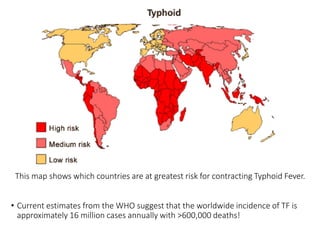
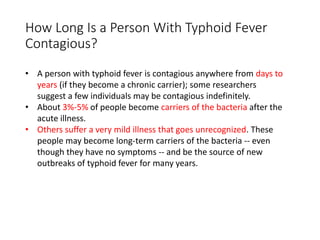
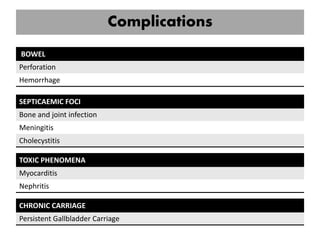
Enteric fever, including typhoid and paratyphoid fever, is caused by Salmonella typhi and Salmonella paratyphi bacteria, leading to significant global morbidity and mortality primarily through fecal-oral transmission via contaminated food and water. The disease is highly contagious, with symptoms including prolonged fever, abdominal pain, and potential complications such as bowel perforation; treatment with antibiotics is critical to reduce mortality rates. Current statistics indicate approximately 16 million cases annually worldwide, with a notable burden in developing countries, and concerns regarding antibiotic resistance are increasing.

![Diagnosis & Investigation
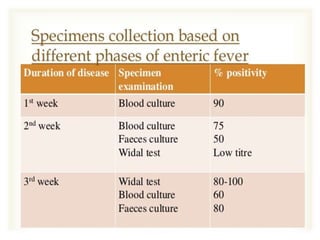
• Blood culture
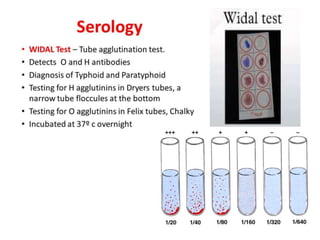
• Specific serologic test
Identify Salmonella antibodies / antigens
[ Fluorescent antibody study to look for
substances that are specific to Typhoid bacteria ]
Widal Test and ELISA
• Urine and Stool Culture (2nd & 3rd week)
• Marrow Culture *
- 90% sensitive unless until after 5 days
commencement of antibiotic
• Punch-biopsy samples of rose spots Culture
- 63% sensitive
• Clot culture
*culture may be obtained from CSF, peritoneal fluid,
mesenteric LNs, resected intestine, gallbladder,
pharynx, tonsils, abscess, bone](https://image.slidesharecdn.com/7-170521101930/85/Enteric-fever-typhoid-fever-16-320.jpg)


![Reference
• Davidson’s Principle and Practice of Medicine 22nd Edition
• Hutchison’s Clinical Methods 23rd Edition
• Medscape
• Mayo Clinic
• Emedicine Health
• Malaysian Journal of Microbiology
[http://mjm.usm.my/uploads/issues/313/Corrected%20proof%20M
JM%20475-12%20(ok).pdf]](https://image.slidesharecdn.com/7-170521101930/85/Enteric-fever-typhoid-fever-23-320.jpg)