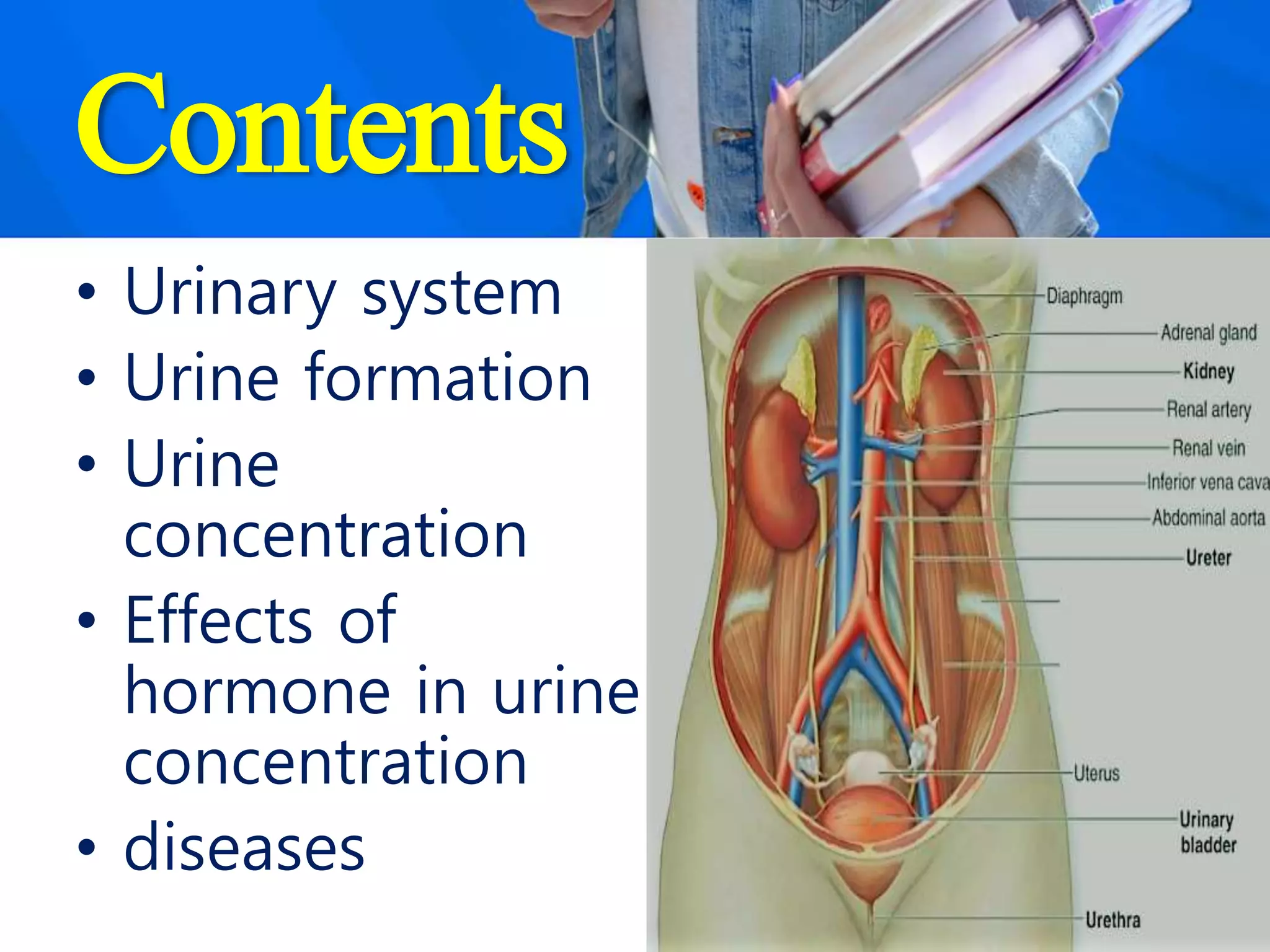
