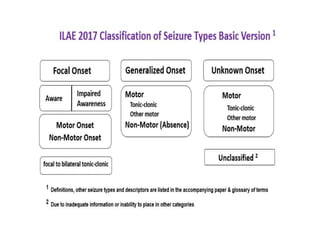
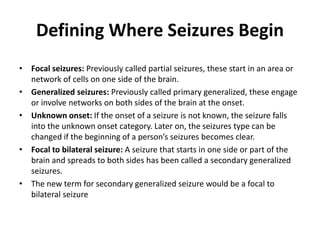
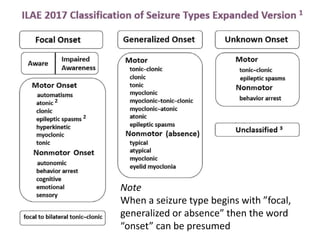
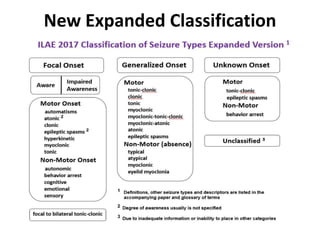
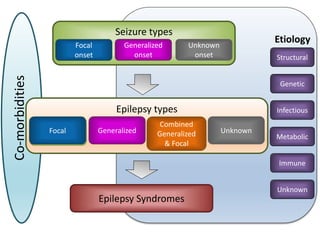
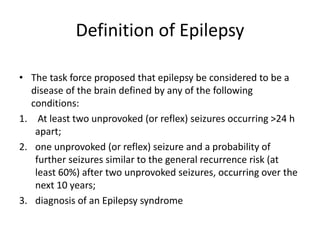
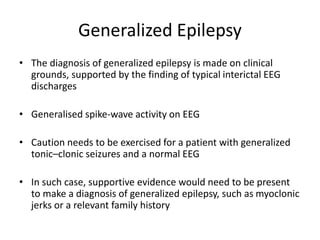
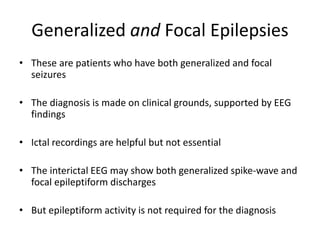
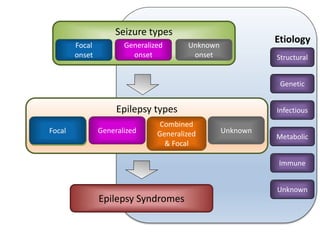
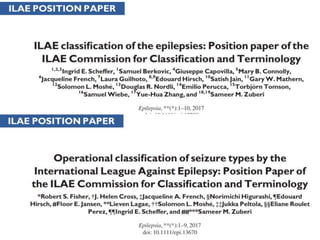
The document summarizes the 2017 revised classification of seizures by the International League Against Epilepsy (ILAE). The classification was updated to better reflect current understanding and includes the following key changes:
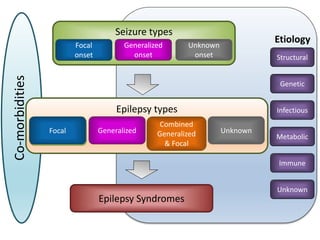
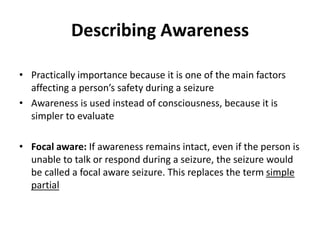
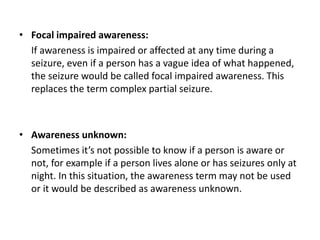
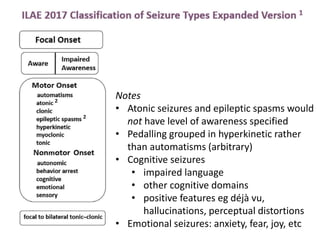
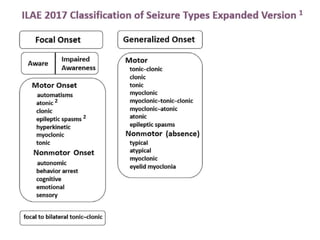
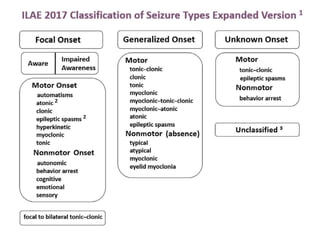
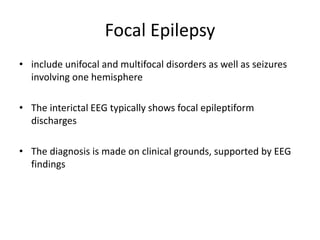
