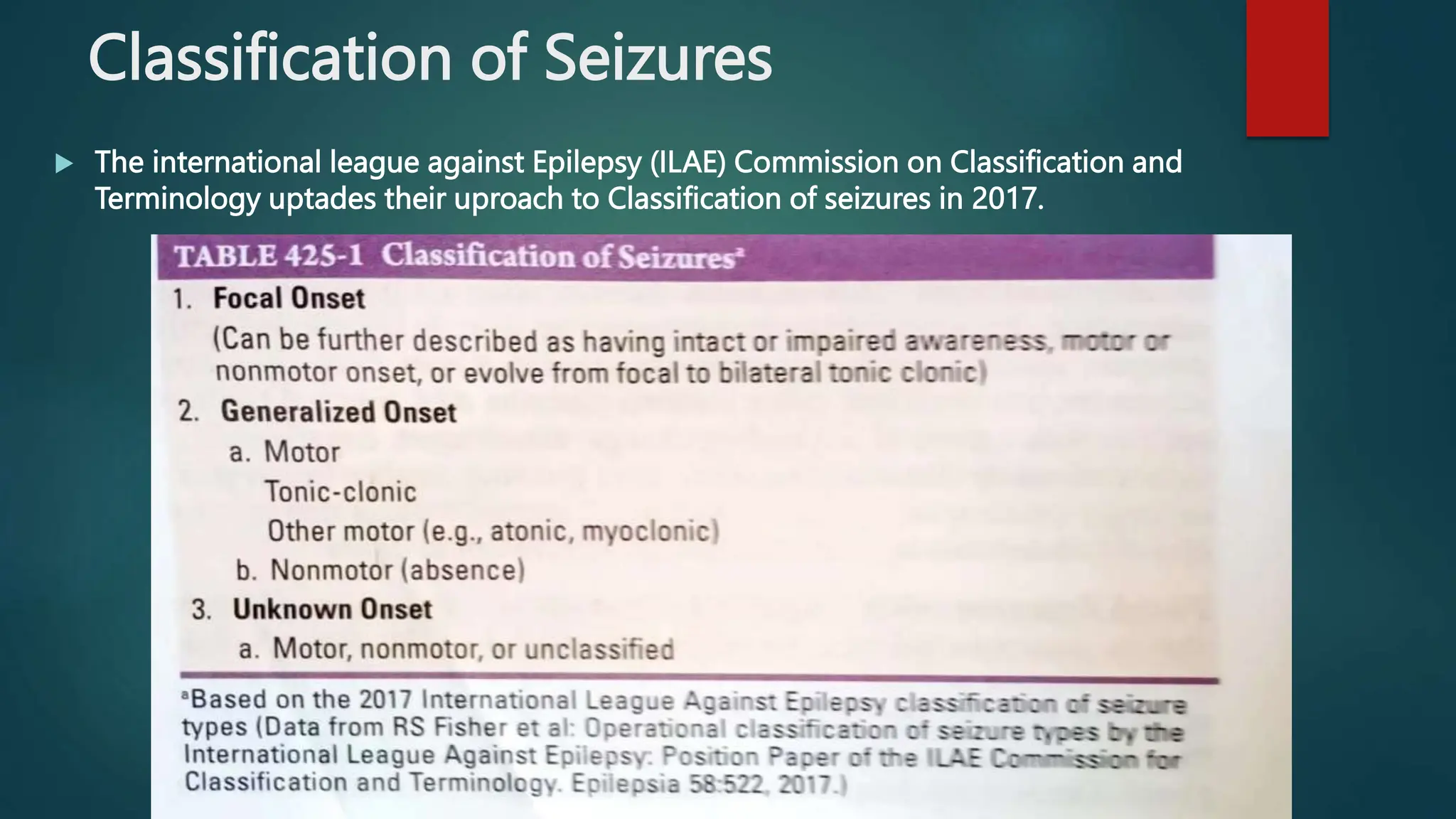
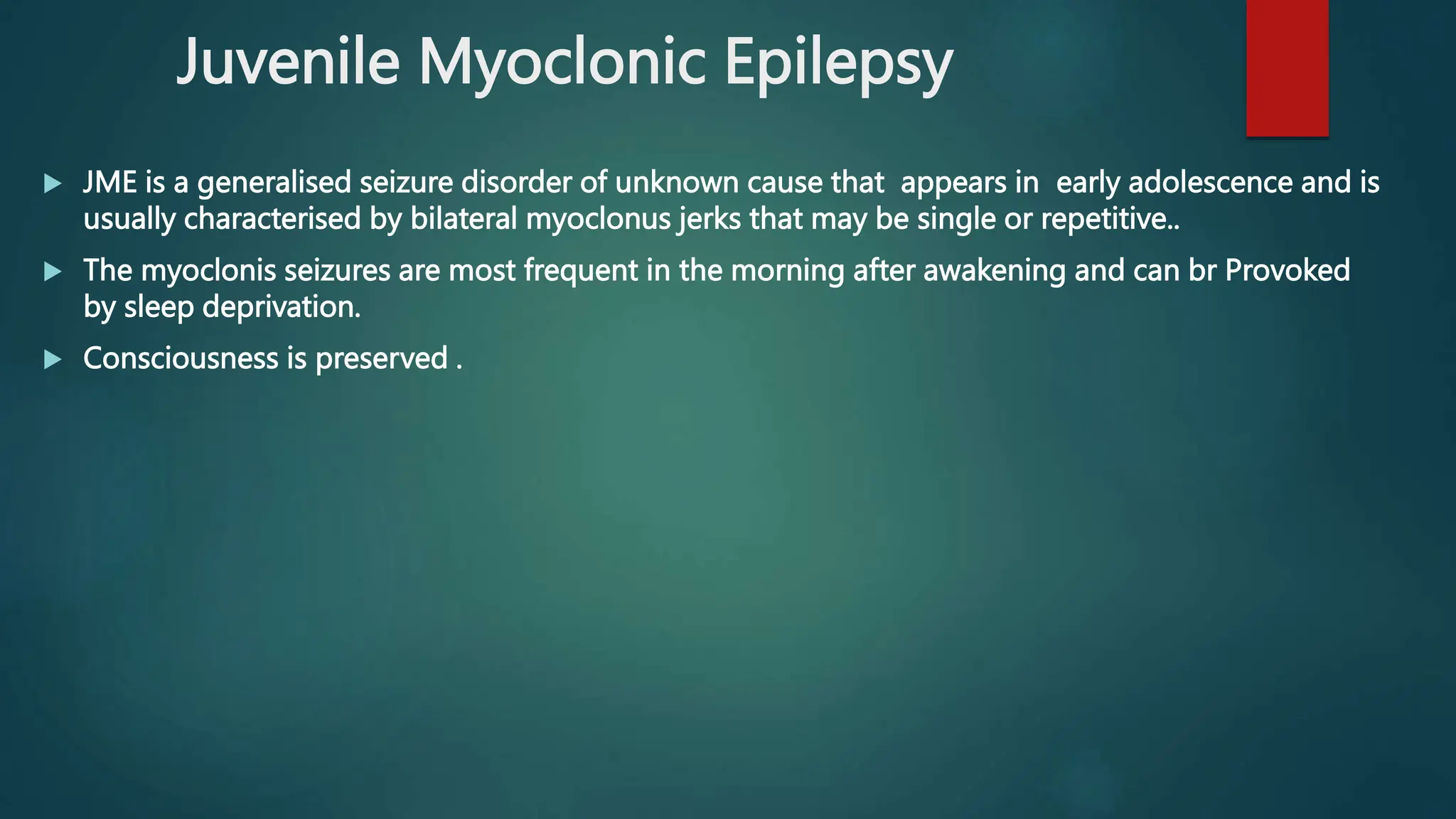
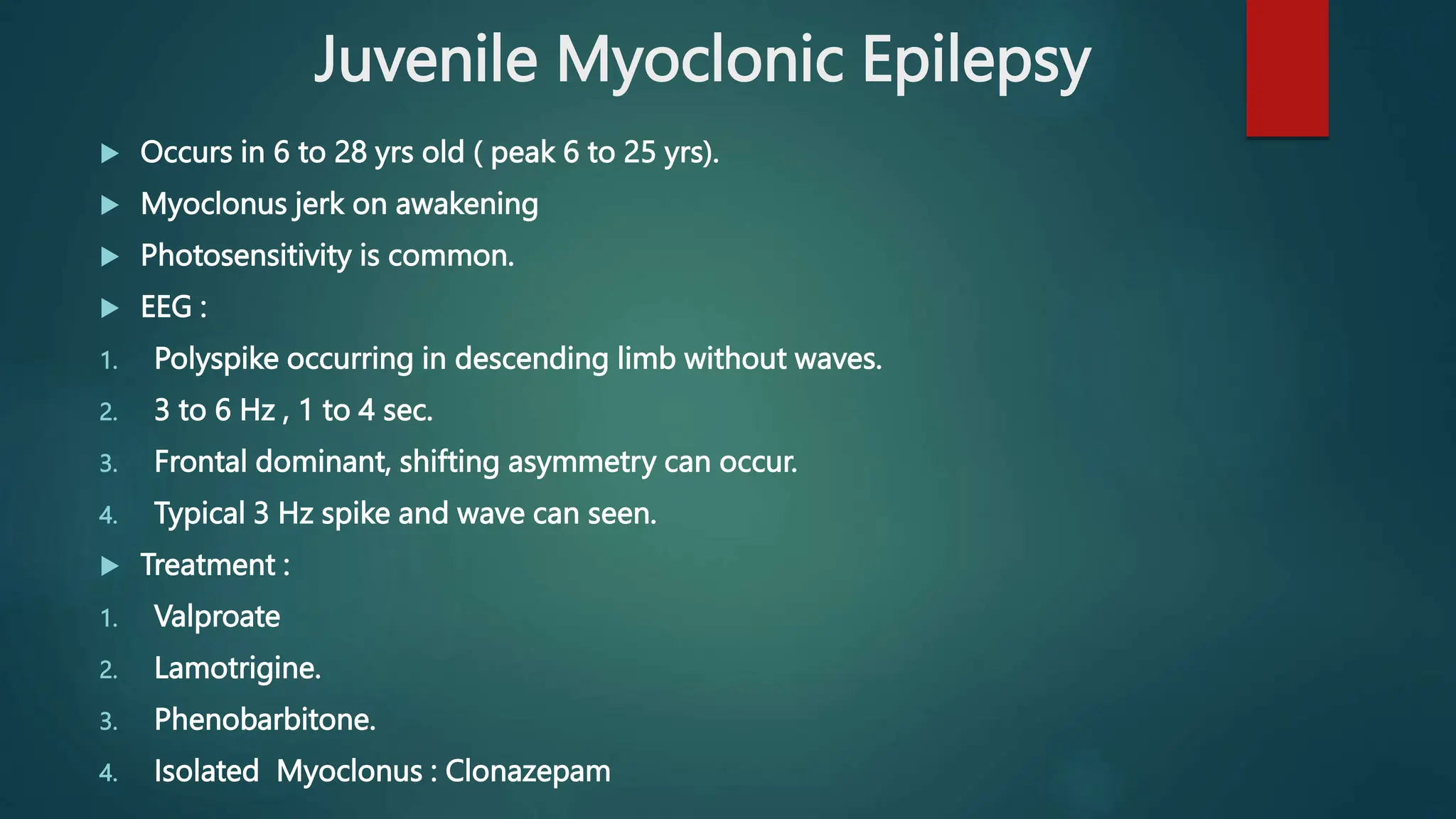
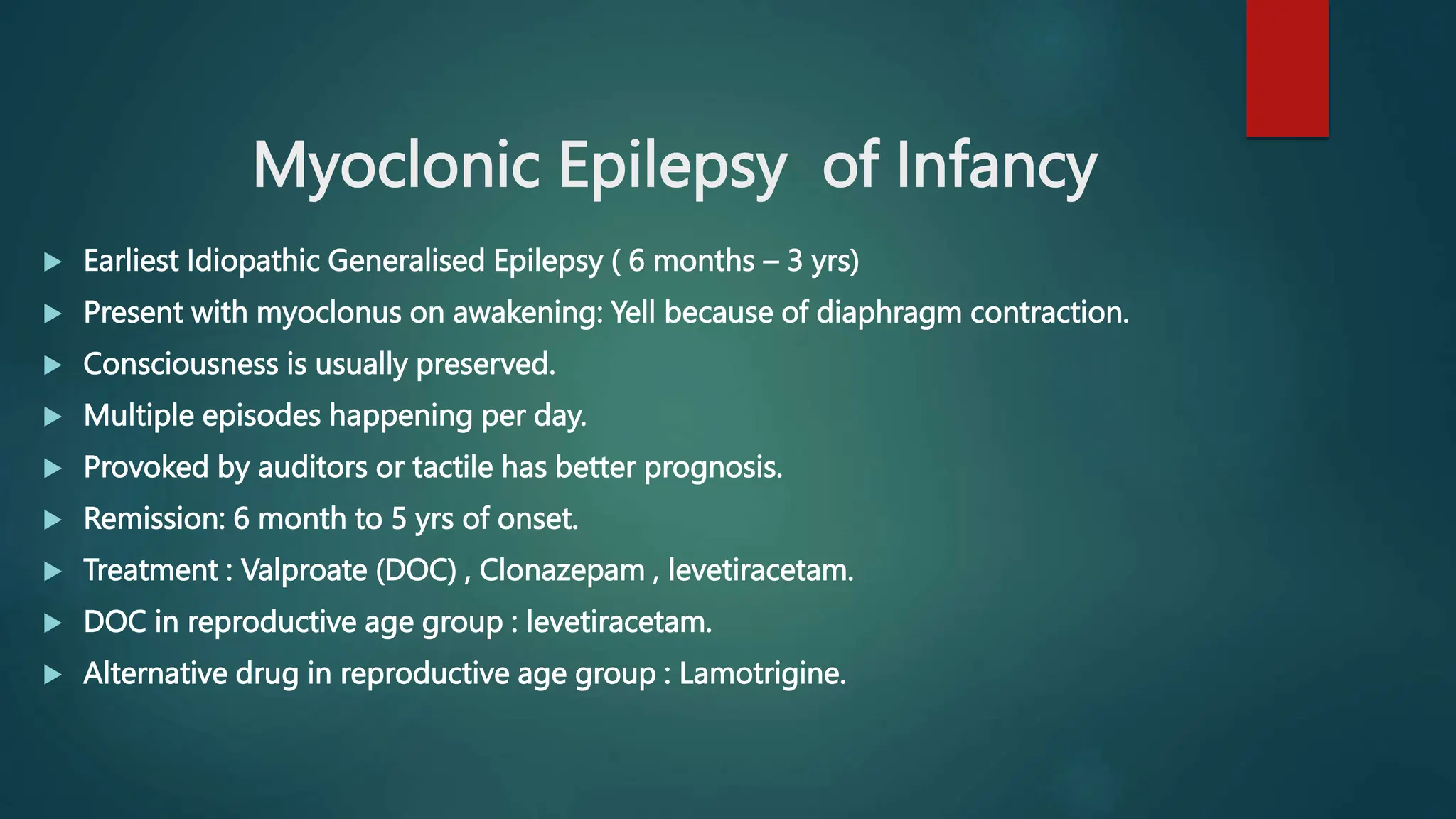
