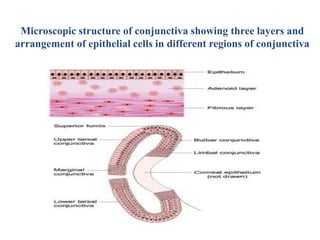
1. The document discusses conjunctivitis, specifically describing the anatomy of the conjunctiva and types of bacterial conjunctivitis.
2. It defines conjunctivitis as inflammation of the conjunctiva and describes the etiological classification including infective, allergic, irritative, and others.
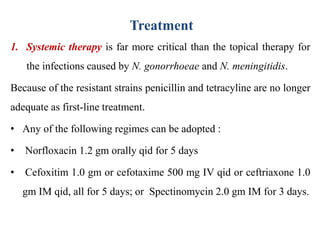
3. The most common type of acute bacterial conjunctivitis is acute mucopurulent conjunctivitis, which presents with conjunctival hypermia and mucopurulent discharge. Common causes are Staphylococcus aureus and Haemophilus influenzae.