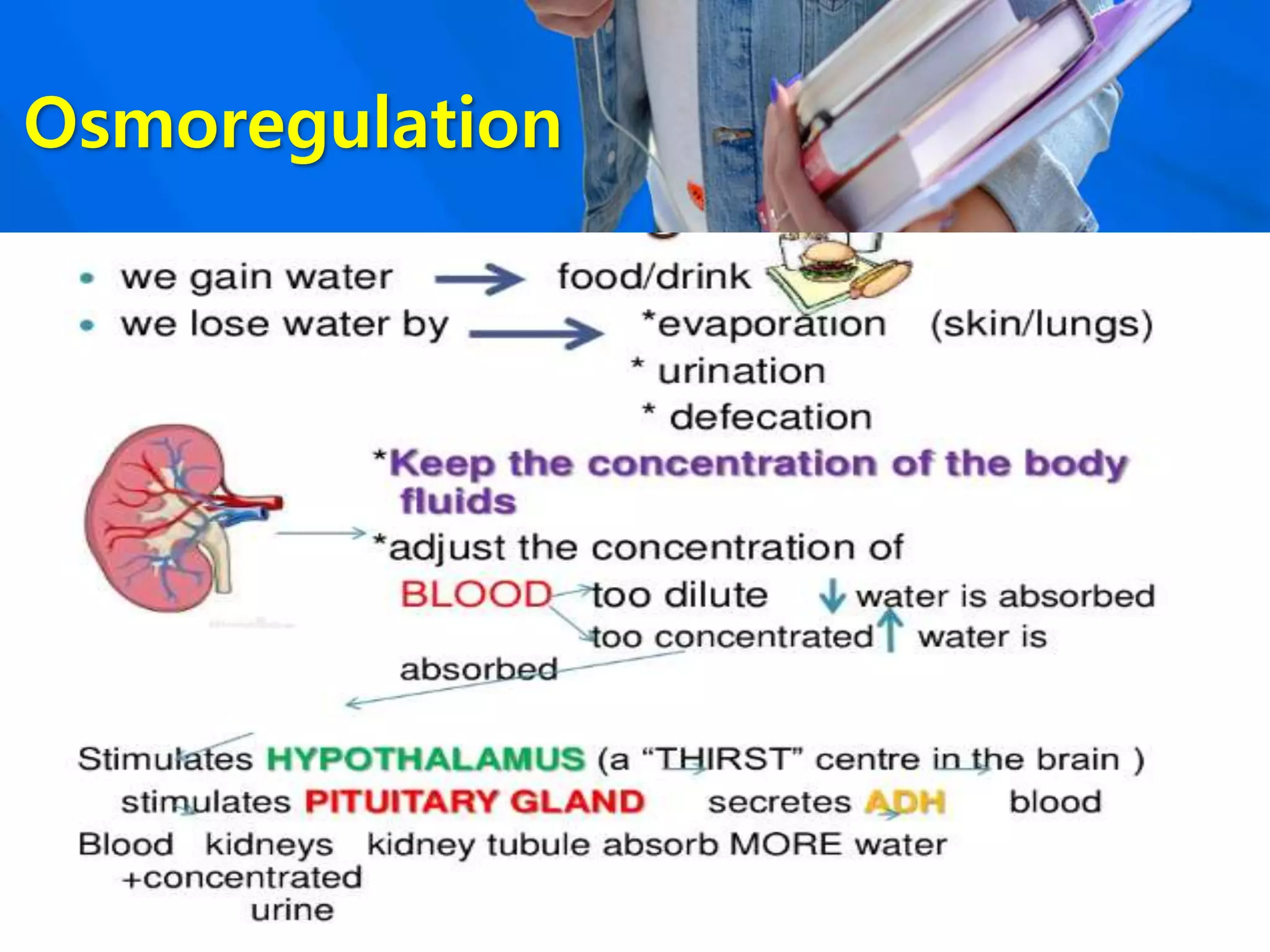