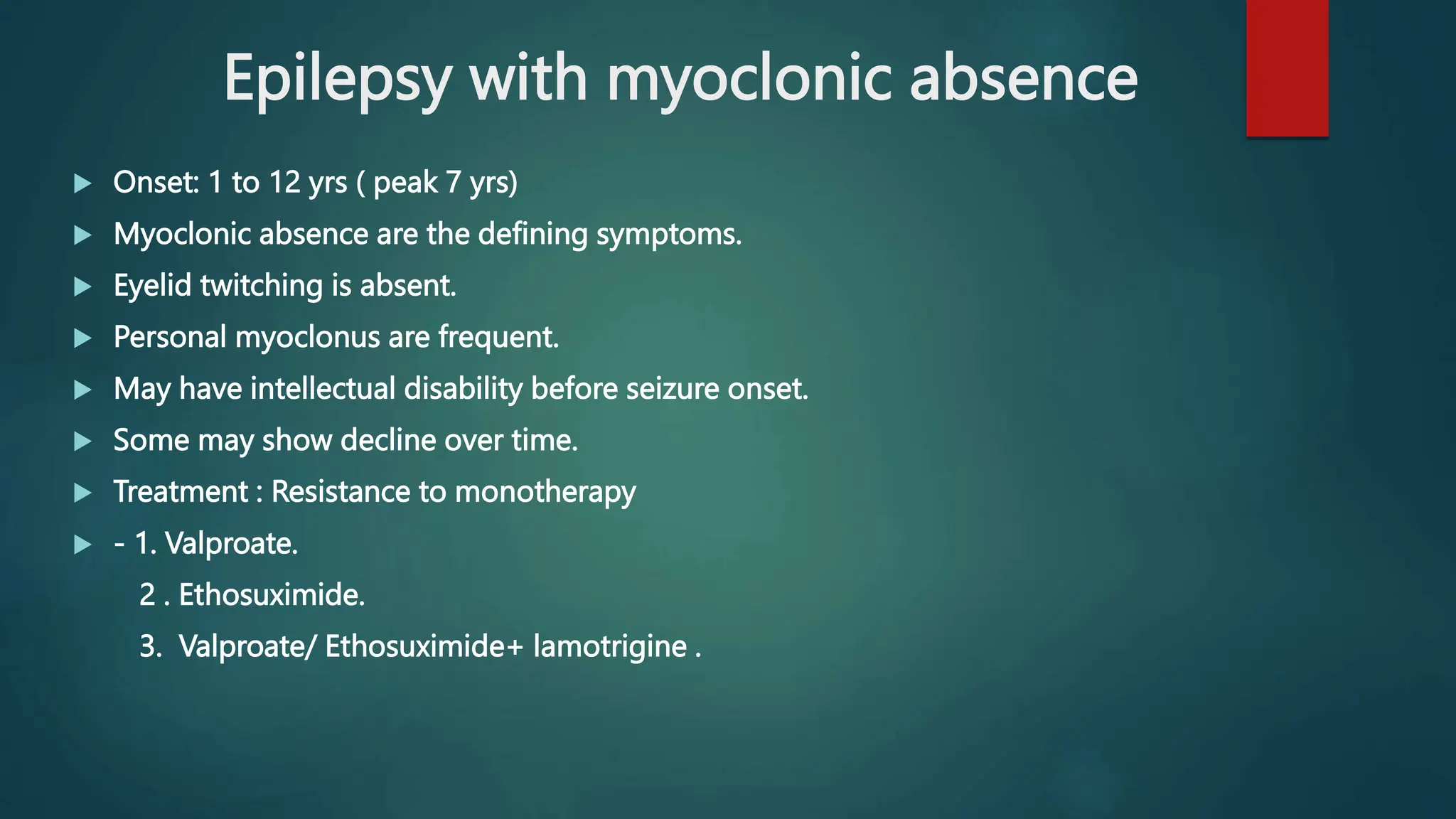
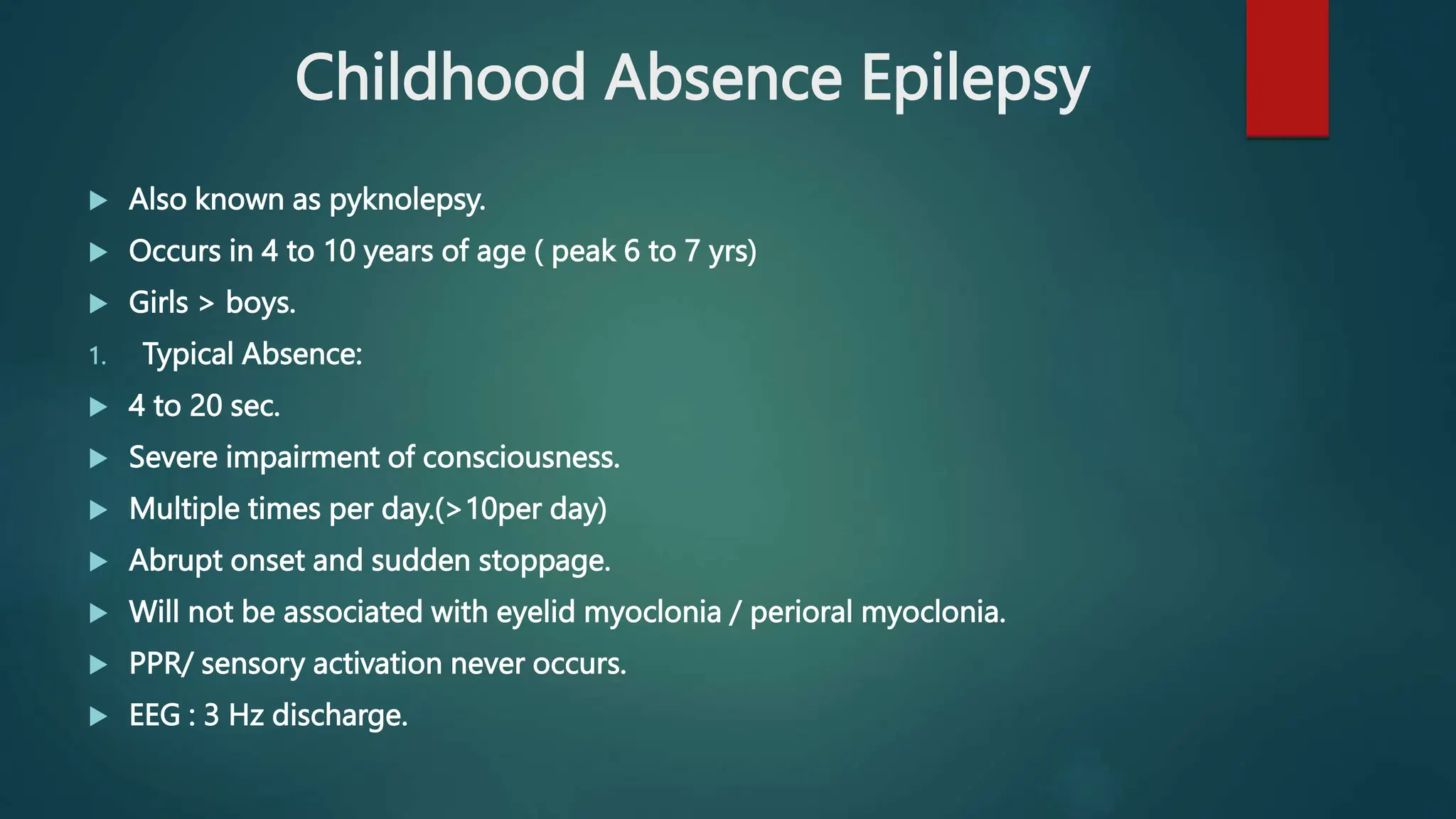
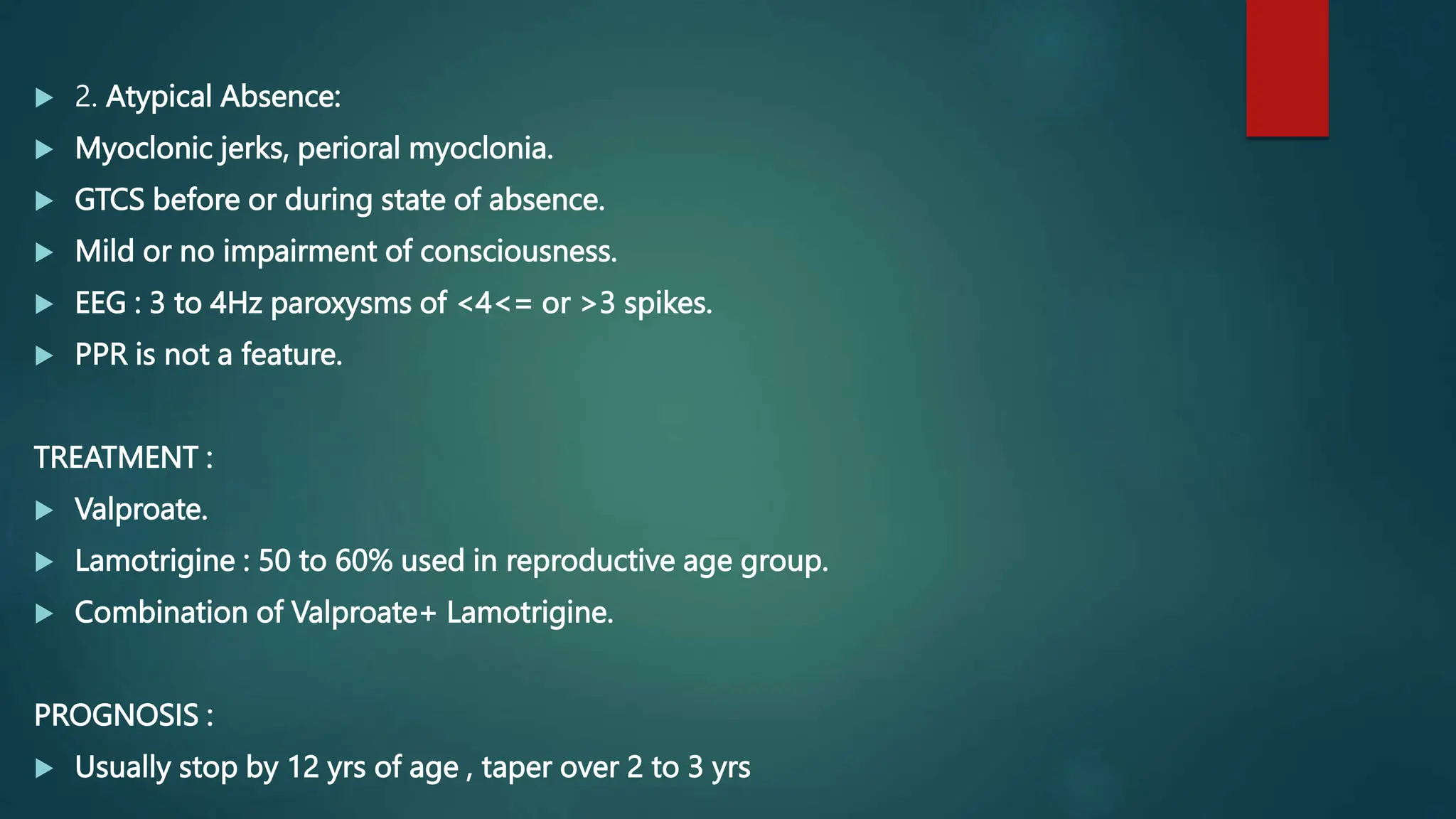
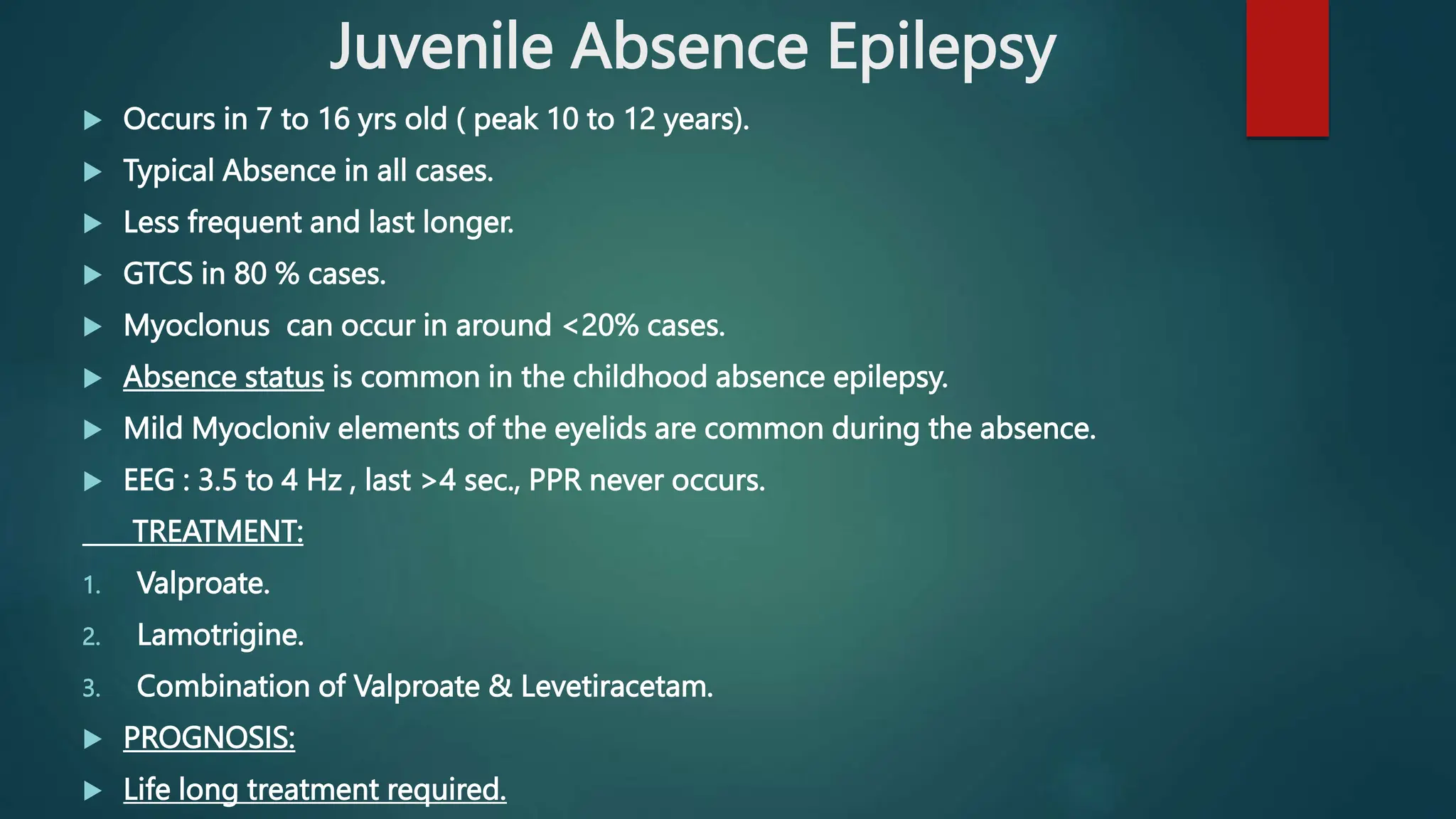
