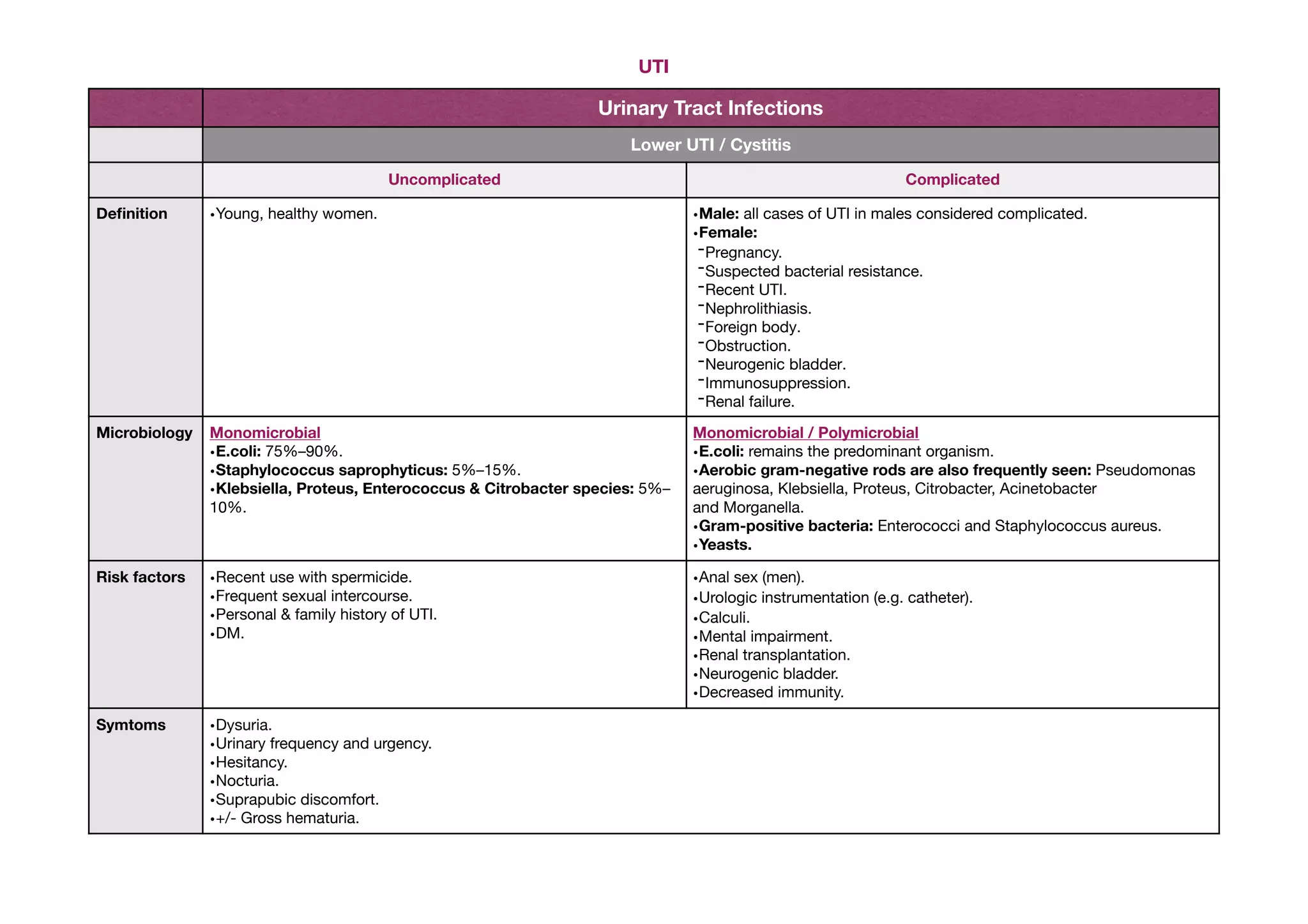
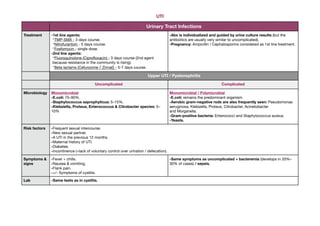
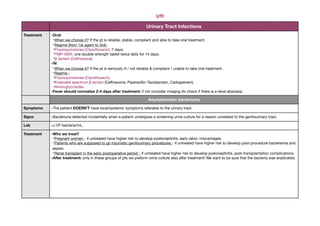
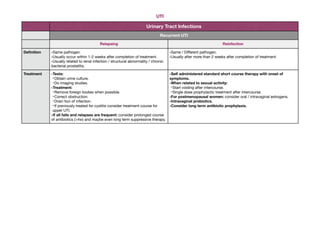
This document summarizes urinary tract infections (UTIs). It describes the differences between lower and upper UTIs, as well as uncomplicated and complicated cases. It provides details on microbiology, risk factors, symptoms, diagnosis and treatment for cystitis, pyelonephritis, asymptomatic bacteriuria, and recurrent UTIs. Treatment involves antibiotics like TMP-SMX, fluoroquinolones, and beta-lactams. Diagnosis involves urine dipstick, microscopy and culture. Recurrent infections may be due to structural issues and require imaging and long-term antibiotic treatment or suppression.