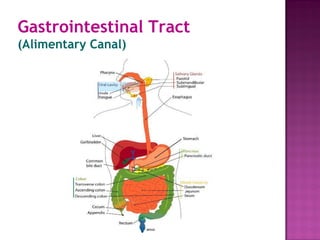
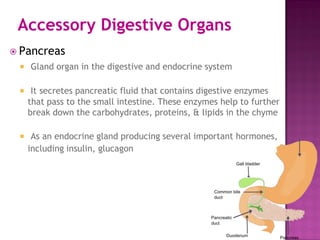
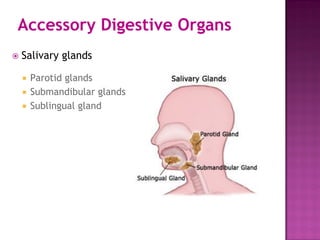
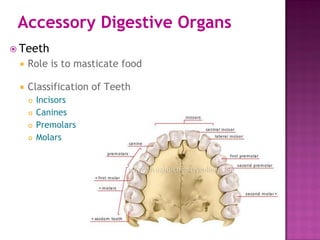
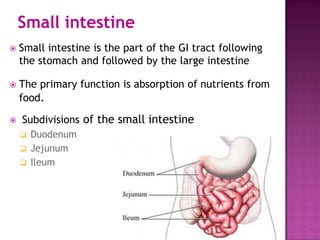
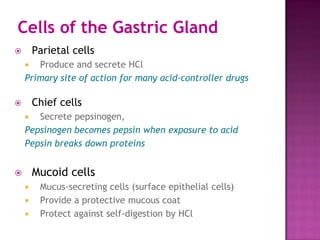
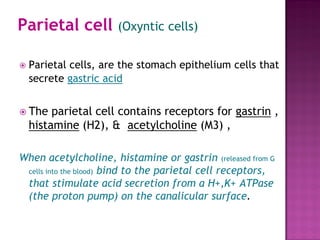
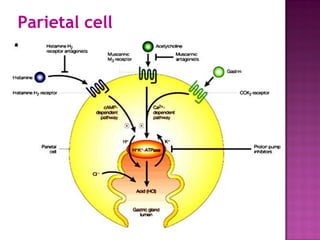
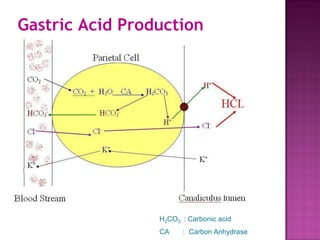
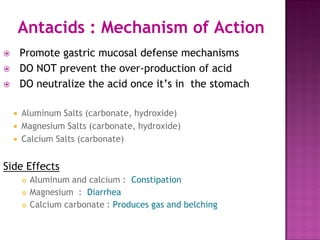
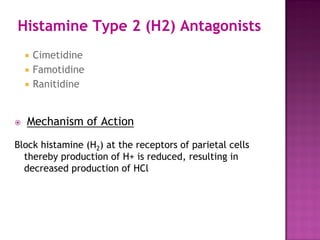
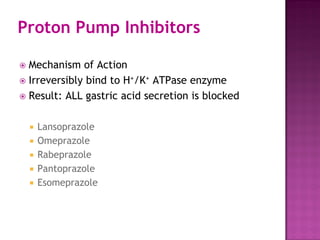
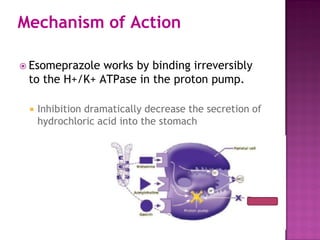
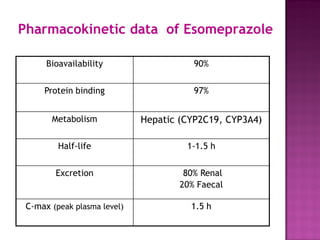
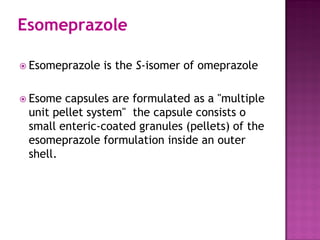
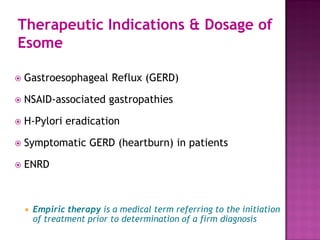
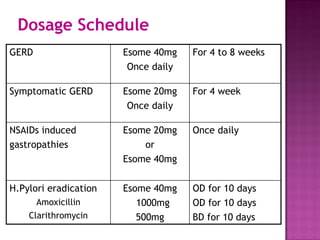
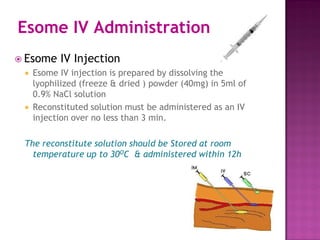
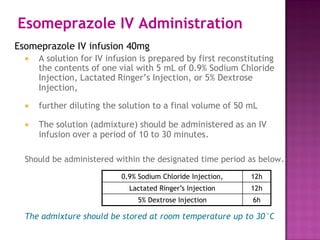
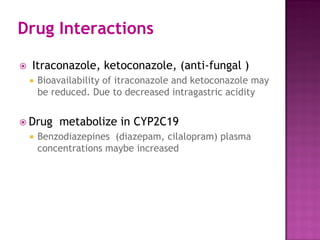
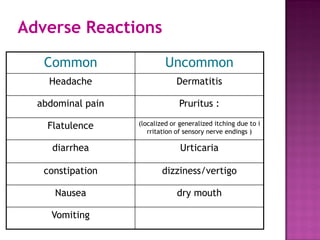
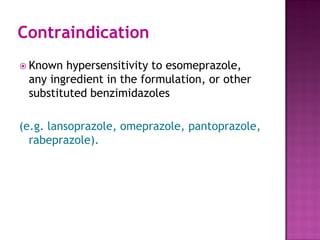
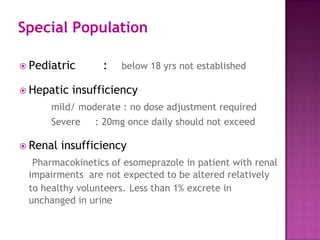
The document provides a detailed overview of the gastrointestinal tract and its associated organs, including the anatomy and functions of the mouth, stomach, small and large intestines, and accessory digestive organs such as the pancreas and liver. It discusses the roles of various cells in the stomach, mechanisms of gastric acid secretion, and compares different acid-controlling agents like antacids, H2 antagonists, and proton pump inhibitors, focusing specifically on esomeprazole. Therapeutic indications, dosage recommendations, and potential drug interactions and contraindications for esomeprazole are also highlighted.