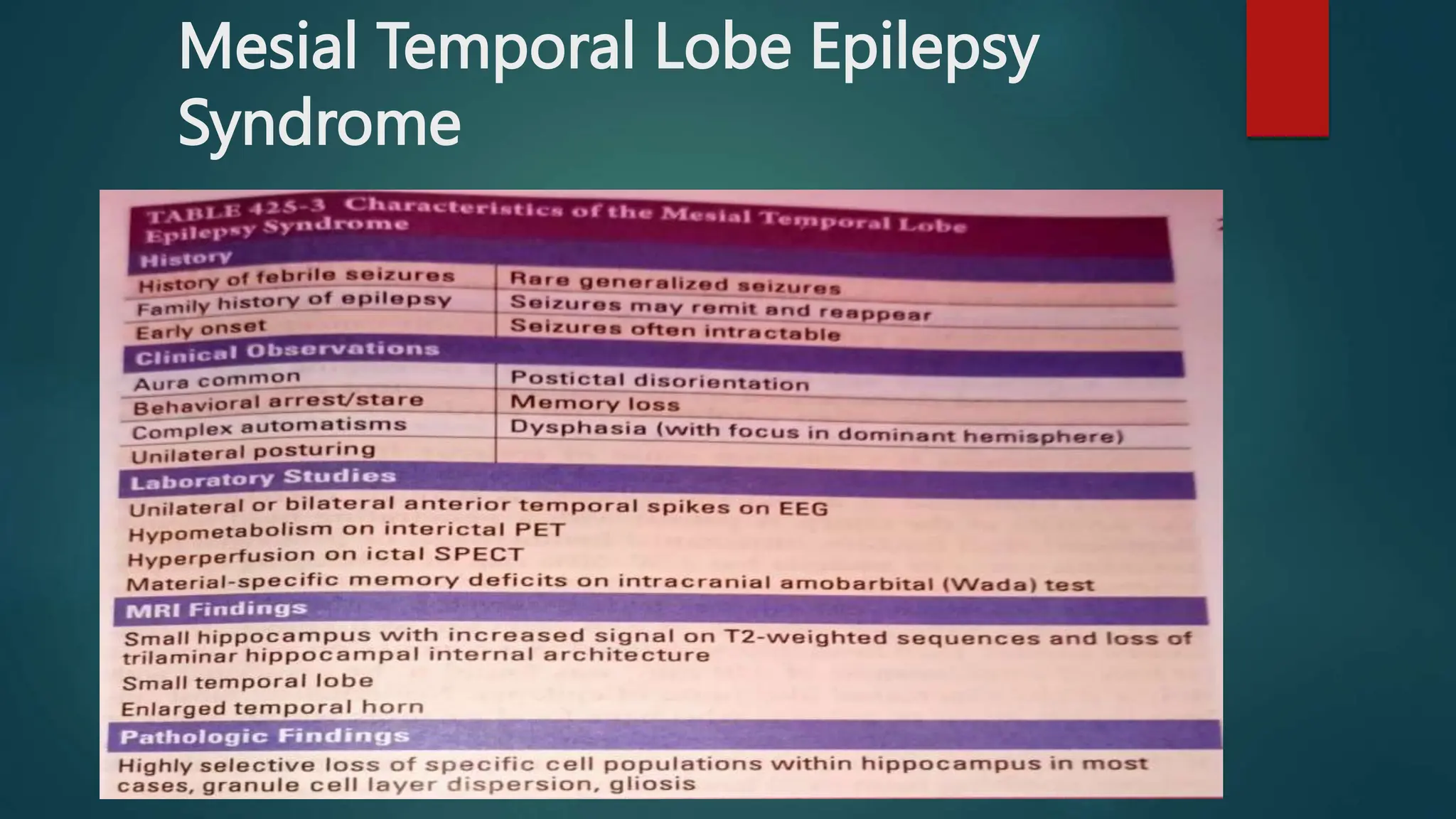
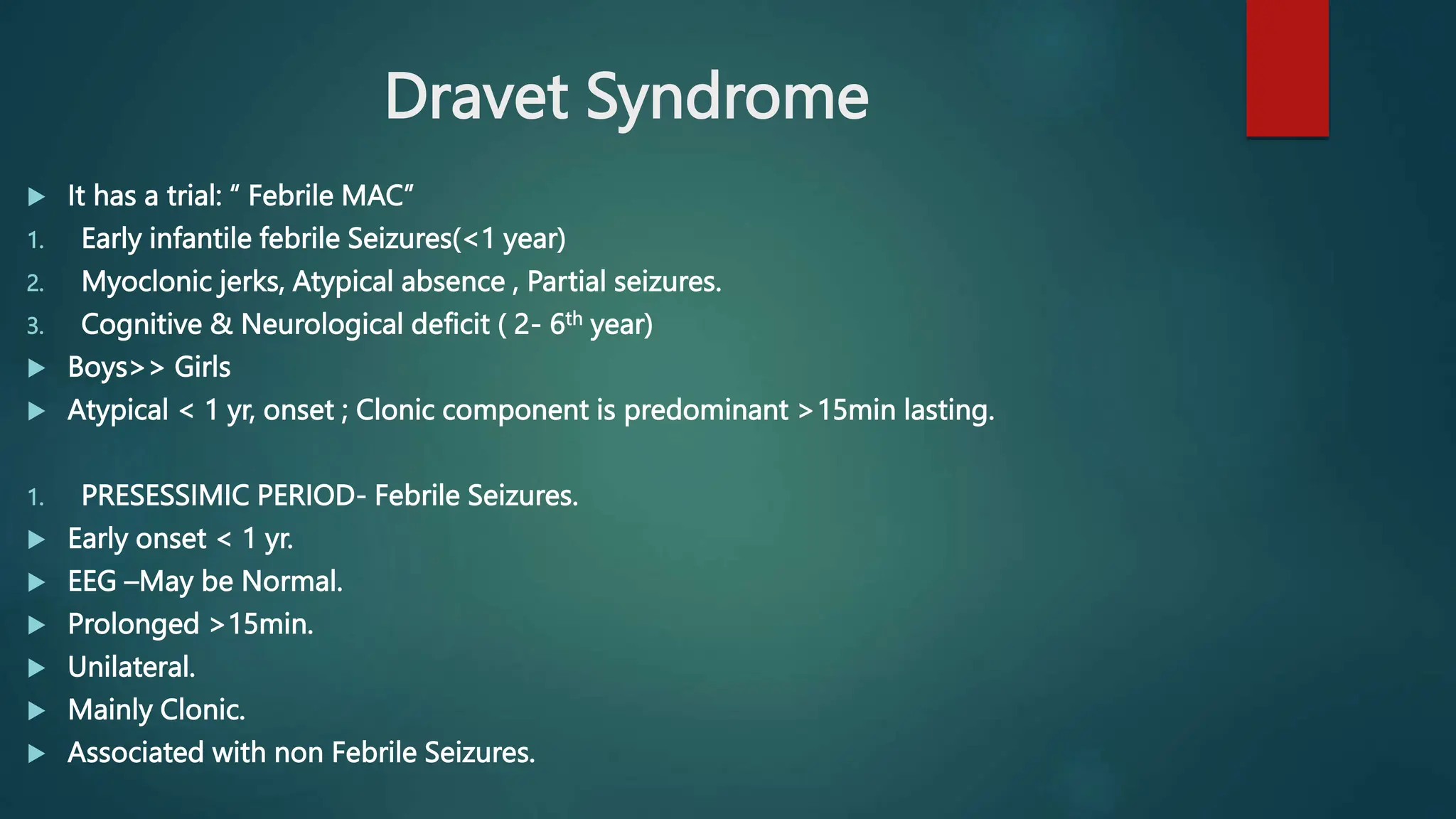
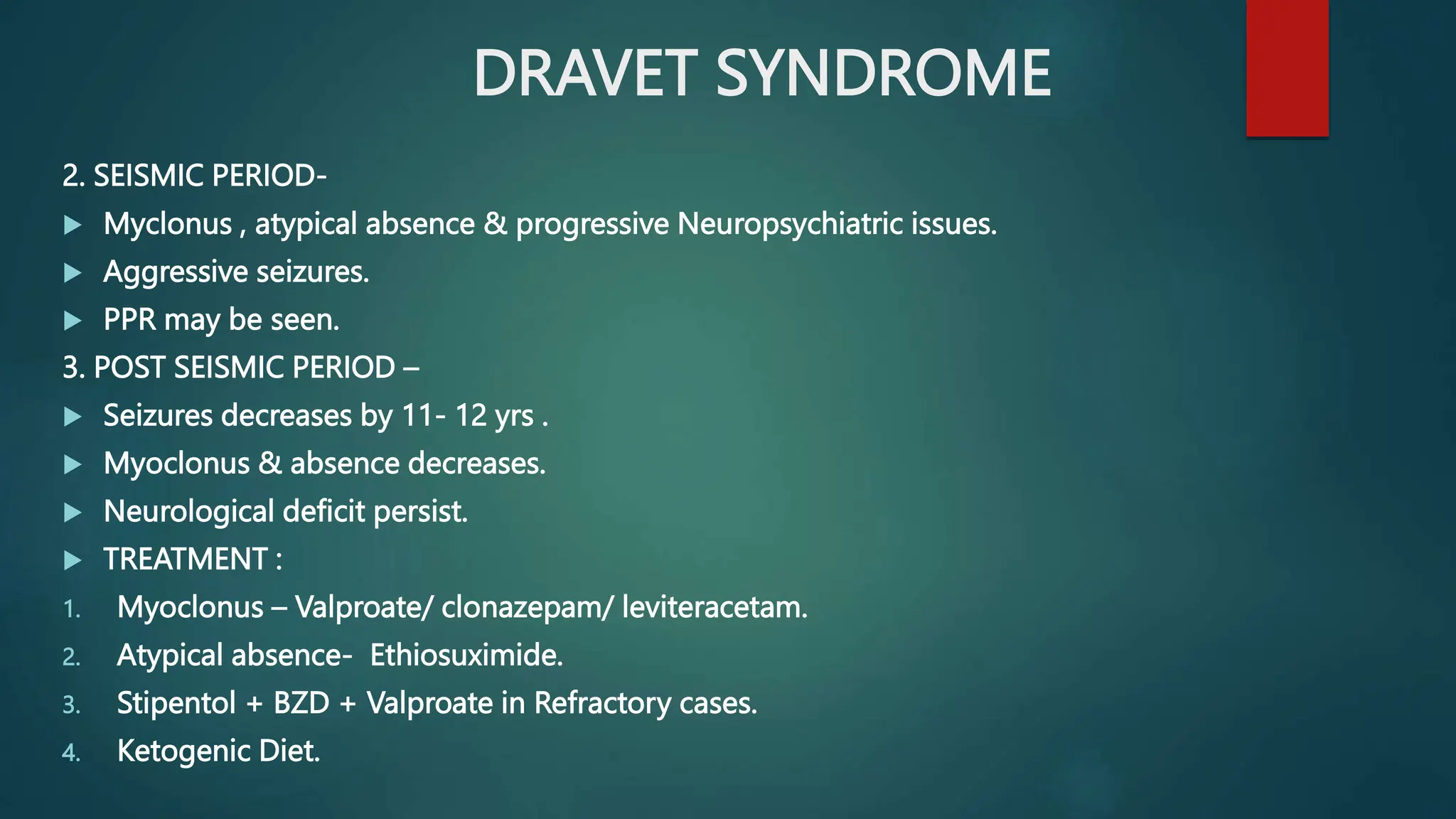
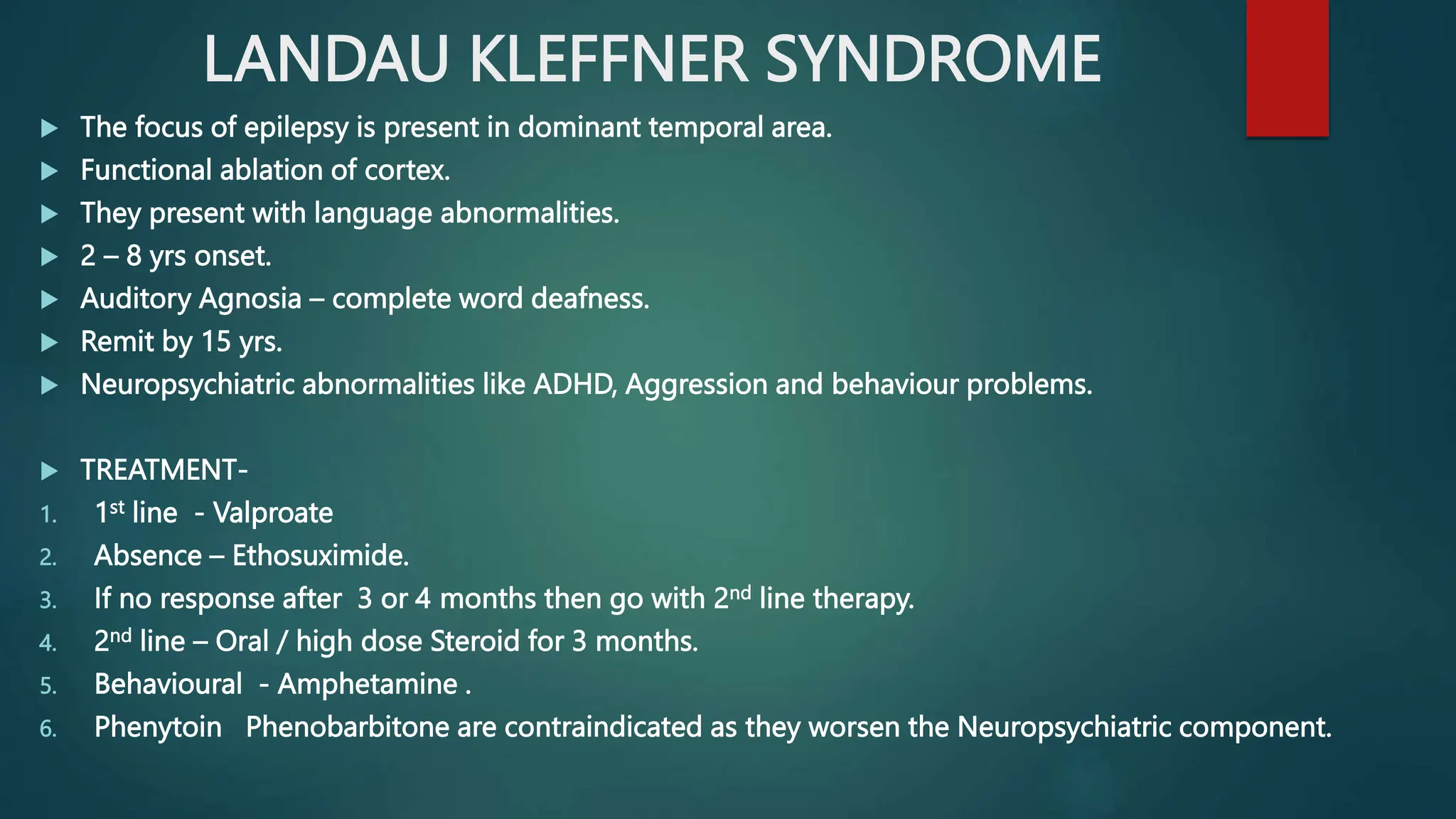
