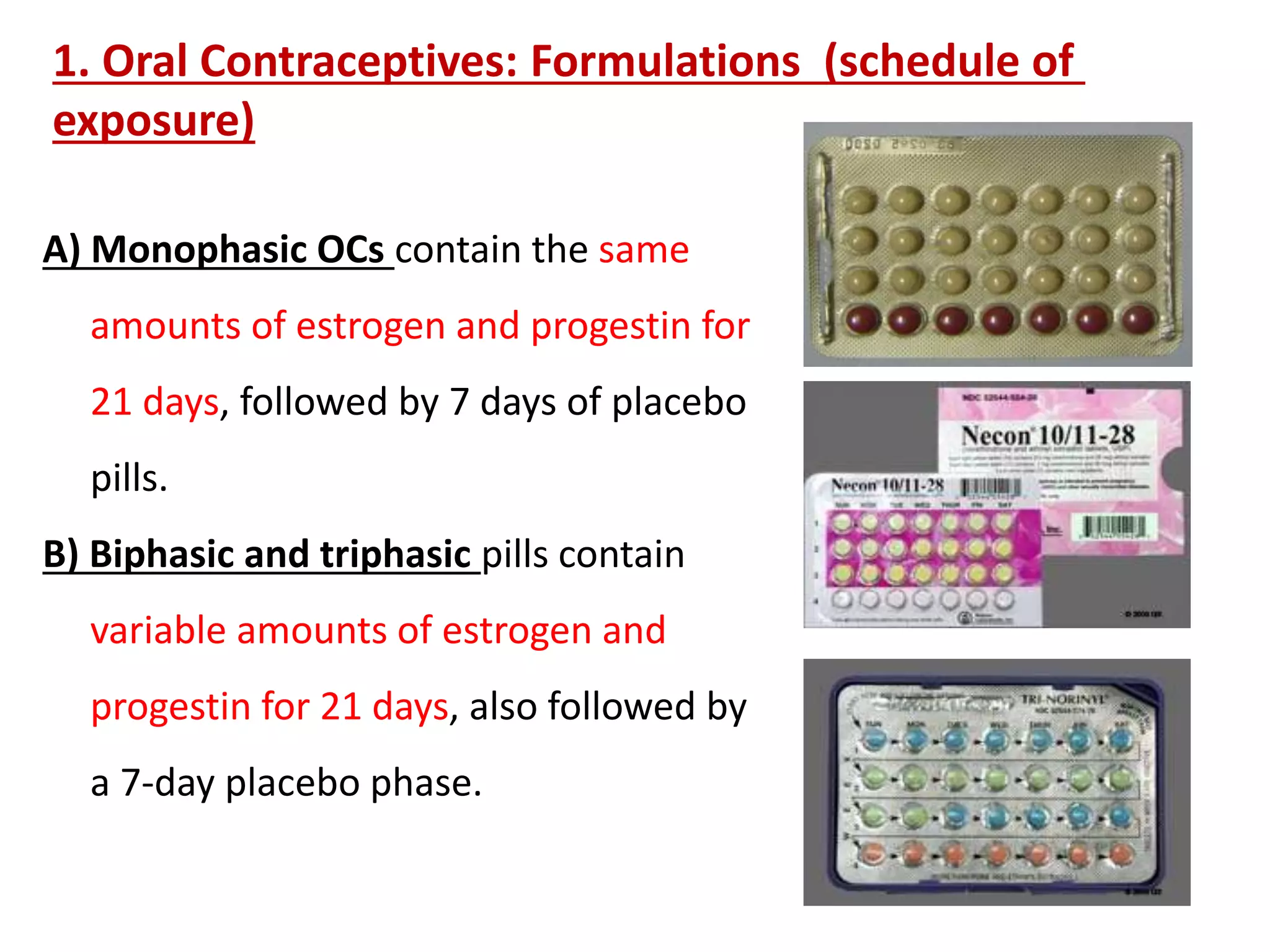
This document outlines various methods of contraception, including barrier methods like condoms and diaphragms, as well as hormonal methods like oral contraceptives, transdermal patches, injectables, and emergency contraception. It describes the formulations and mechanisms of different hormonal contraceptives, such as monophasic and triphasic oral contraceptives that contain constant or varying levels of estrogen and progestin, extended cycle pills, and progestin-only mini pills. Long acting reversible contraceptives like the contraceptive implant and intrauterine device are also discussed.