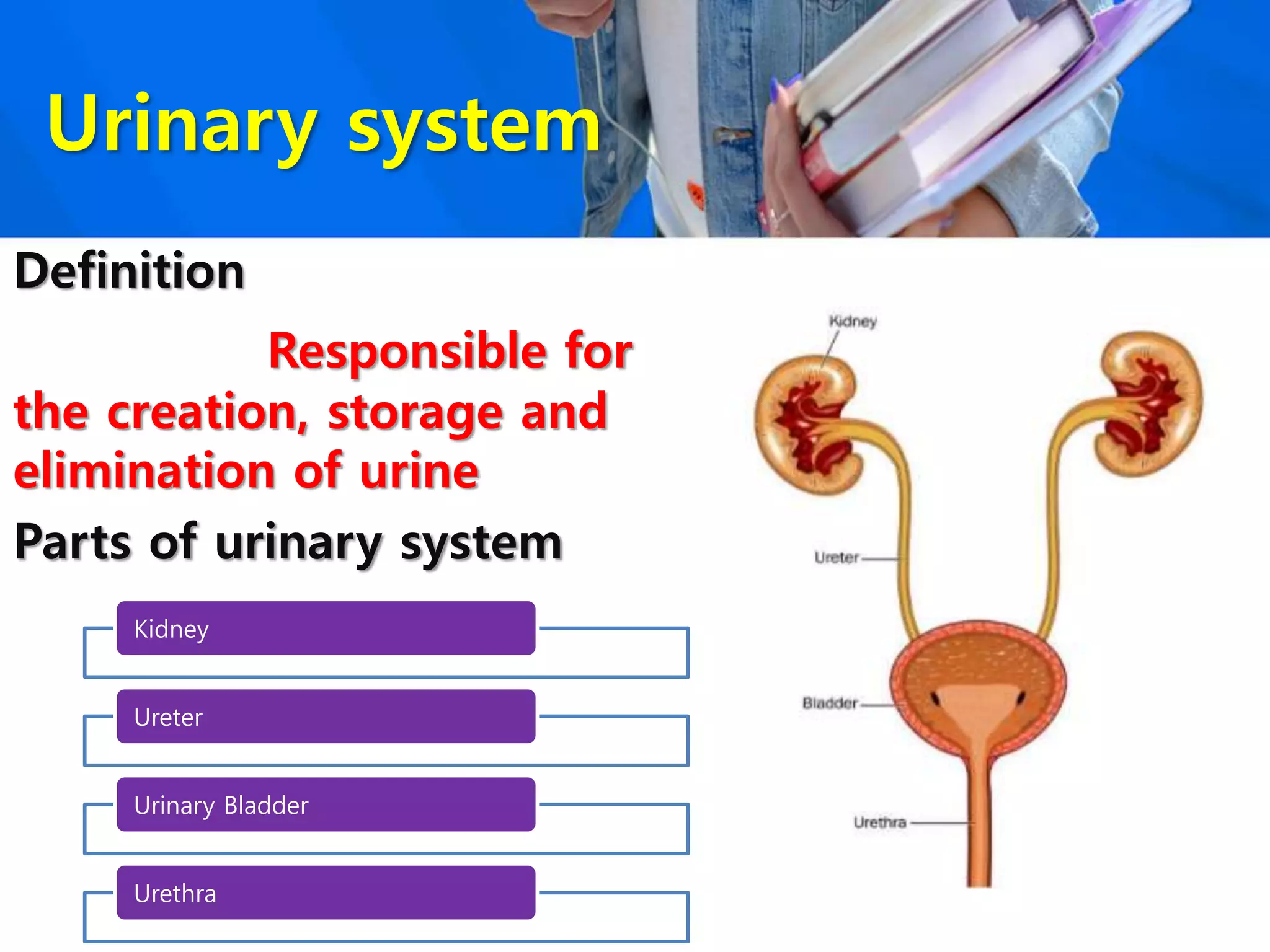
