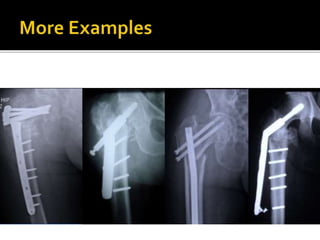
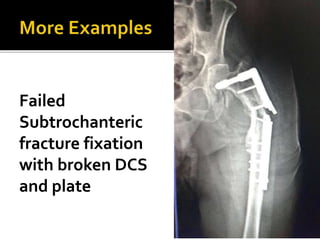
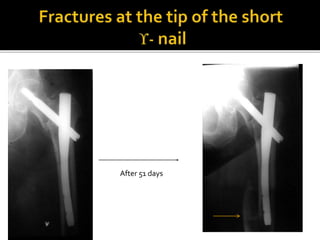
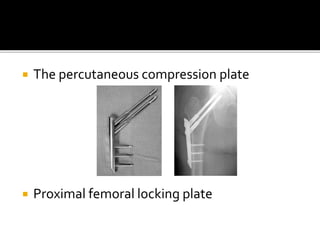
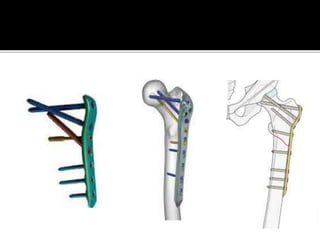
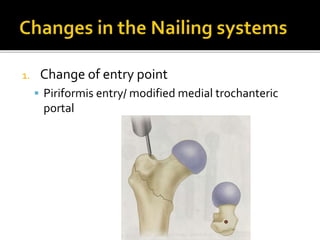
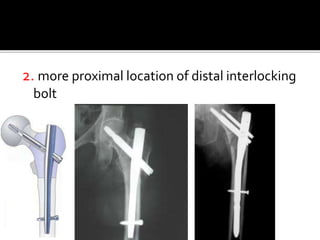
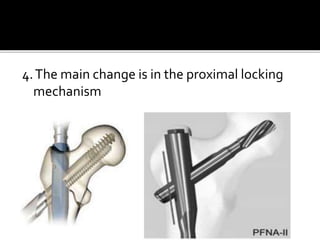
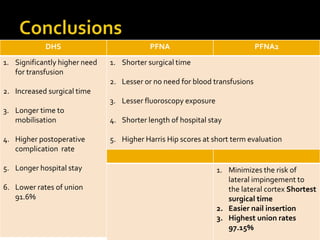
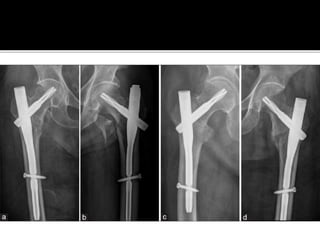
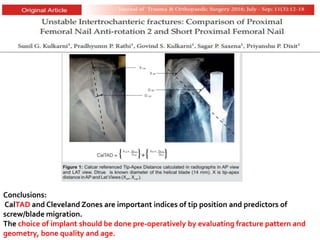
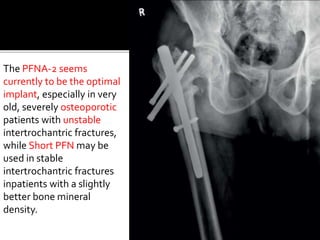
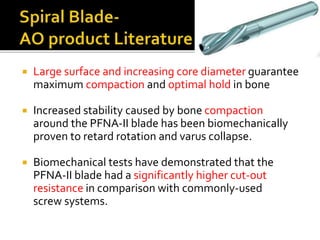
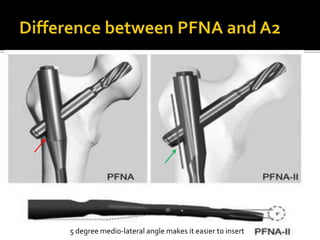
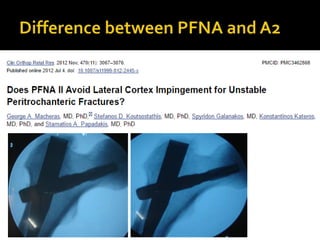
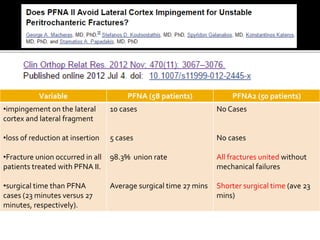
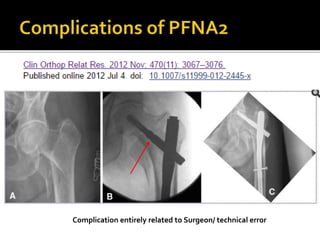
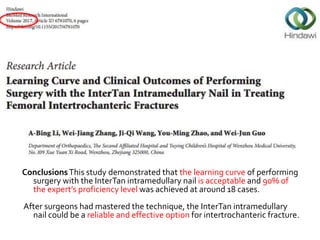
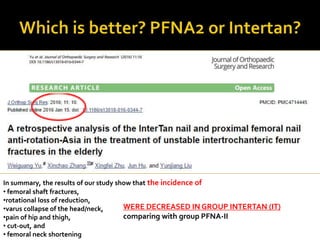
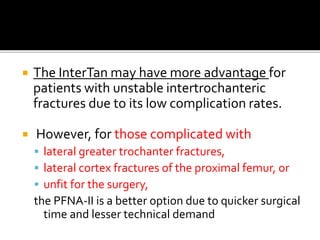
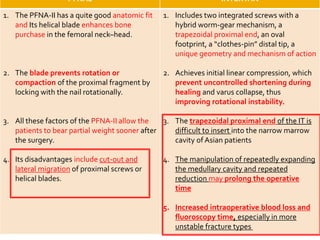
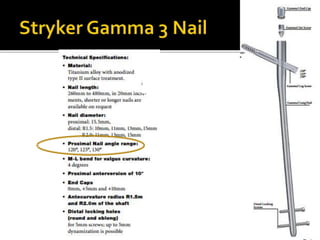
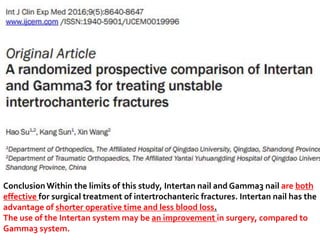
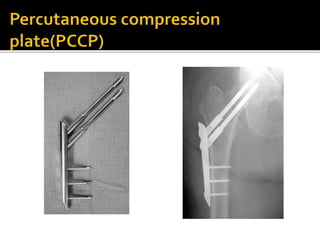
