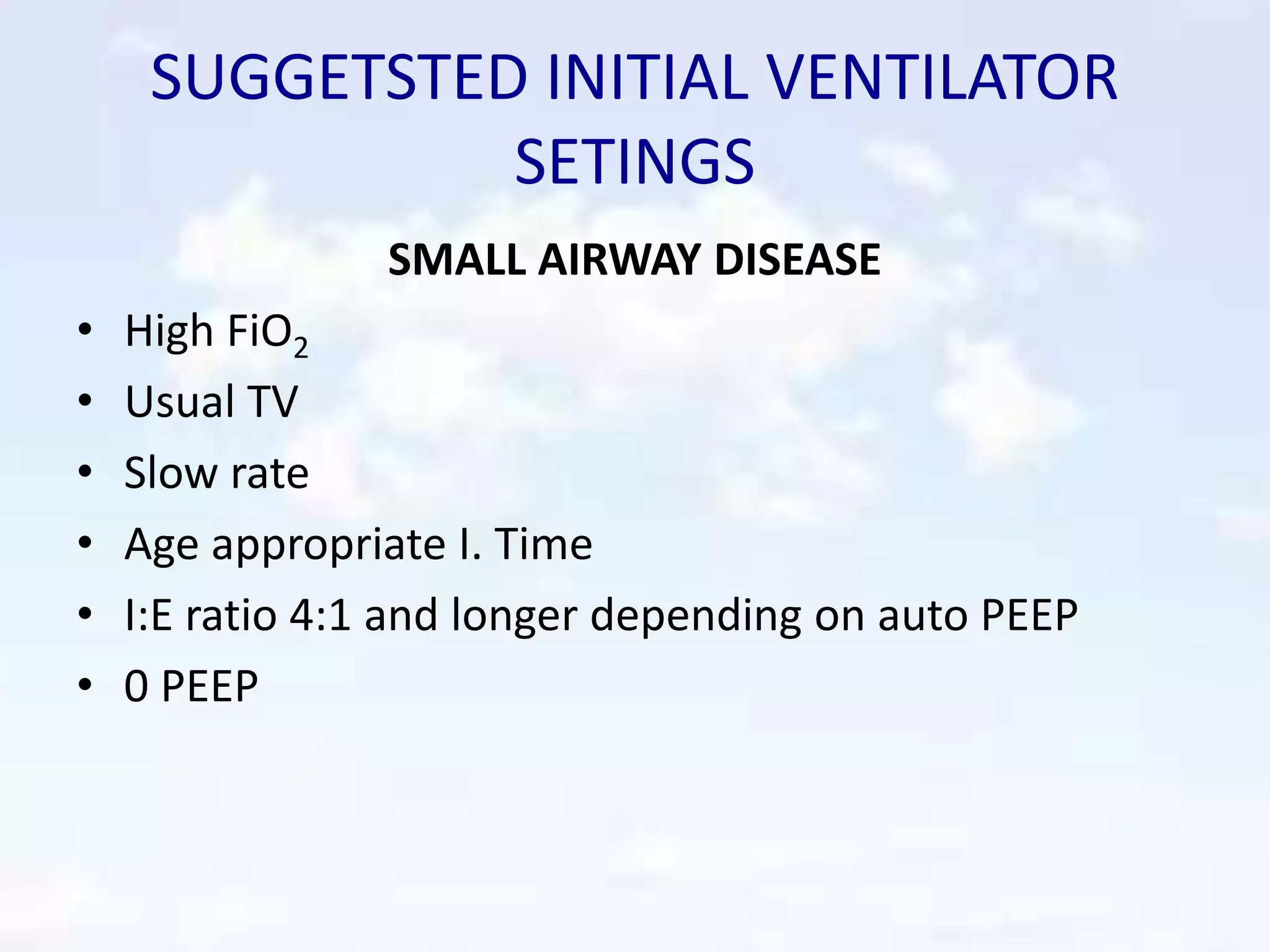
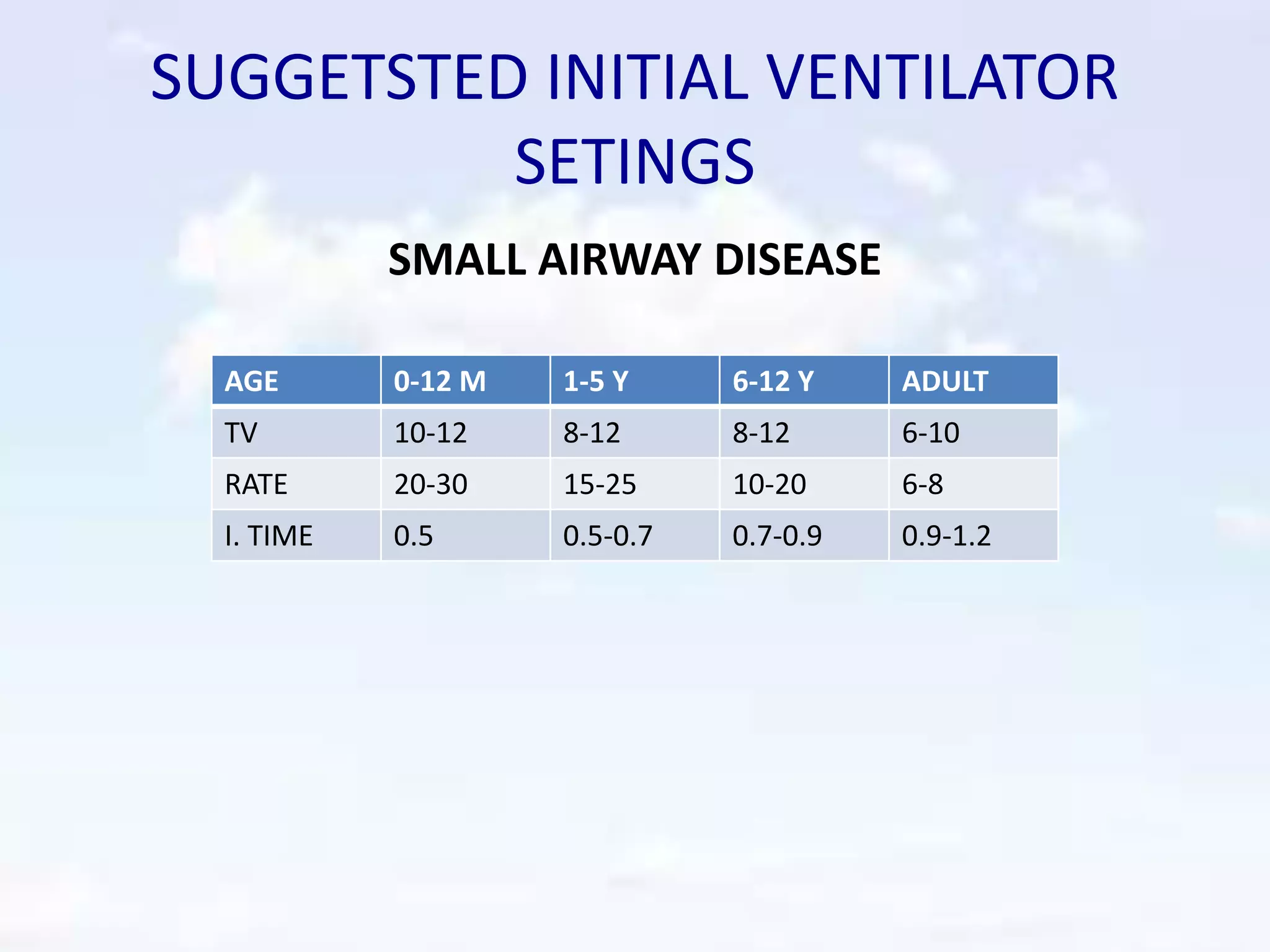
The document outlines the principles of conventional positive pressure ventilation (PPV) focusing on the respiratory system's function, the importance of gas exchange, and the management of respiratory failure. It describes various settings and modes of PPV, detailing considerations for initiating and adjusting ventilator settings based on specific patient conditions and responses. Additionally, it highlights the potential complications associated with ventilation and emphasizes the need for careful monitoring and weaning strategies.