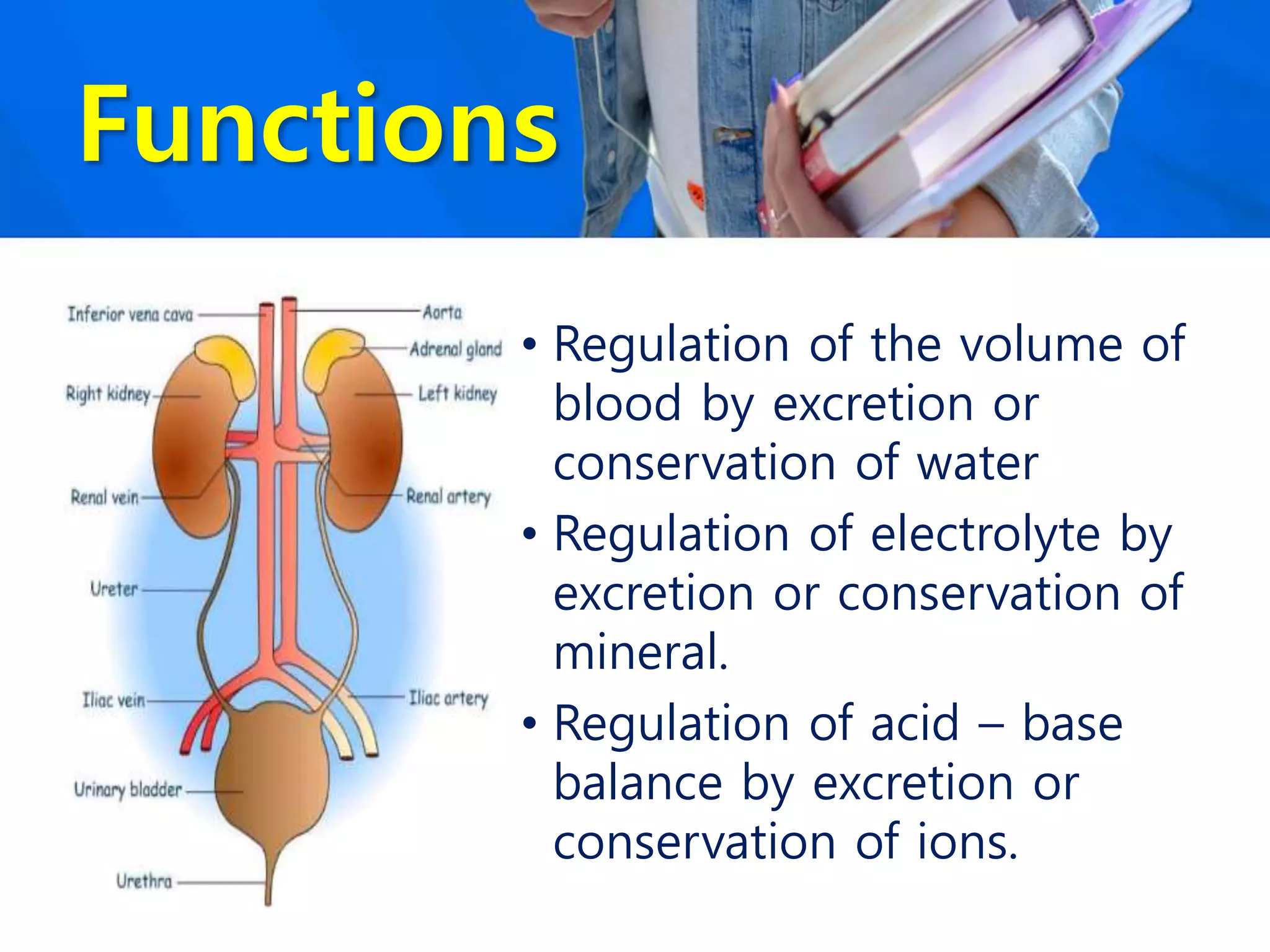
