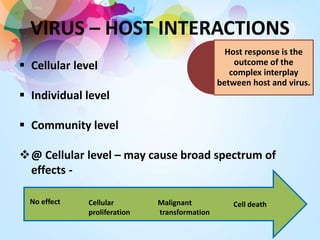
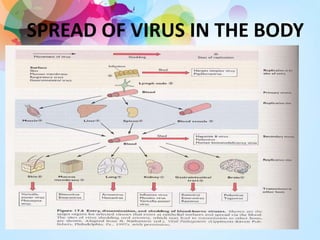
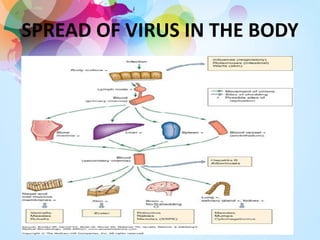
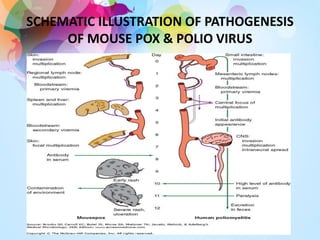
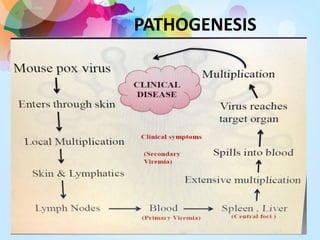
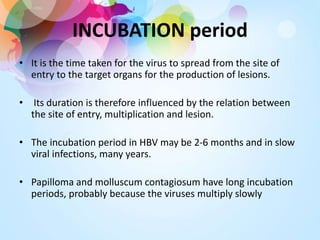
1. The document discusses virus-host interactions at the cellular, individual, and community levels and the various effects viruses can have on cells, including no effect, proliferation, malignant transformation, and cell death.
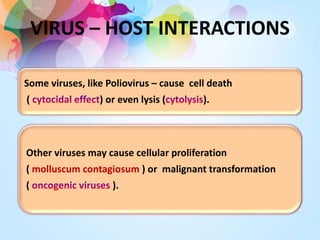
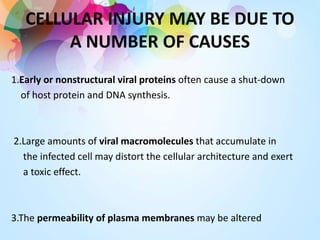
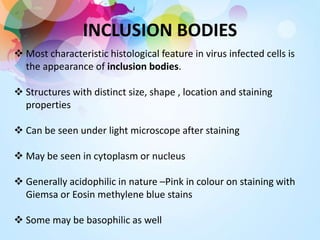
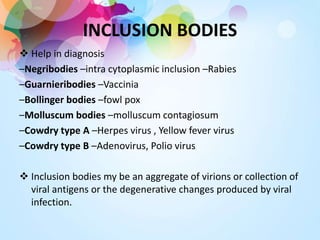
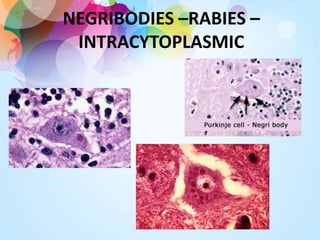
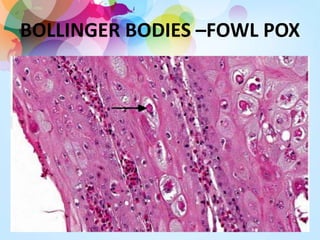
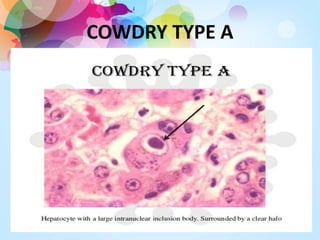
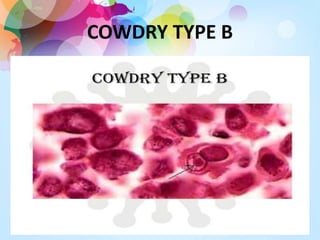
2. It describes how viruses like poliovirus cause cell death or lysis, while others cause proliferation or malignant transformation. Cellular injury may be caused by viral proteins, accumulation of viral molecules, altered membranes and chromosomes, fusion of adjacent cells, inclusion bodies, and viral antigens on the cell surface.
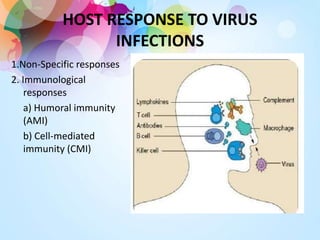
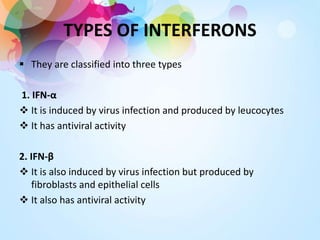
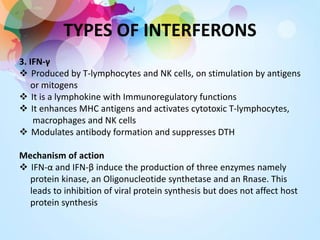
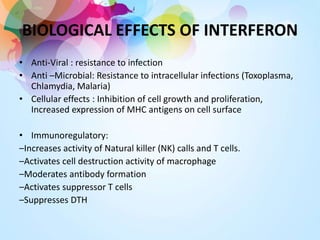
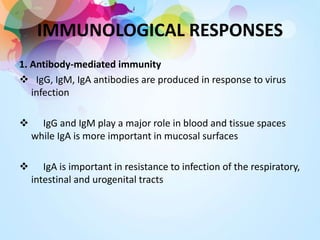
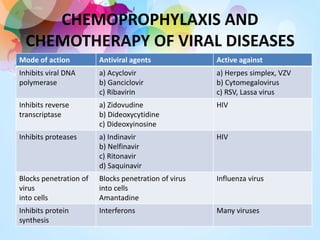
3. The host response involves non-specific responses like fever and interferons as well as immune responses through antibodies and cell-mediated immunity which work to neutralize viruses, opsonize them for destruction