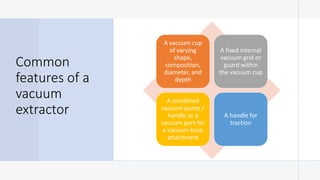
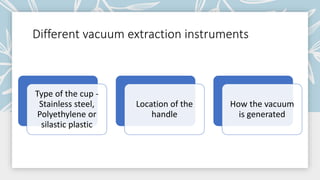
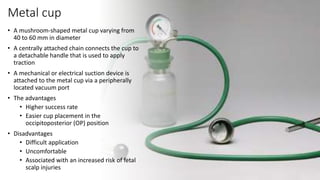
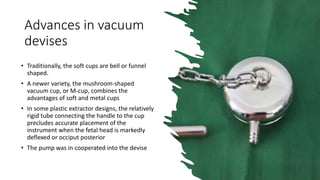
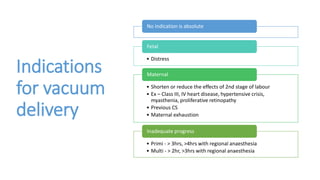
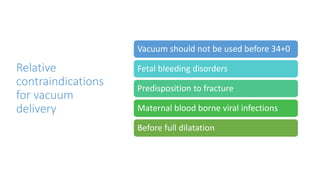
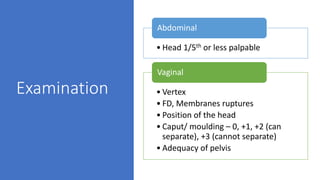
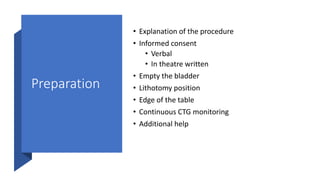
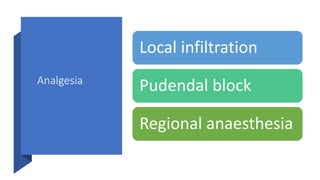
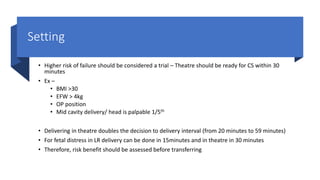
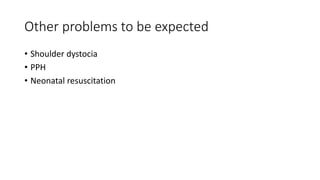
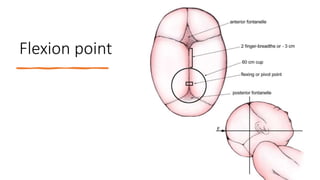
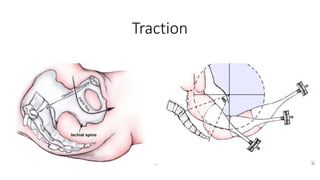
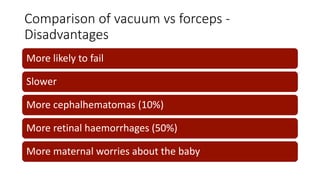
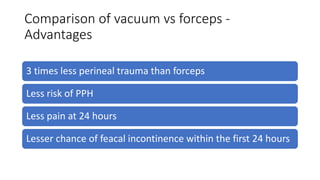
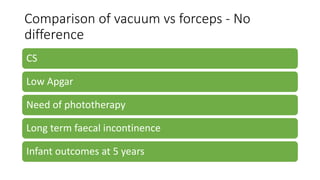
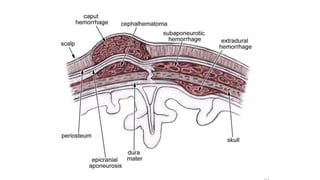
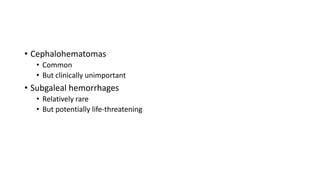
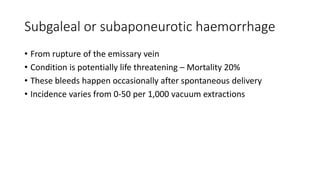
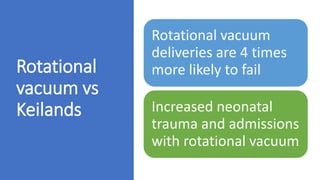
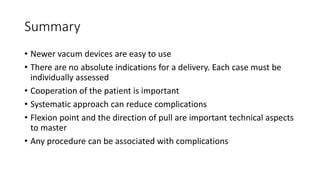
The document discusses the history, advantages, and challenges associated with vacuum delivery methods in obstetrics, focusing on different types of vacuum cups and their effectiveness. It highlights evolving practices, contraindications, and the procedures to follow for a successful vacuum delivery while comparing its outcomes to forceps delivery. The document emphasizes the importance of patient cooperation and careful assessment to reduce complications during delivery.