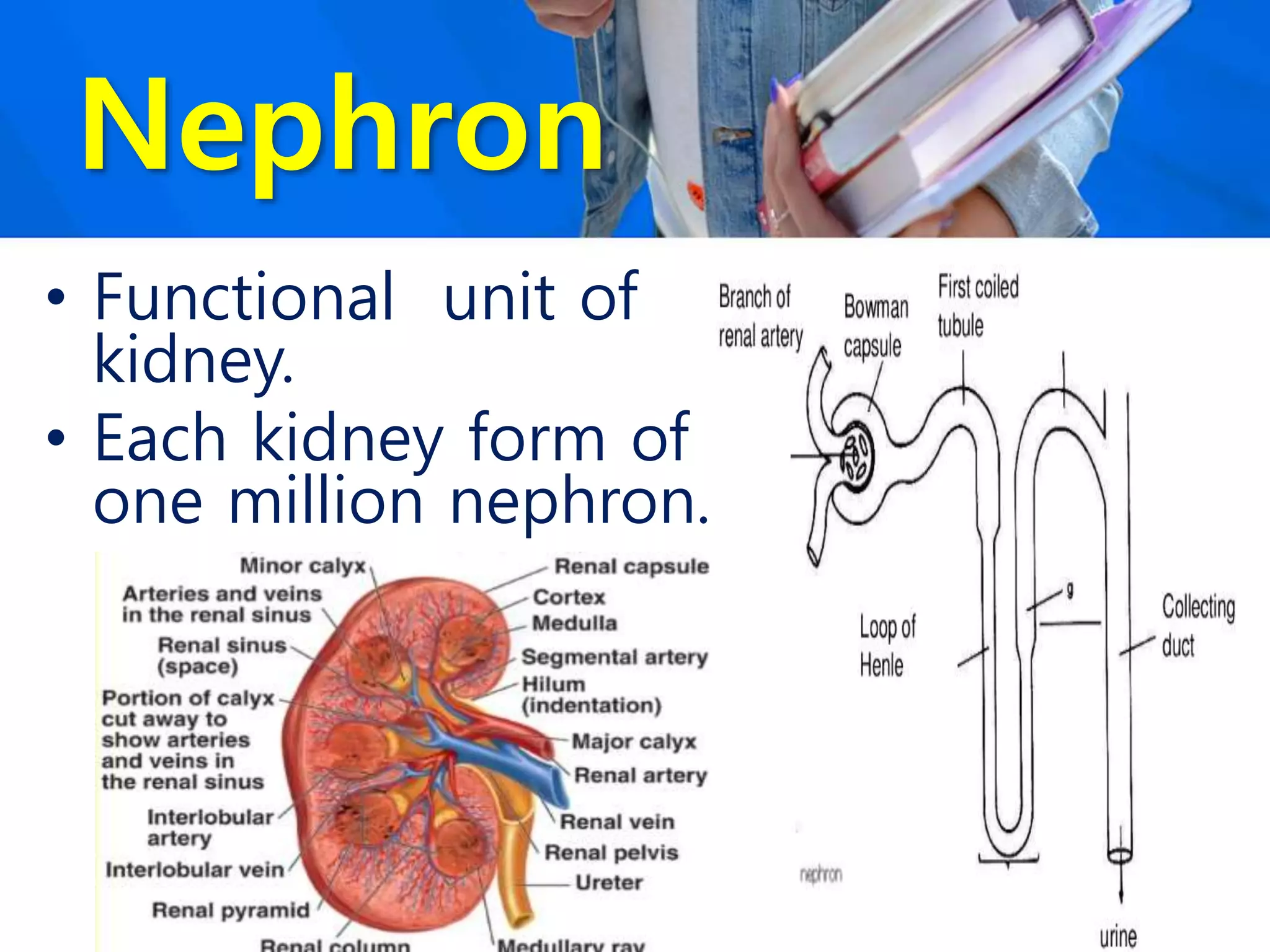
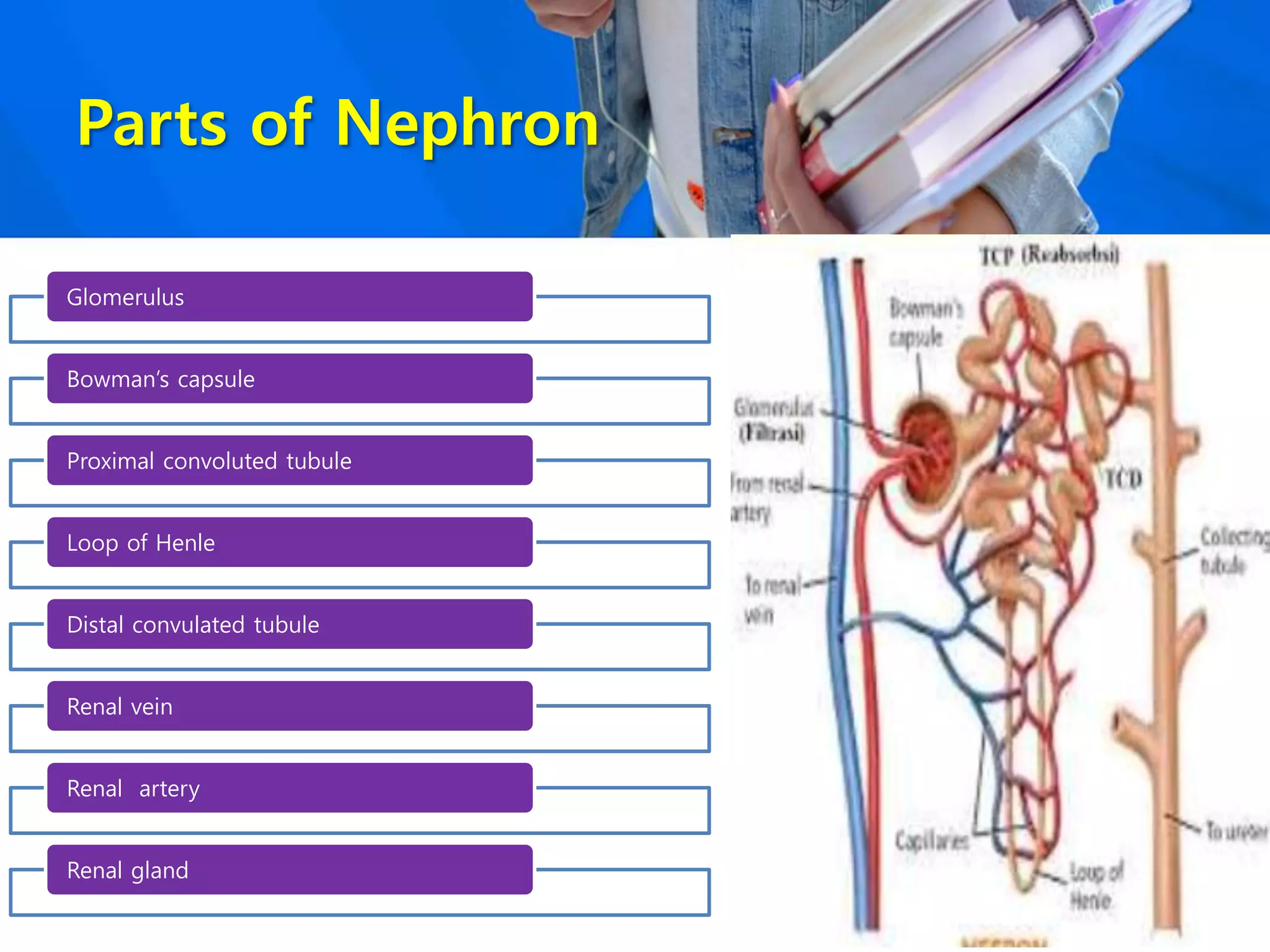
