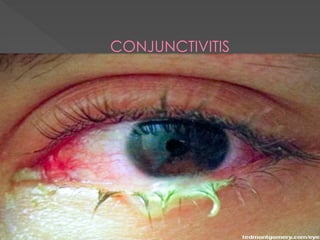
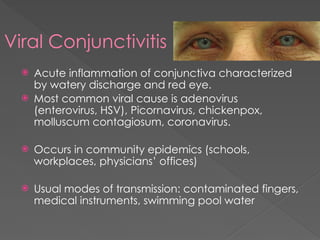
Conjunctivitis, inflammation of the conjunctiva, can be classified into viral, bacterial, and allergic types, each with distinct symptoms and causes. Viral conjunctivitis is highly contagious, commonly caused by adenoviruses, presenting with red eyes and watery discharge, while bacterial conjunctivitis often presents with purulent discharge and may require antibiotic treatment. Allergic conjunctivitis typically features itching and redness and is commonly associated with seasonal allergies, with management focused on allergen avoidance and symptomatic relief.
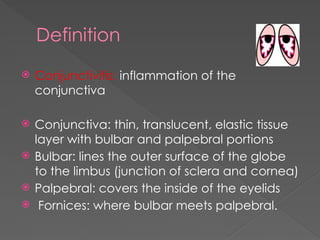





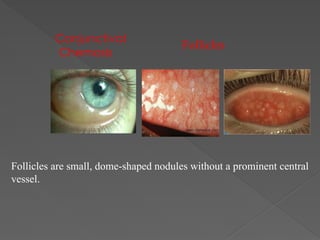






![Signs and Symptoms
Follicles on the inflamed conjunctiva
Discharge: More purulent than in viral conjunctivitis, with more
mattering (generally white or yellow mucous discharge [green in
some cases]) of the eyelid margins and greater associated
difficulty opening the eyelids following sleep; patients waking up
with their eyes “glued” shut.
Enlarged preauricular lymph node: Unusual in bacterial
conjunctivitis but found in severe conjunctivitis caused by N
gonorrhoeae
Eyelid edema: Often present in bacterial conjunctivitis, but mild
in most cases; severe eyelid edema in the presence of purulent
discharge raises the suspicion of N gonorrhoeae infection](https://image.slidesharecdn.com/conjunctivitis-241107120147-f74aed61/85/Conjunctivitis-pptx-21-320.jpg)