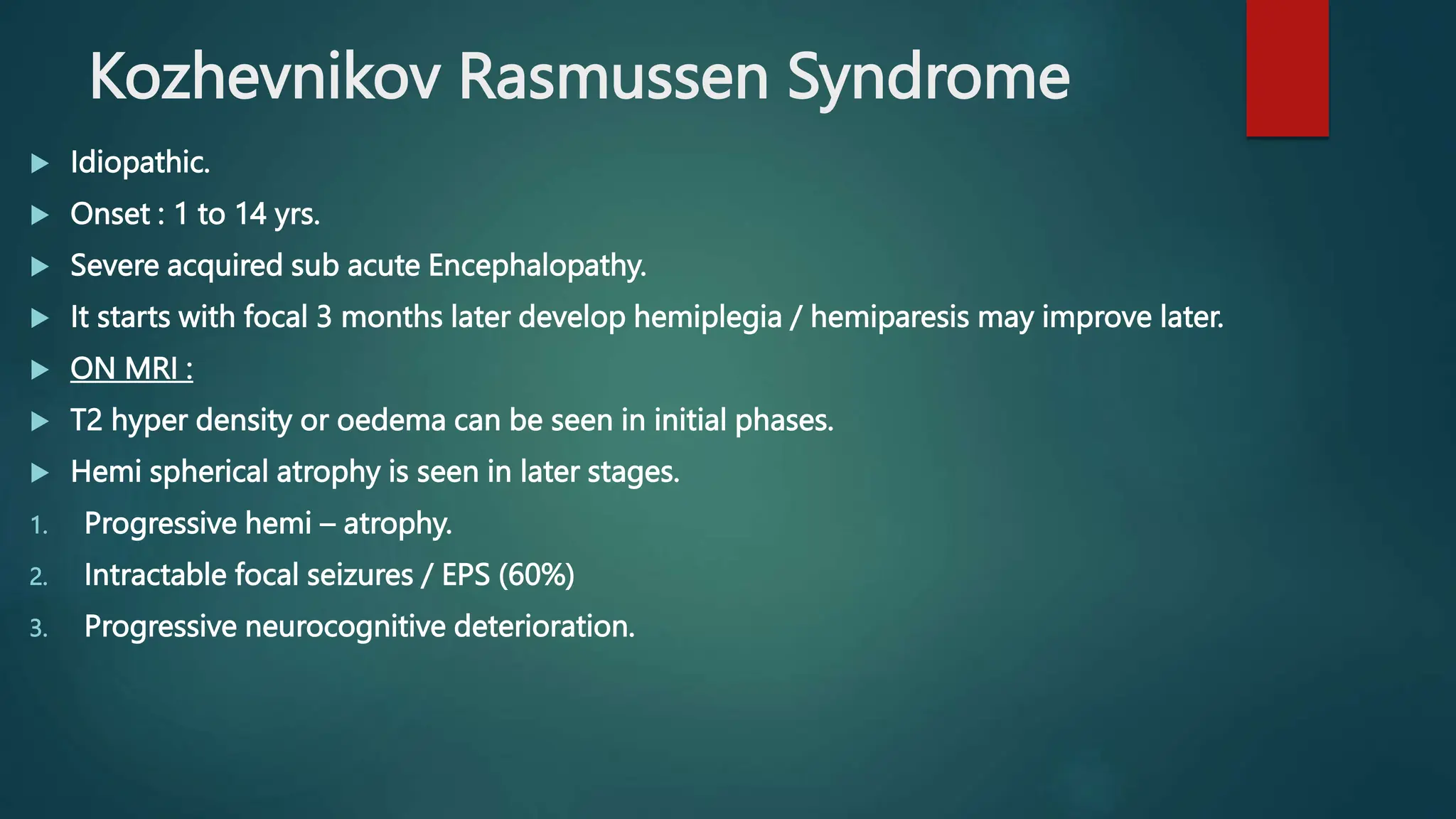
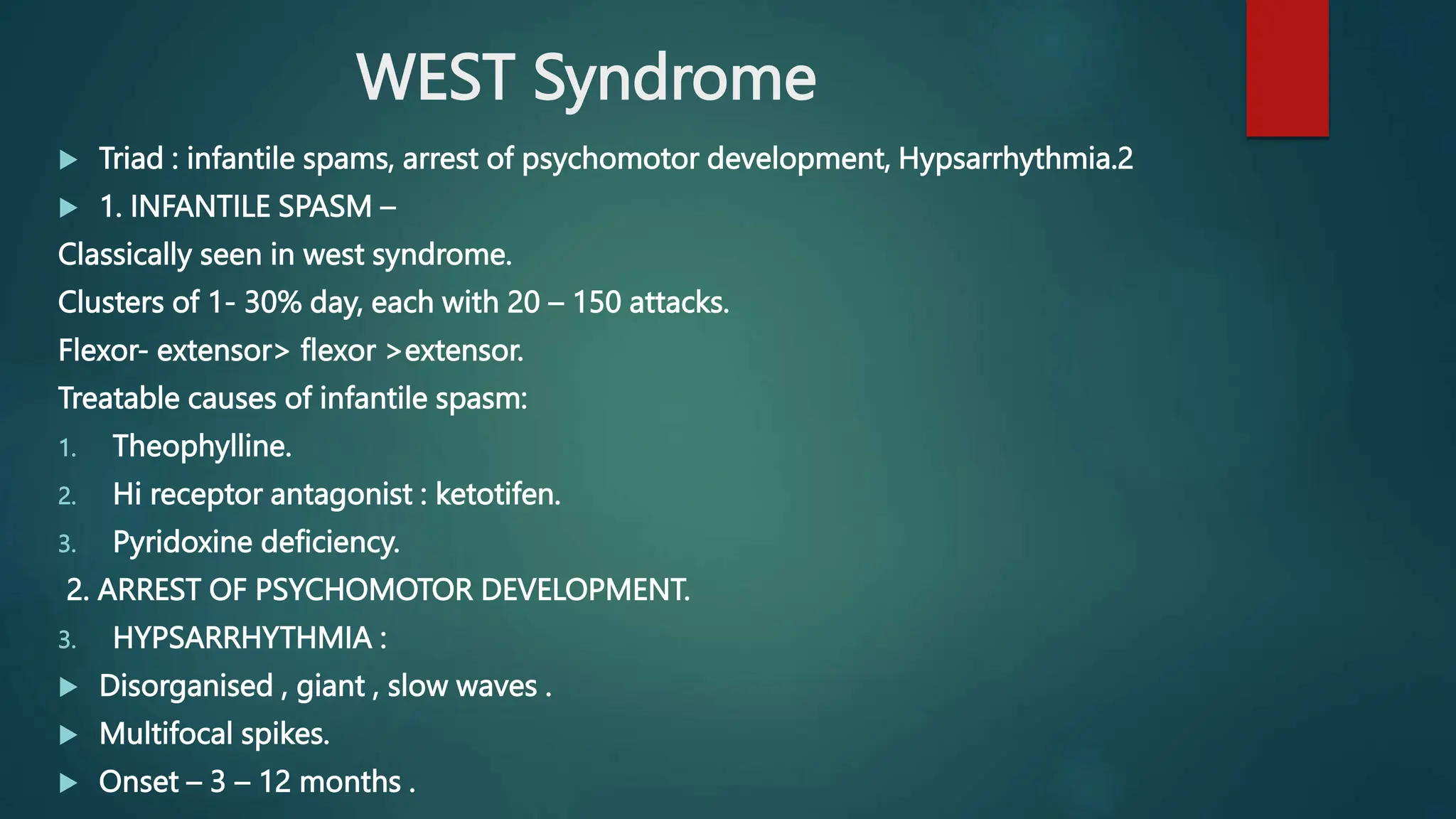
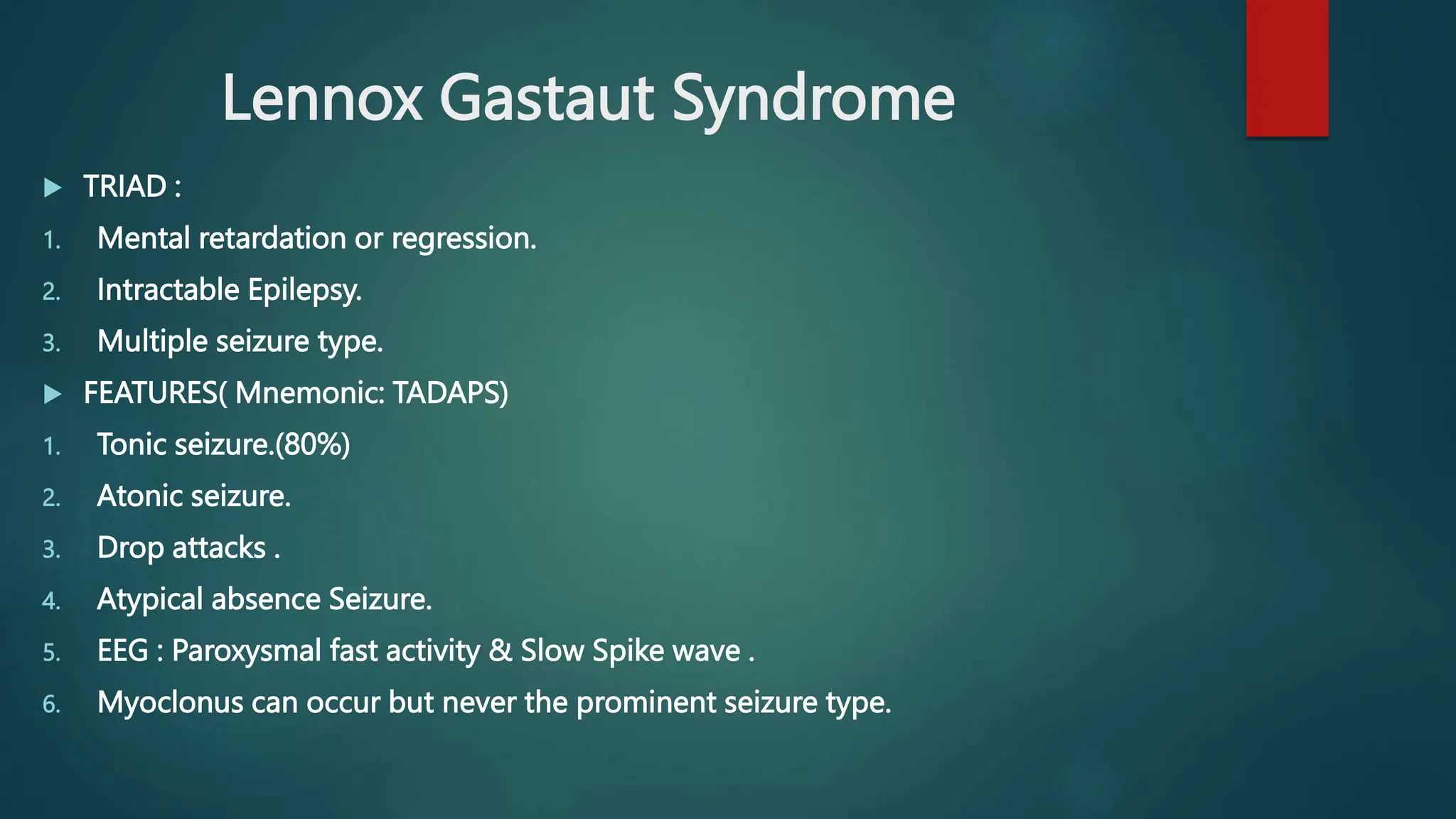
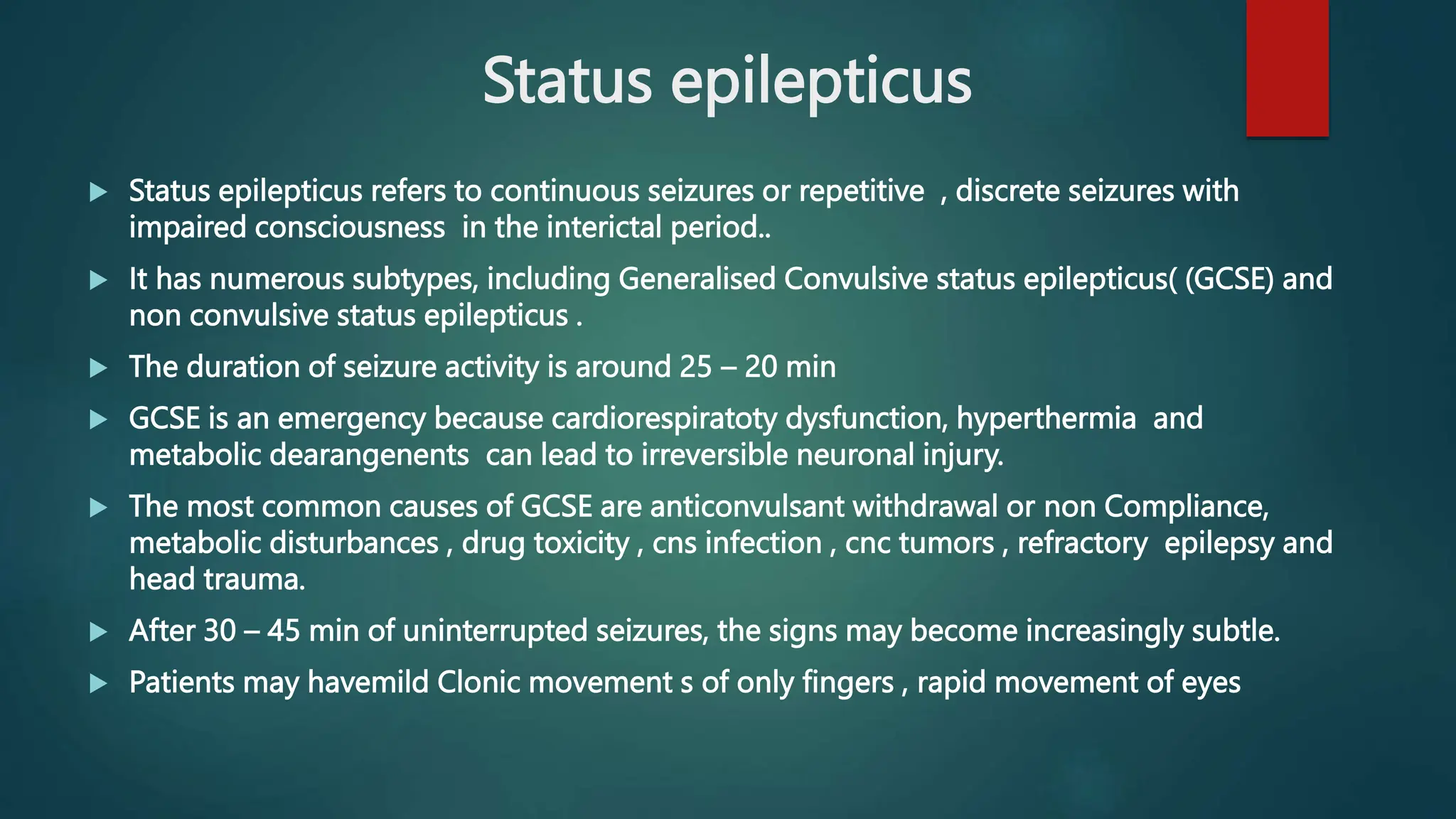