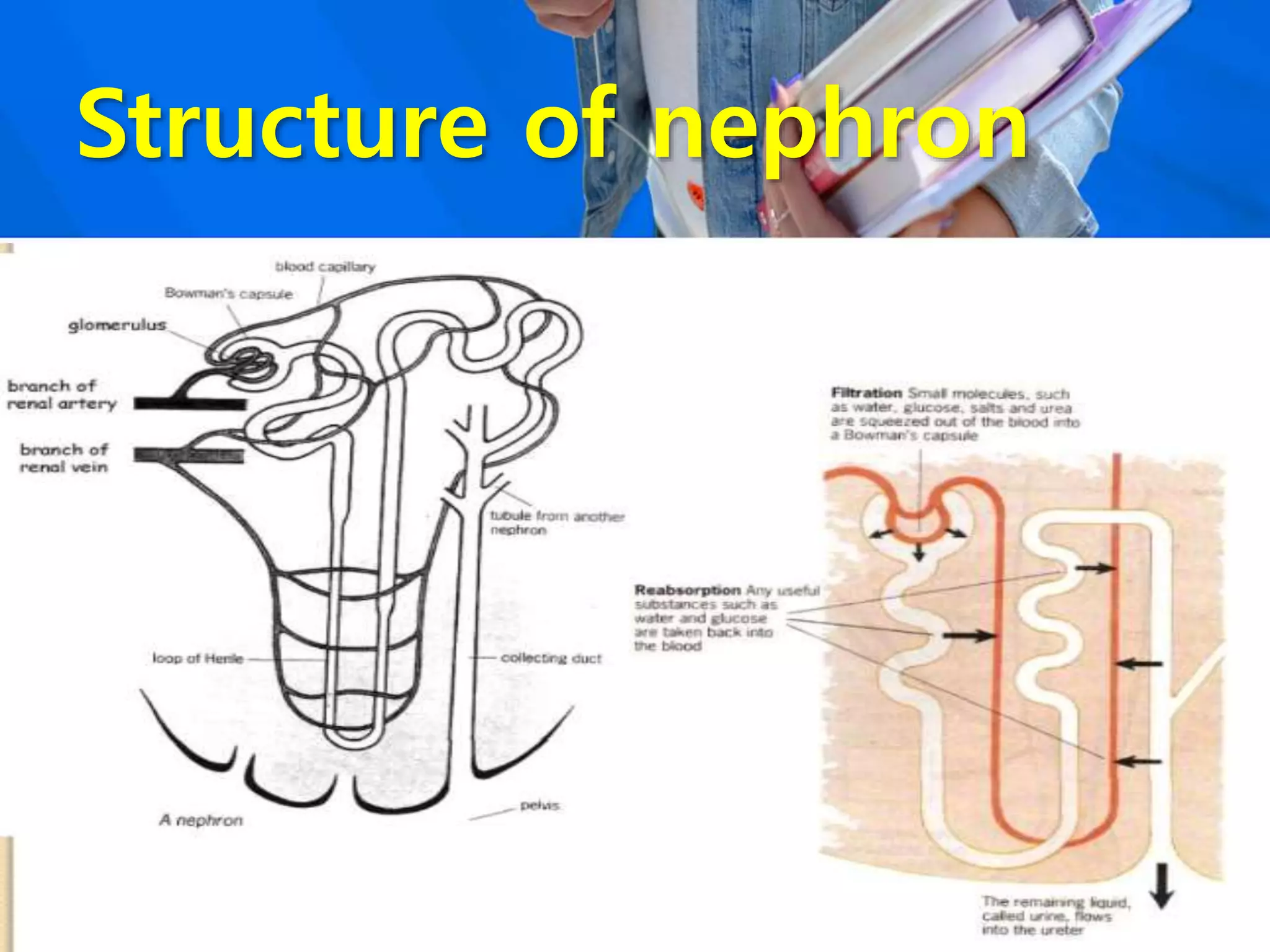
