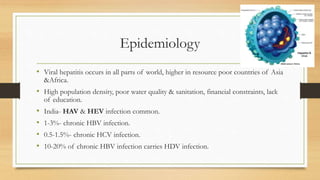
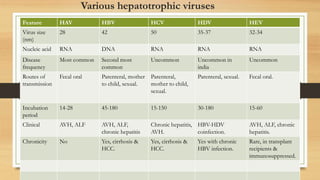
This document discusses hepatitis, primarily caused by five hepatotropic viruses - hepatitis A, B, C, D, and E viruses. Hepatitis A virus and hepatitis B virus are the most common causes of acute viral hepatitis in children in India. Most cases of acute viral hepatitis improve spontaneously without treatment. Prolongation of prothrombin time is a reliable laboratory marker of worsening liver function or potential liver failure. Chronic infection with hepatitis B or C can potentially lead to chronic hepatitis.
![Introduction
• Acute hepatitis- Inflammatory disorder of liver, usually associated with complete clinical &
histological recovery within 4 to 6 weeks.
• Children most commonly caused by hepatotrophic viruses, followed by drugs & metabolic
liver diseases.
• Acute viral hepatitis- self limited mild disease, does not require any active treatment.
• Sometimes leads to fulminant hepatitis & may need liver transplantation.
• Infection with Hepatotropic viruses [HAV, HBV, HCV, HDV, HEV].
• Non Hepatotropic viruses- mumps, measles, rubella, CMV, HSV, VZV, Dengue virus.
• Salmonella typhi, Plasmodium.
• Drugs- ATT, Antiepileptics, Halothane.
• Autoimmune Hepatitis.](https://image.slidesharecdn.com/viralhepatitis-170503130730/85/Viral-hepatitis-2-320.jpg)
![• Acute viral hepatitis- HAV, HEV.
• Chronic viral hepatitis- [>6months]- HBV,HCV,HDV.](https://image.slidesharecdn.com/viralhepatitis-170503130730/85/Viral-hepatitis-3-320.jpg)

![• Hepatitis B virus
• HBV[ DNA virus ], enters into hepatocyte nucleus .
• Integrates with host DNA- forms covalently closed circular DNA
(cccDNA).
• cccDNA remains inside the body for rest of life- Chronic HBV
infection.](https://image.slidesharecdn.com/viralhepatitis-170503130730/85/Viral-hepatitis-11-320.jpg)