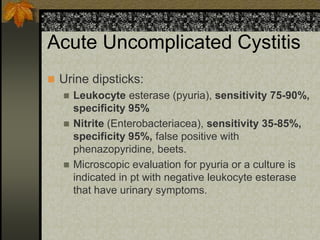
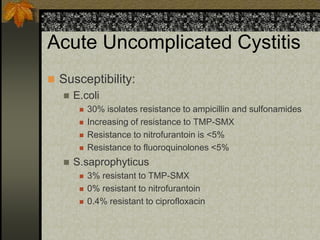
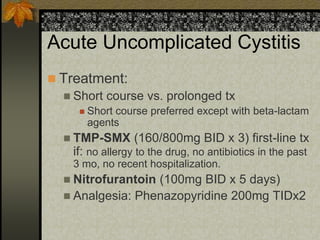
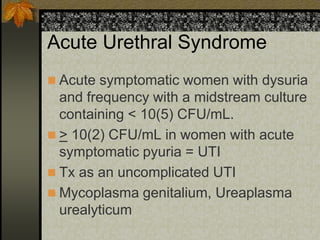
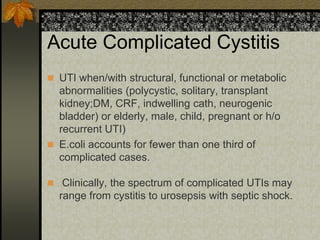
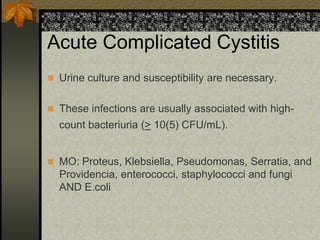
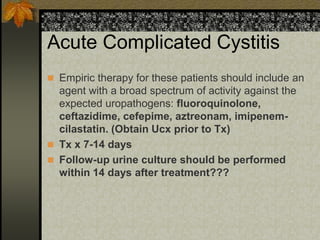
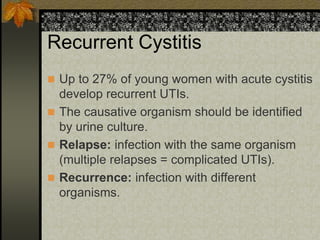
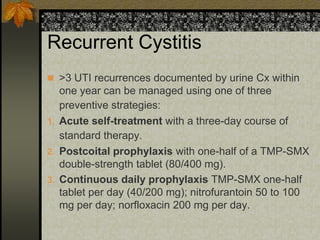
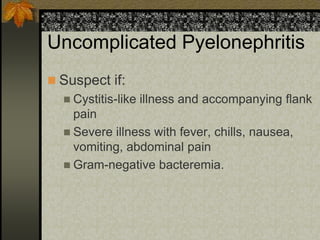
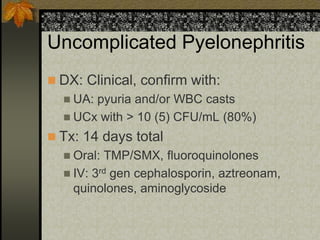
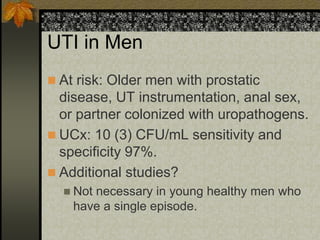
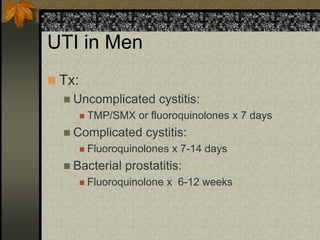
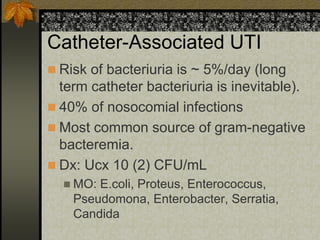
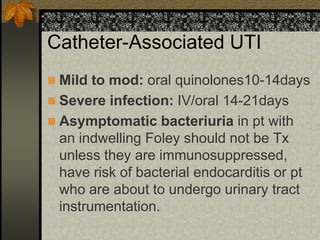
Urinary tract infections are a common problem that affect both women and men. They range from uncomplicated cystitis to complicated infections involving the kidneys or structural abnormalities. Common causes include E. coli and symptoms include dysuria, frequency, and urgency. Treatment involves antibiotics like TMP-SMX or fluoroquinolones depending on severity and recurrence risk. Recurrent infections require long term prophylaxis in some cases.