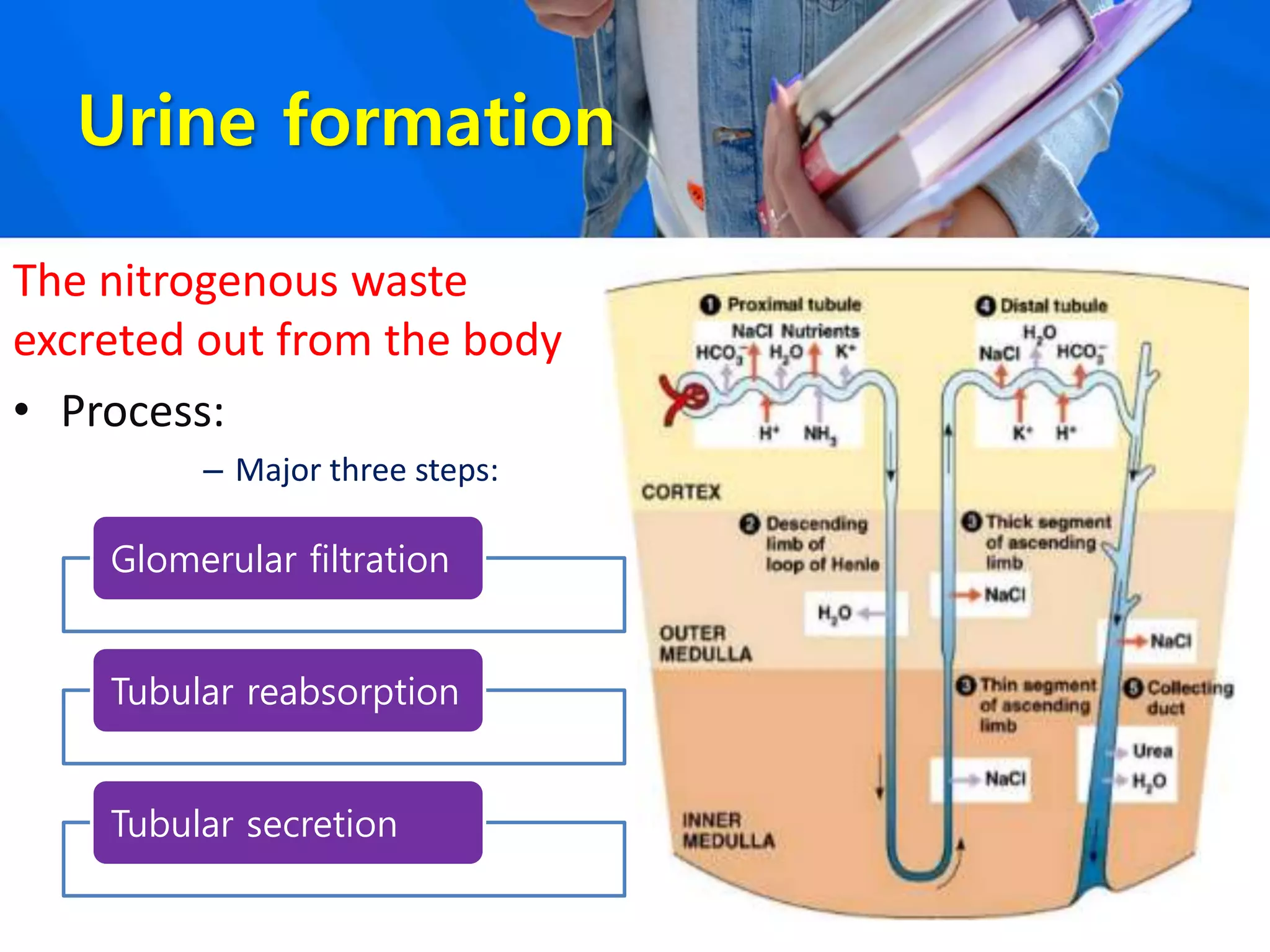
