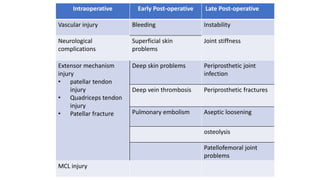
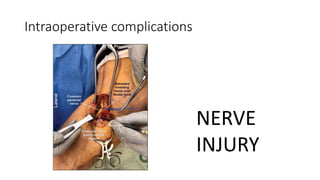
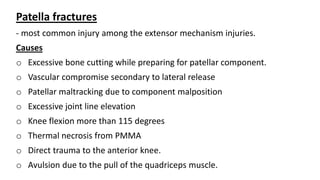
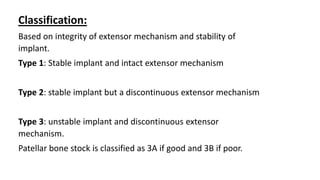
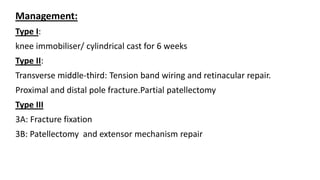
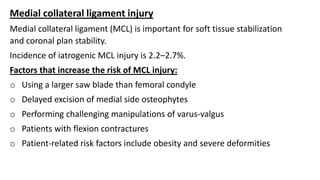
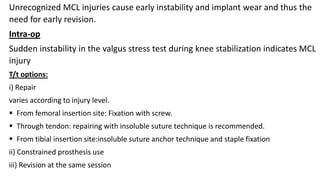
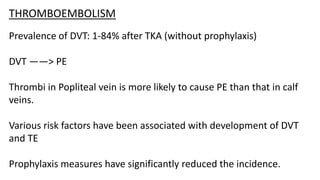
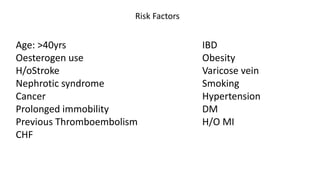
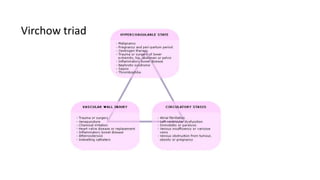
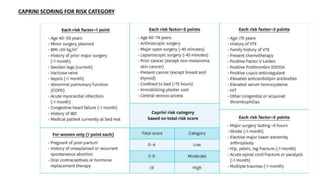
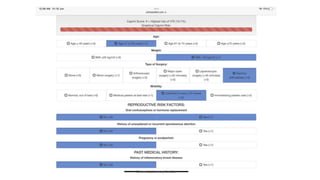
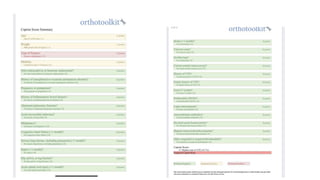
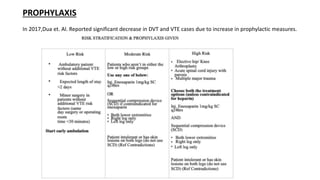
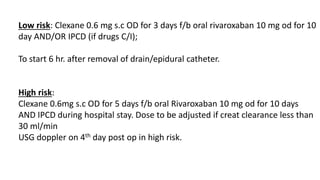
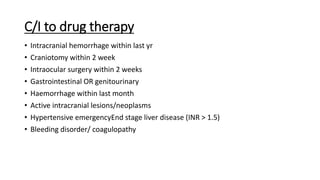
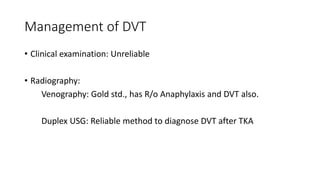
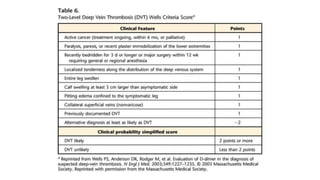
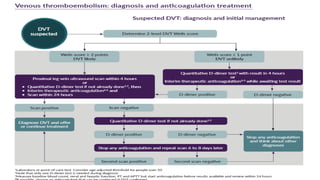
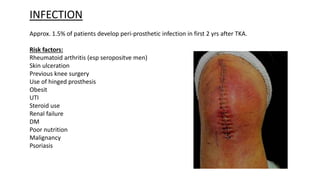
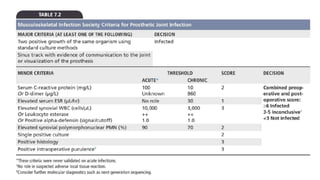
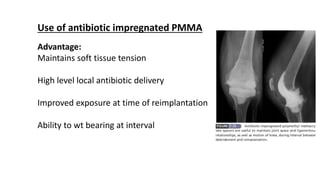
Total knee arthroplasty (TKA) can have various complications that are grouped into intraoperative, early postoperative, and late postoperative categories. Intraoperative complications include vascular injuries, neurological injuries, and injuries to the extensor mechanism. Early postoperative complications include bleeding, infections, deep vein thrombosis, and pulmonary embolism. Late complications involve issues like instability, stiffness, fractures around the prosthesis, loosening of the prosthesis, and patellofemoral joint problems. Careful surgical technique and appropriate preventative measures can help reduce the risk of complications from TKA.