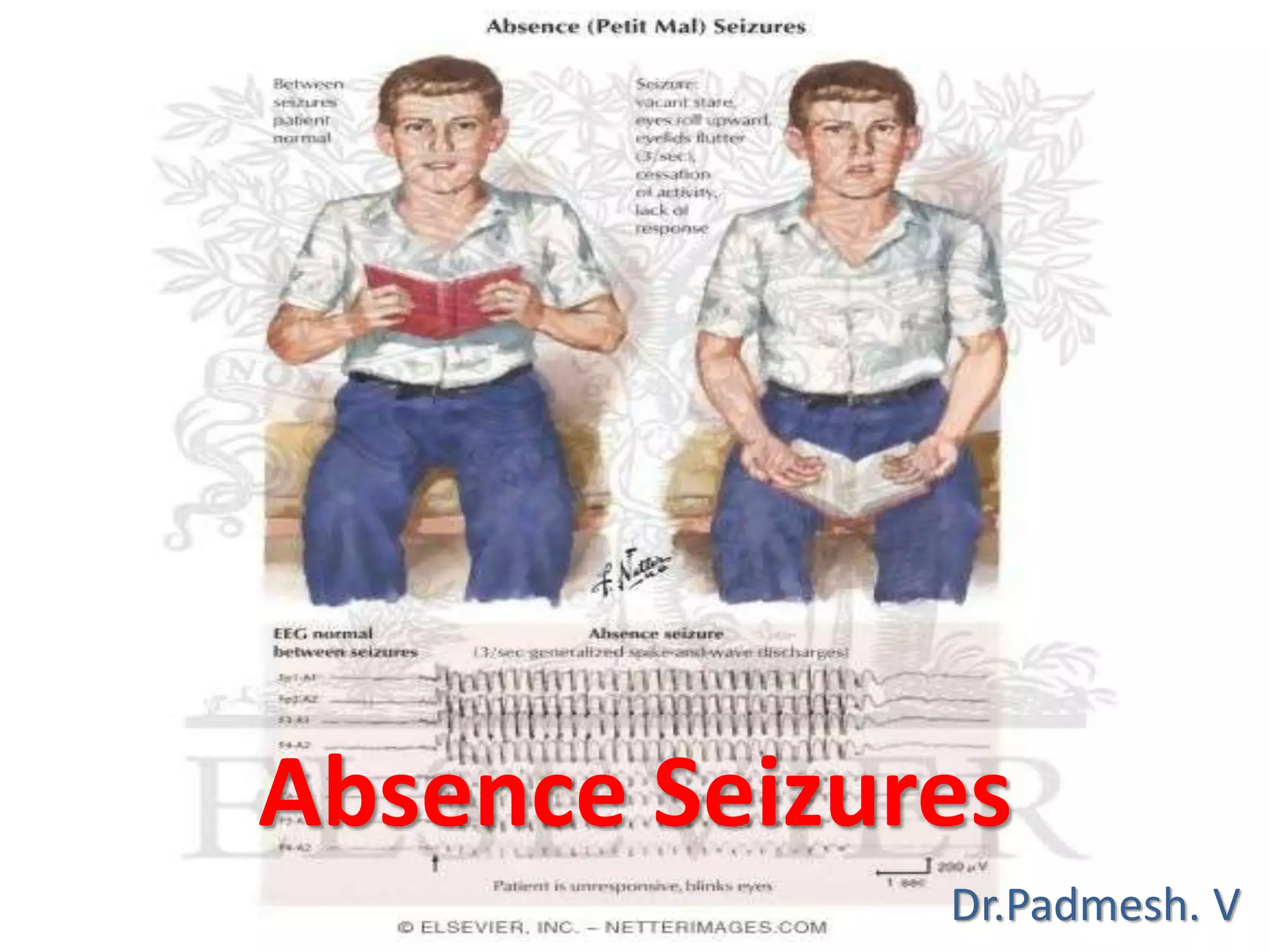
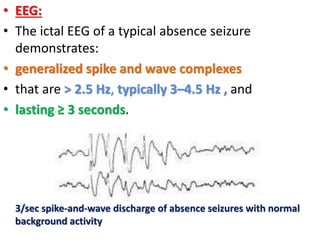
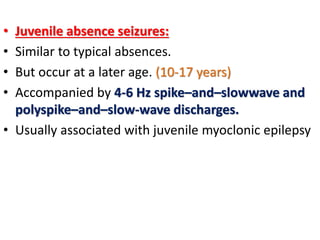
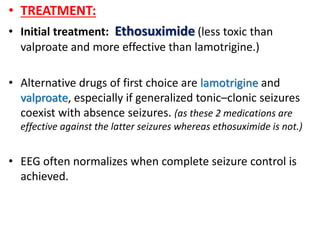
Absence seizures typically have two peaks in age of onset, between 5-8 years and near 12 years. Childhood absence epilepsy (CAE) accounts for 10-17% of childhood epilepsy cases and is characterized by brief seizures without aura or postictal period. Typical absence seizures involve eye blinking or movements lasting a few seconds accompanied by generalized spike-and-wave discharges on EEG. Treatment typically begins with ethosuximide, though valproate or lamotrigine may be used if generalized tonic-clonic seizures are also present. While often labeled benign, CAE has variable outcomes, with some studies finding generalized tonic-clonic seizures develop later in 40% of cases.