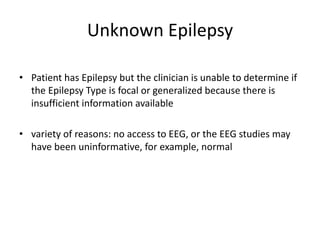
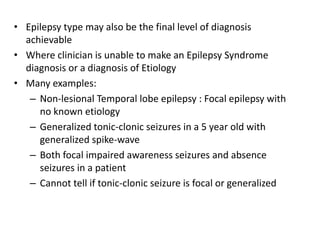
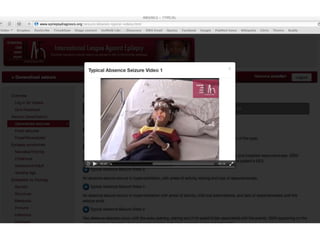
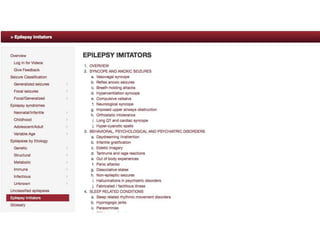
1. Seizures are classified based on where they begin in the brain, level of awareness during the seizure, and other features.
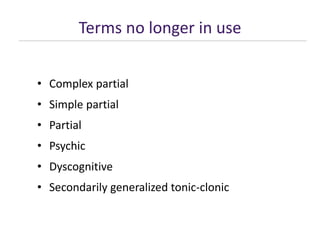
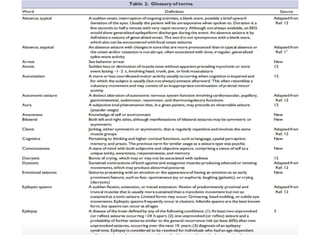
2. New terminology is introduced, such as "focal aware" and "focal impaired awareness" seizures instead of "simple partial" and "complex partial".
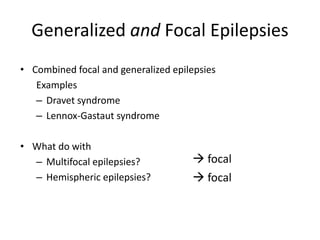
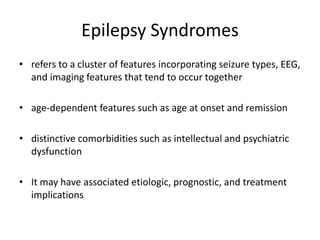
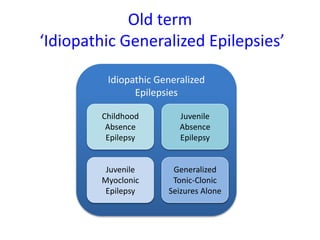
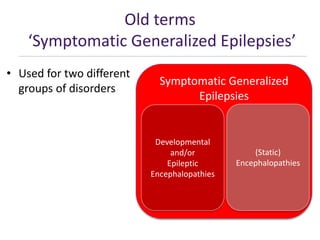
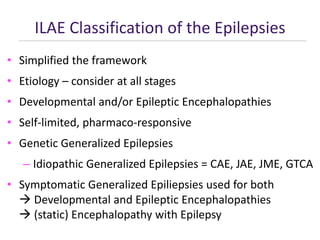
3. Epilepsy syndromes are defined as clusters of features rather than approved entities. Old terms like "idiopathic generalized epilepsies" are replaced.
4. The classification aims to be applicable