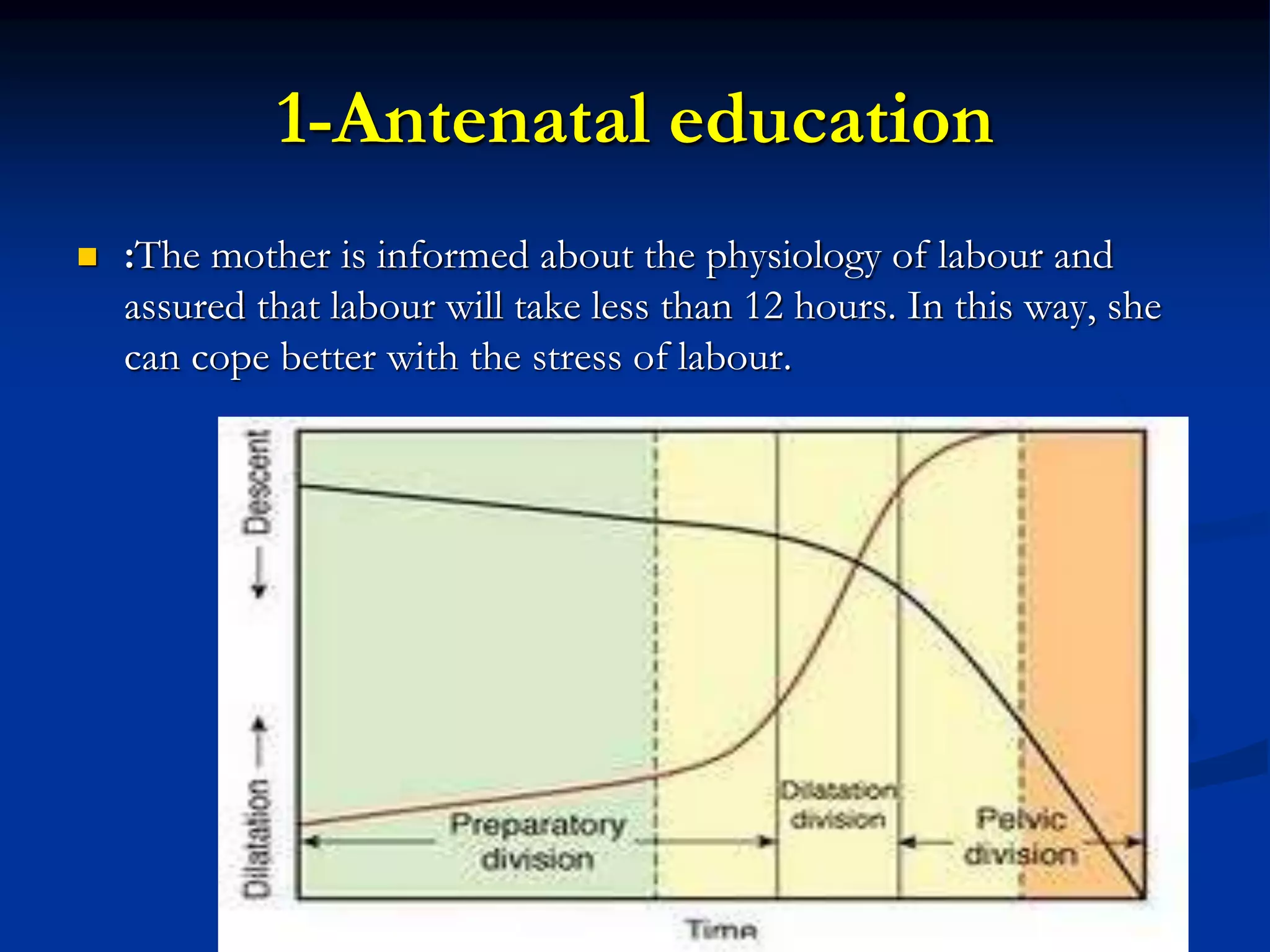
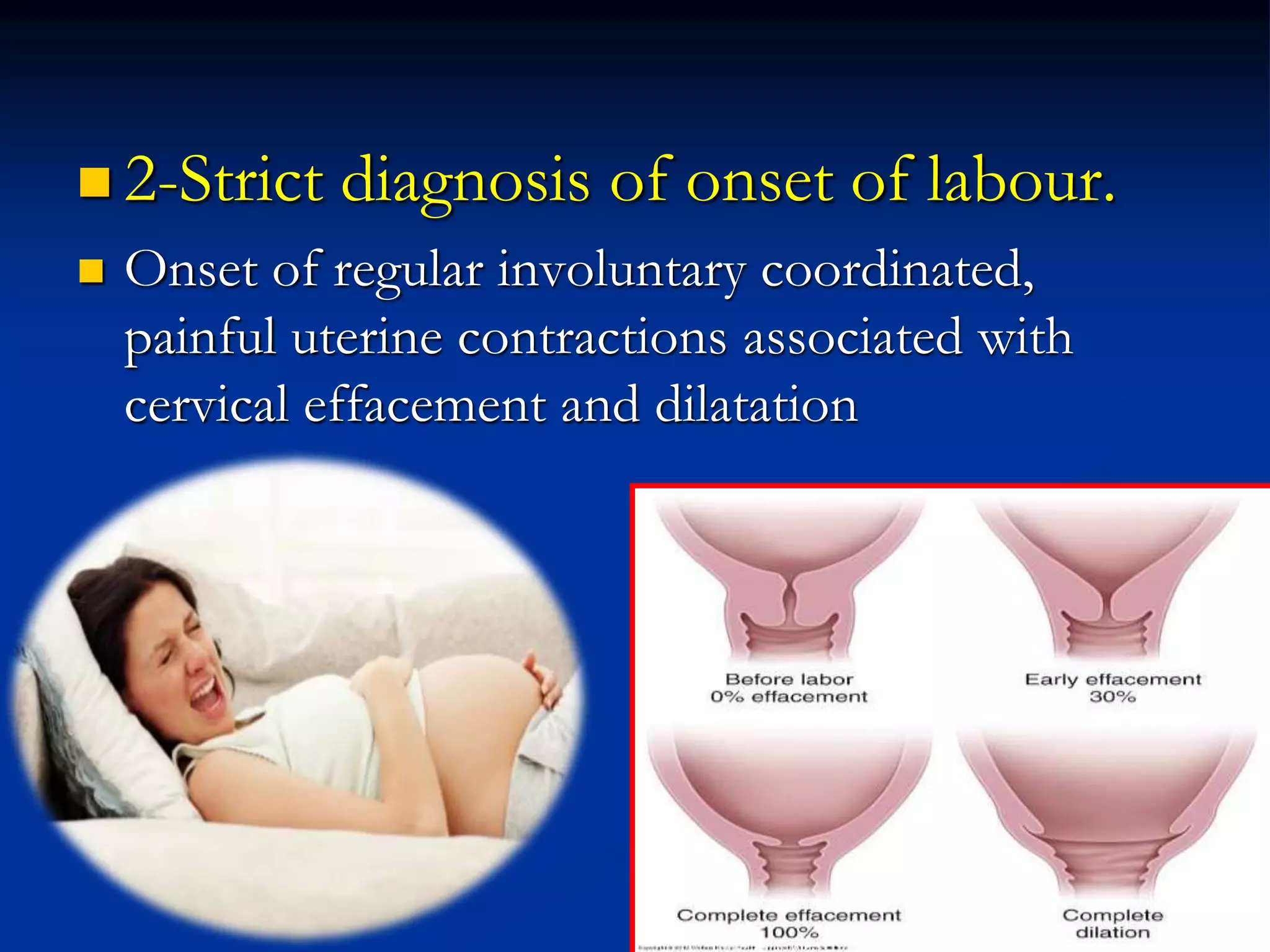
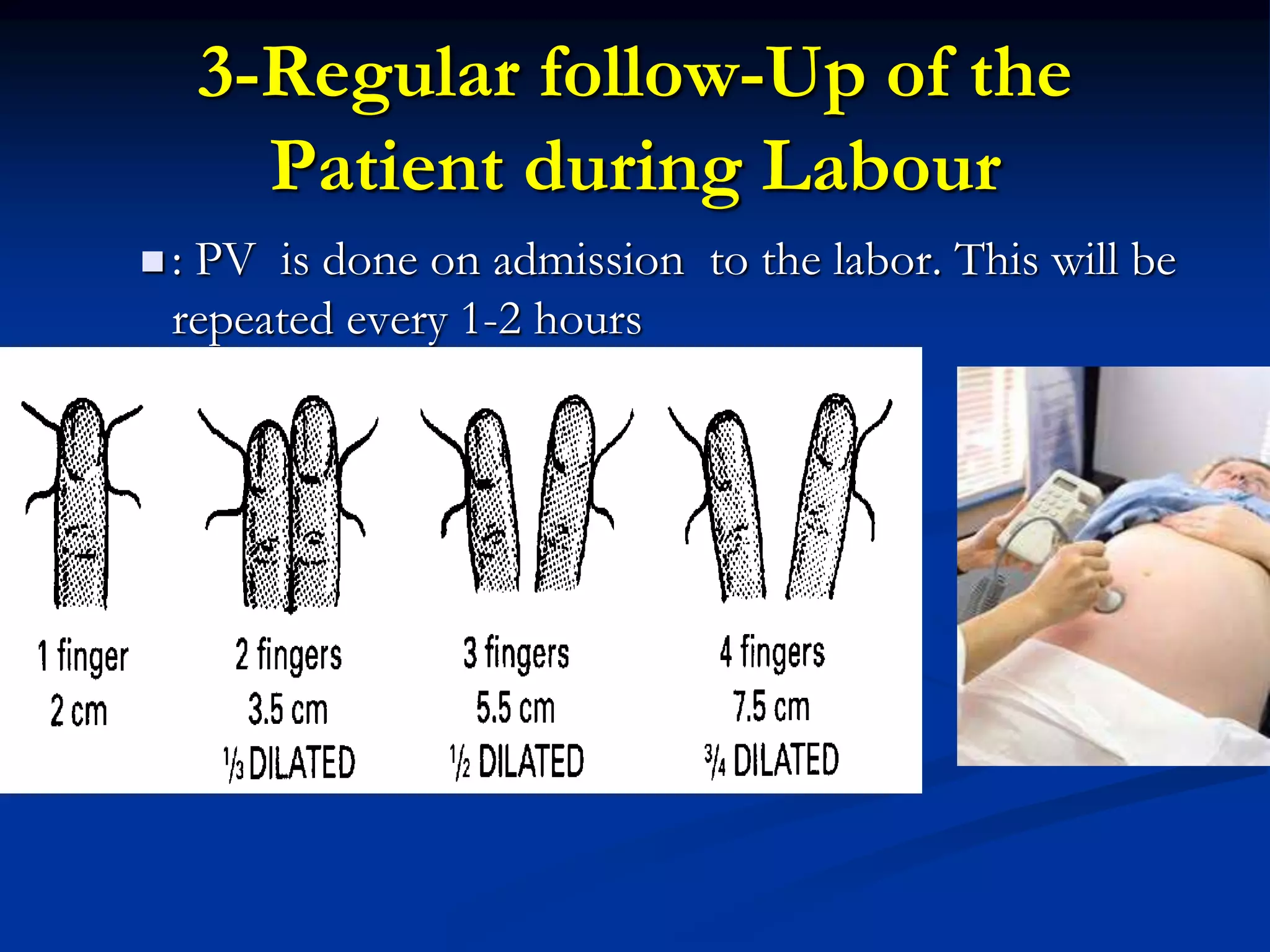
