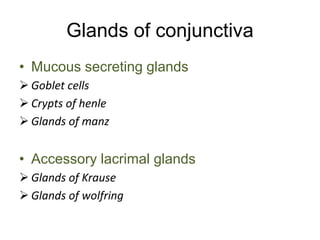
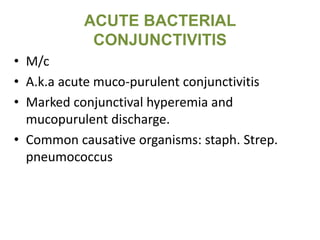
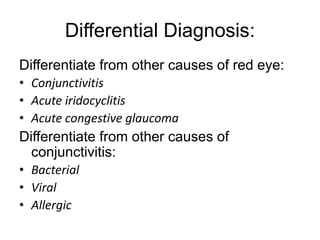
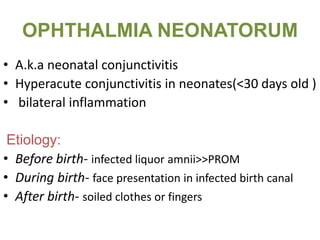
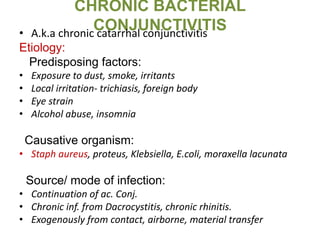
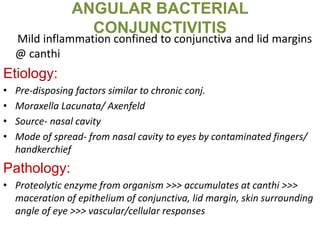
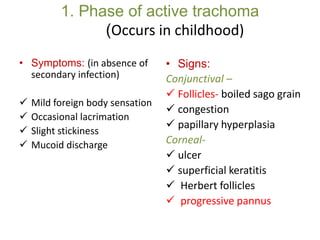
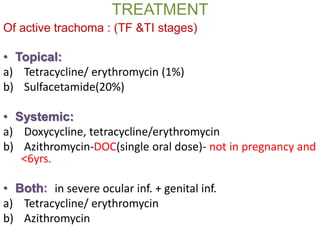
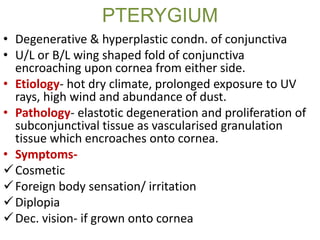
This document provides information on diseases of the conjunctiva. It discusses the various types of conjunctivitis including bacterial, viral, allergic, and trachoma. It describes the clinical features, causes, treatment, and complications of acute bacterial conjunctivitis, gonococcal conjunctivitis, ophthalmia neonatorum, chronic bacterial conjunctivitis, angular bacterial conjunctivitis, vernal keratoconjunctivitis, pinguecula, and pterygium. The document is an extensive overview of conjunctival diseases and their management.