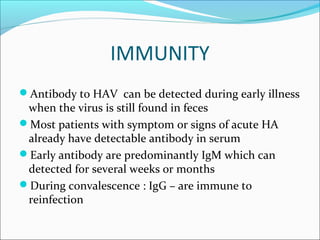
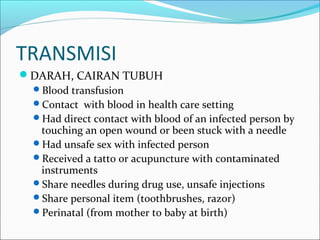
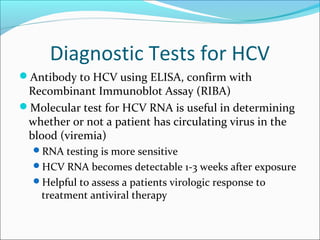
This document provides information on various types of hepatitis. It discusses hepatitis A, B, C, D, and E. Key points include: hepatitis A is transmitted fecal-orally and does not cause chronic infection; hepatitis B can become chronic and is transmitted through blood/bodily fluids; hepatitis C often becomes chronic and is transmitted through blood exposure; hepatitis D requires hepatitis B for transmission; and hepatitis E is transmitted fecal-orally similar to hepatitis A and does not cause chronic infection. The document also outlines symptoms, diagnostic tests, treatment options, and prevention measures for each type of viral hepatitis.