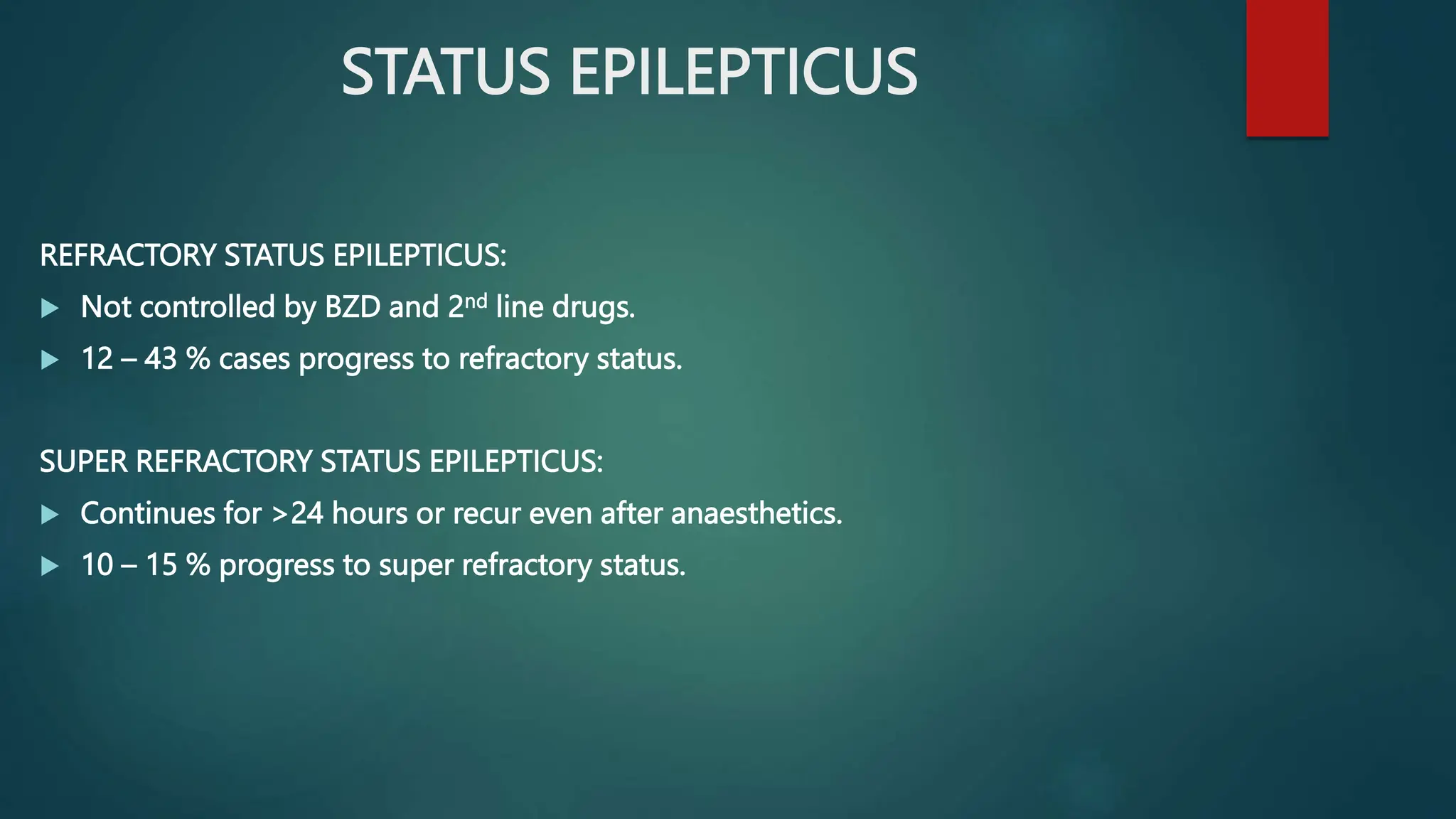
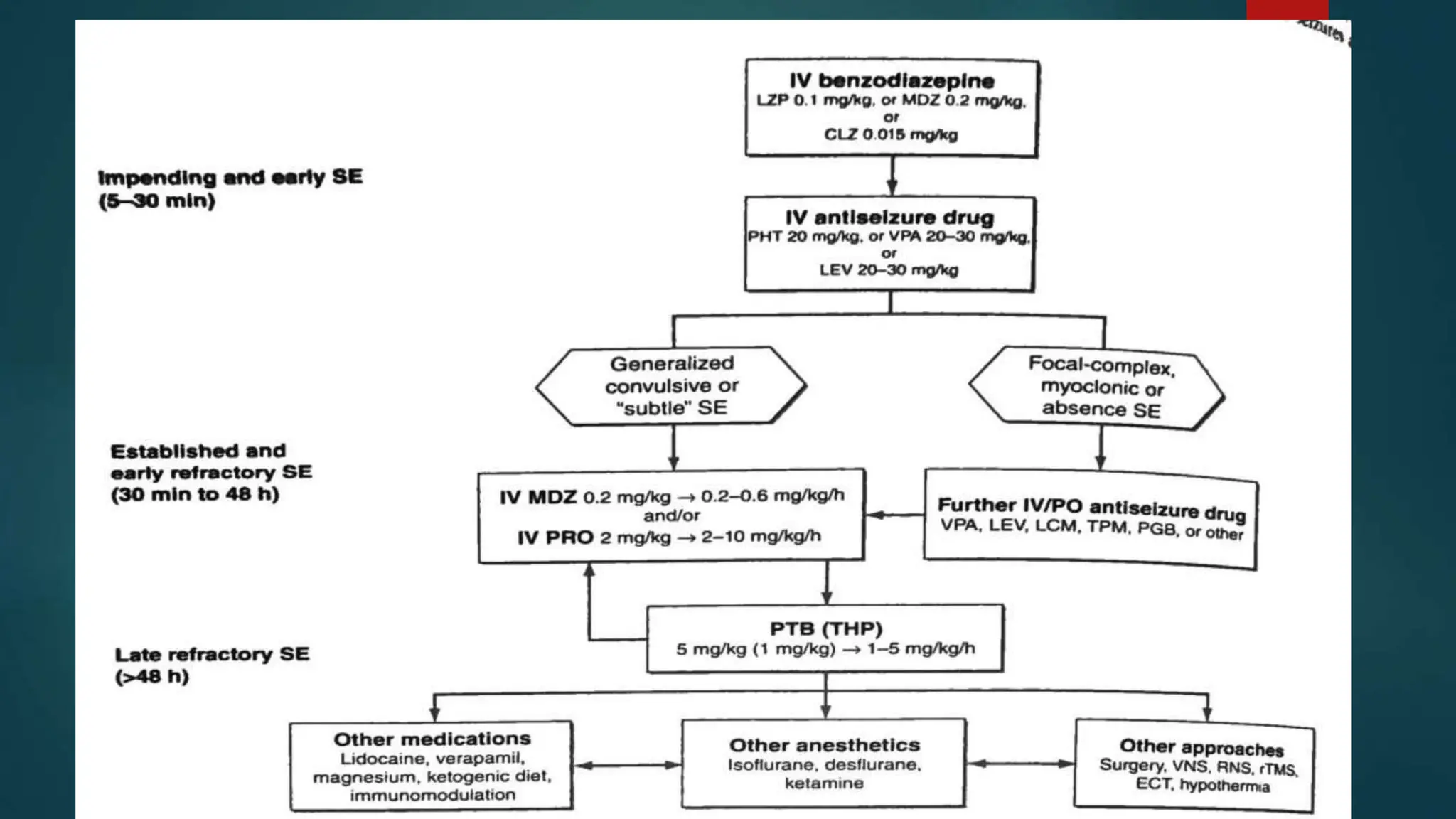
The document provides an extensive overview of epilepsy and seizure classification, highlighting definitions, differences between seizures and epilepsy, and classifications such as focal and generalized seizures. It details various types of seizures, their characteristics, clinical manifestations, diagnostic methods like EEG, and treatment options for different epilepsy syndromes including juvenile myoclonic epilepsy, childhood absence epilepsy, and more. Additionally, it discusses status epilepticus, its types, causes, and clinical significance.