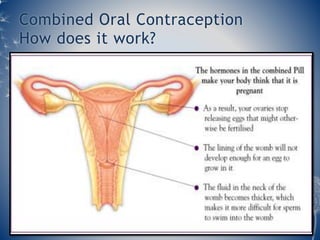
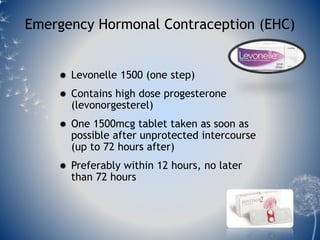
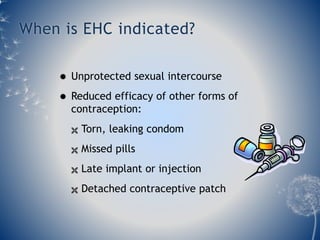
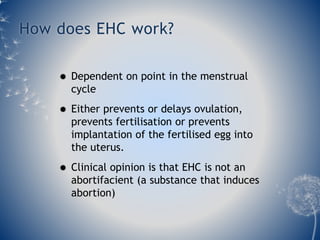
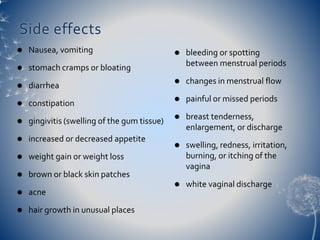
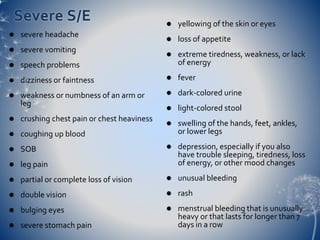
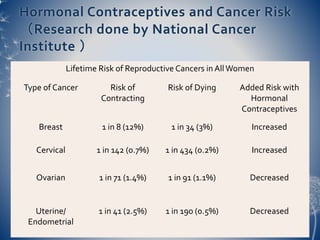
This document discusses hormonal contraceptives, including combined oral contraceptives containing estrogen and progesterone, progestogen-only pills, and emergency hormonal contraception. It describes how each method works, directions for use, effectiveness, and potential side effects. Hormonal contraceptives are widely used birth control methods that are convenient and reversible. When taken properly, combined oral contraceptives are over 99% effective in preventing pregnancy. The document also summarizes research on the cancer risks associated with hormonal contraceptive use.