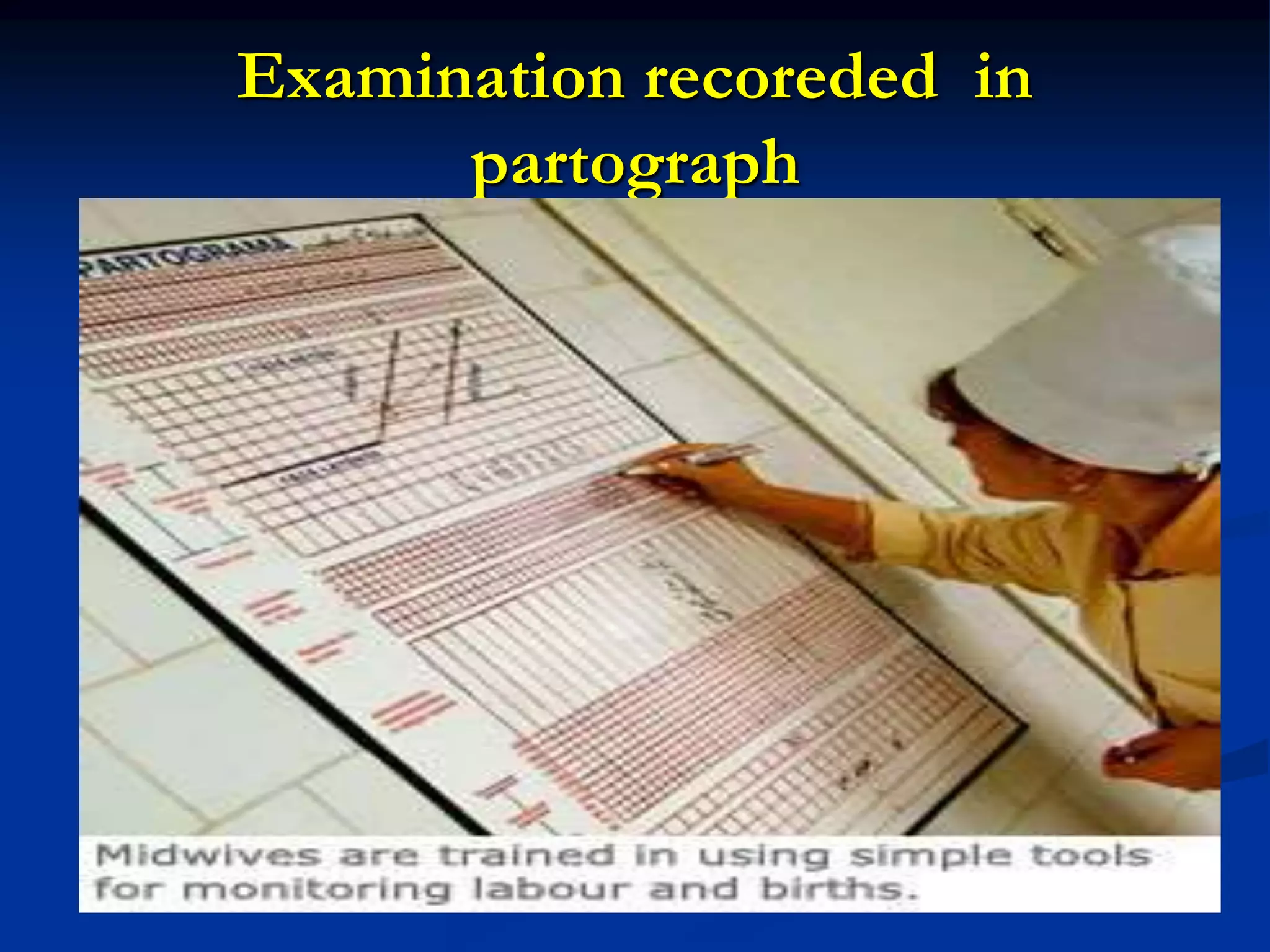
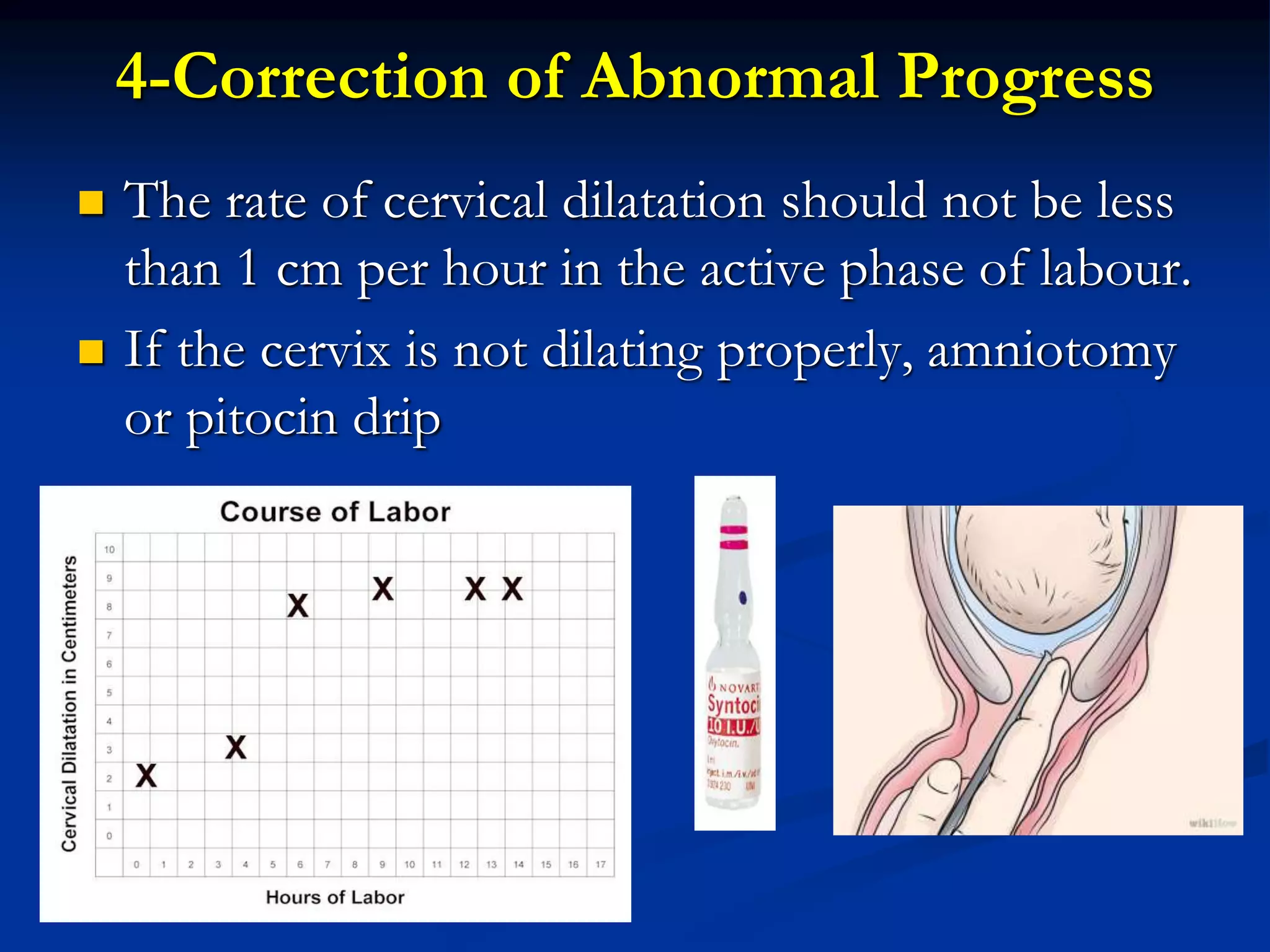
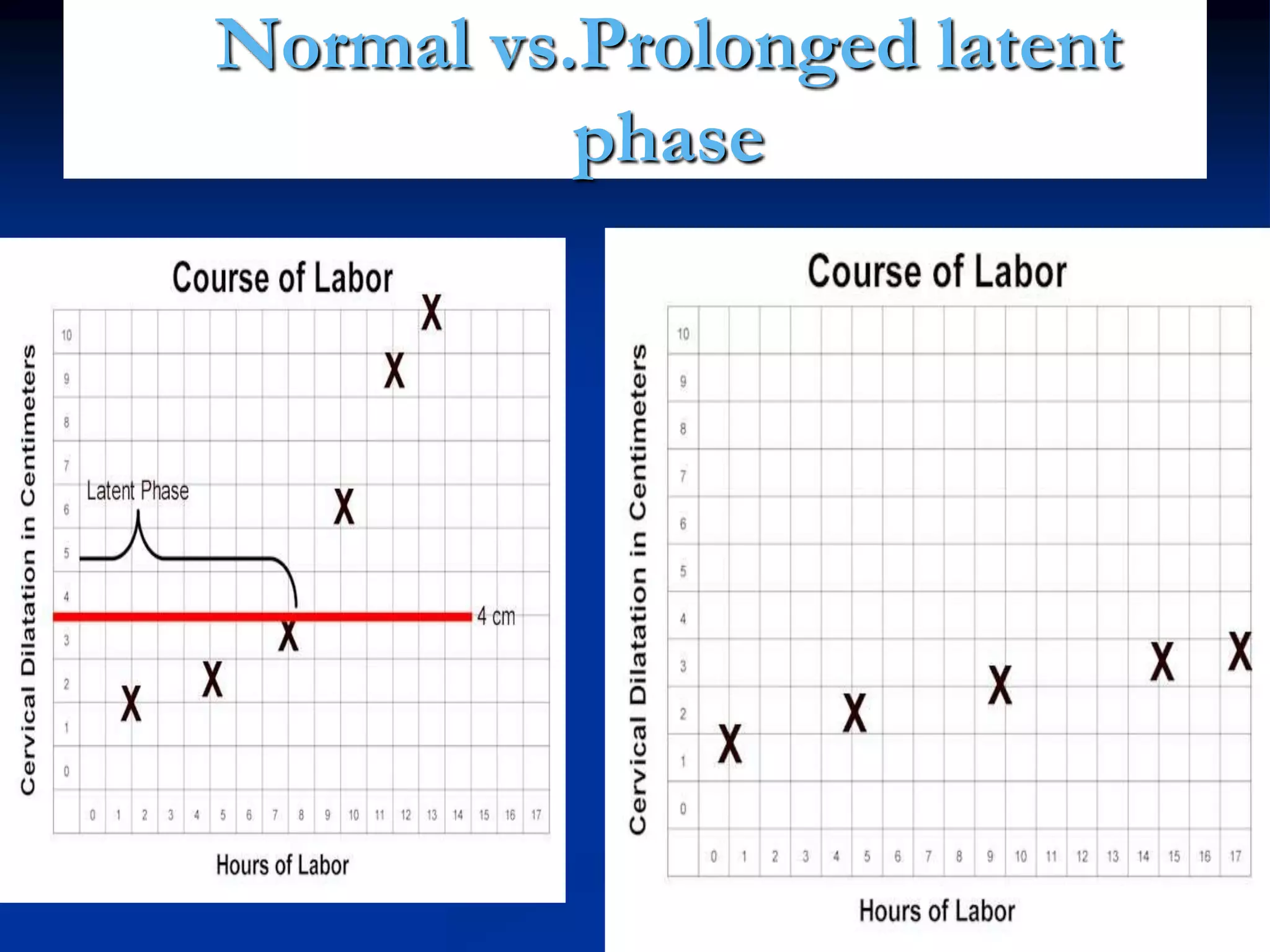
The document outlines the management of normal labor from admission to delivery, emphasizing the importance of a thorough history, examinations, and monitoring using a partograph. It details the phases of labor, fetal condition assessments, maternal care, and active management strategies to ensure timely delivery while minimizing complications. Active management principles include patient education, regular monitoring, and intervention for abnormal progress to enhance outcomes for both mother and baby.