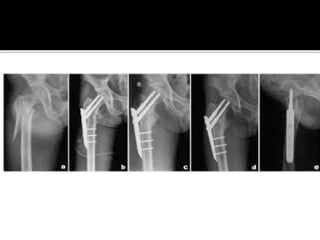
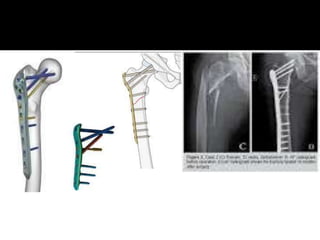
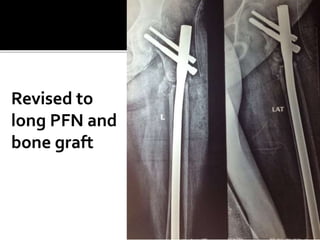
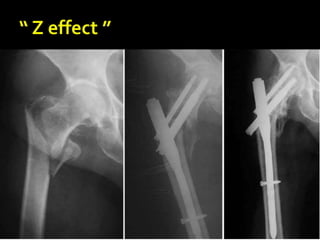
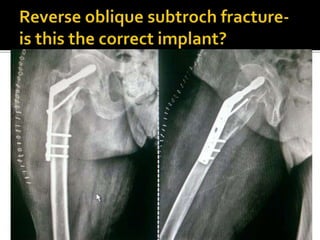
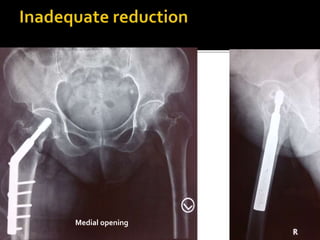
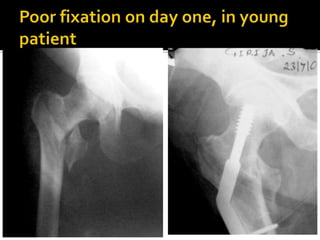
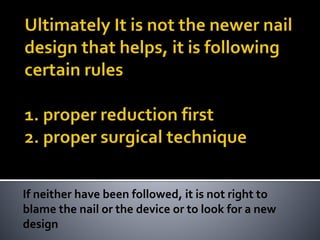
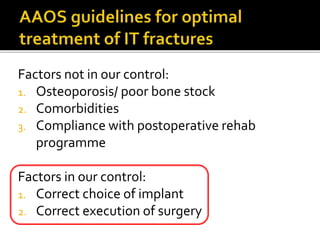
The document discusses advancements in the fixation of intertrochanteric fractures, emphasizing the advantages of intramedullary devices such as the Proximal Femoral Nail Antirotation II (PFNA-2) over traditional methods like Dynamic Hip Screws (DHS). It highlights improved surgical outcomes, including shorter surgical times, lower complication rates, and higher union rates with PFNA-2, while noting the importance of surgical technique in preventing complications. Overall, it concludes that PFNA-2 is a promising choice for unstable intertrochanteric fractures, particularly in elderly patients, although further research is recommended.