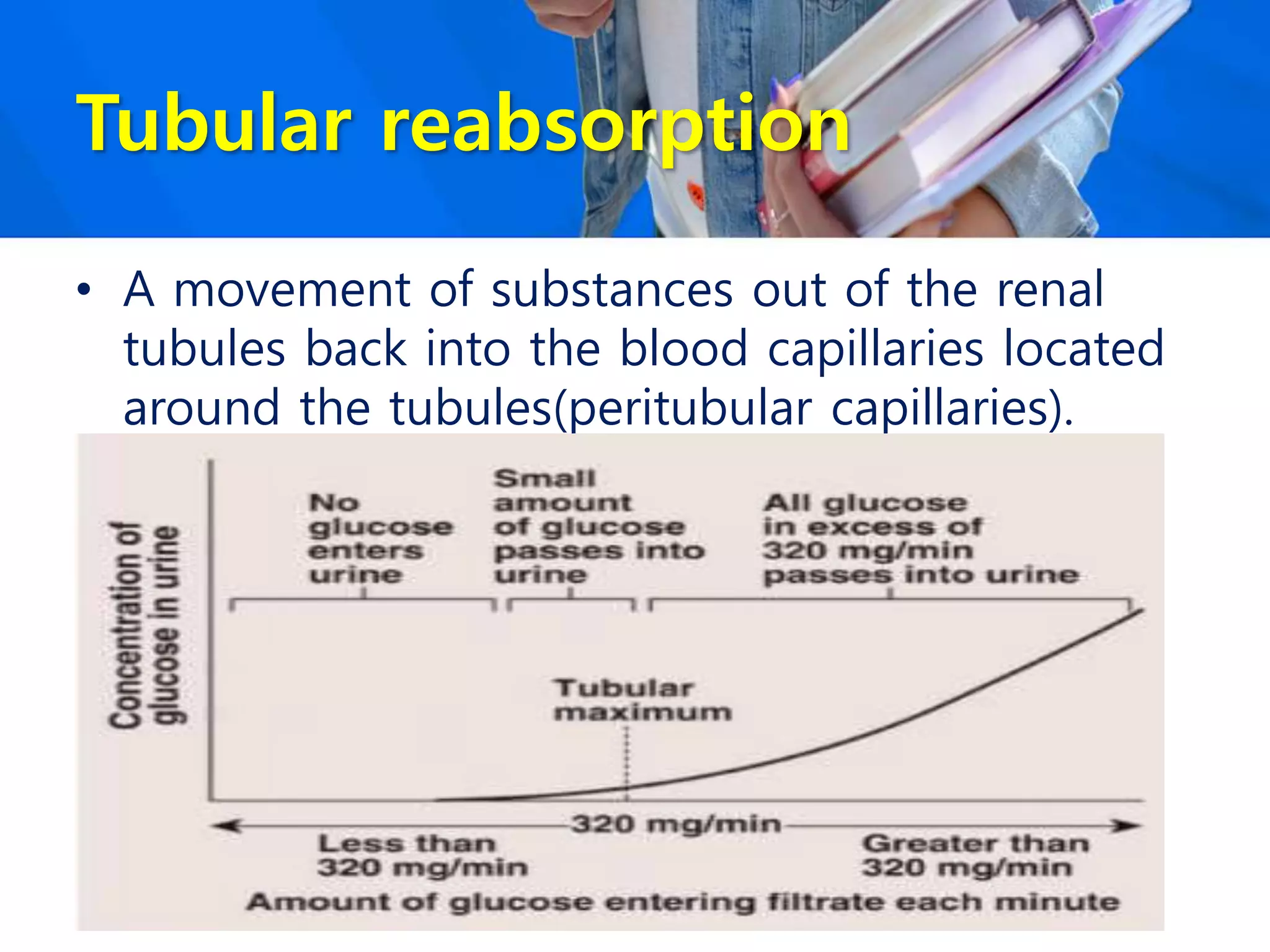
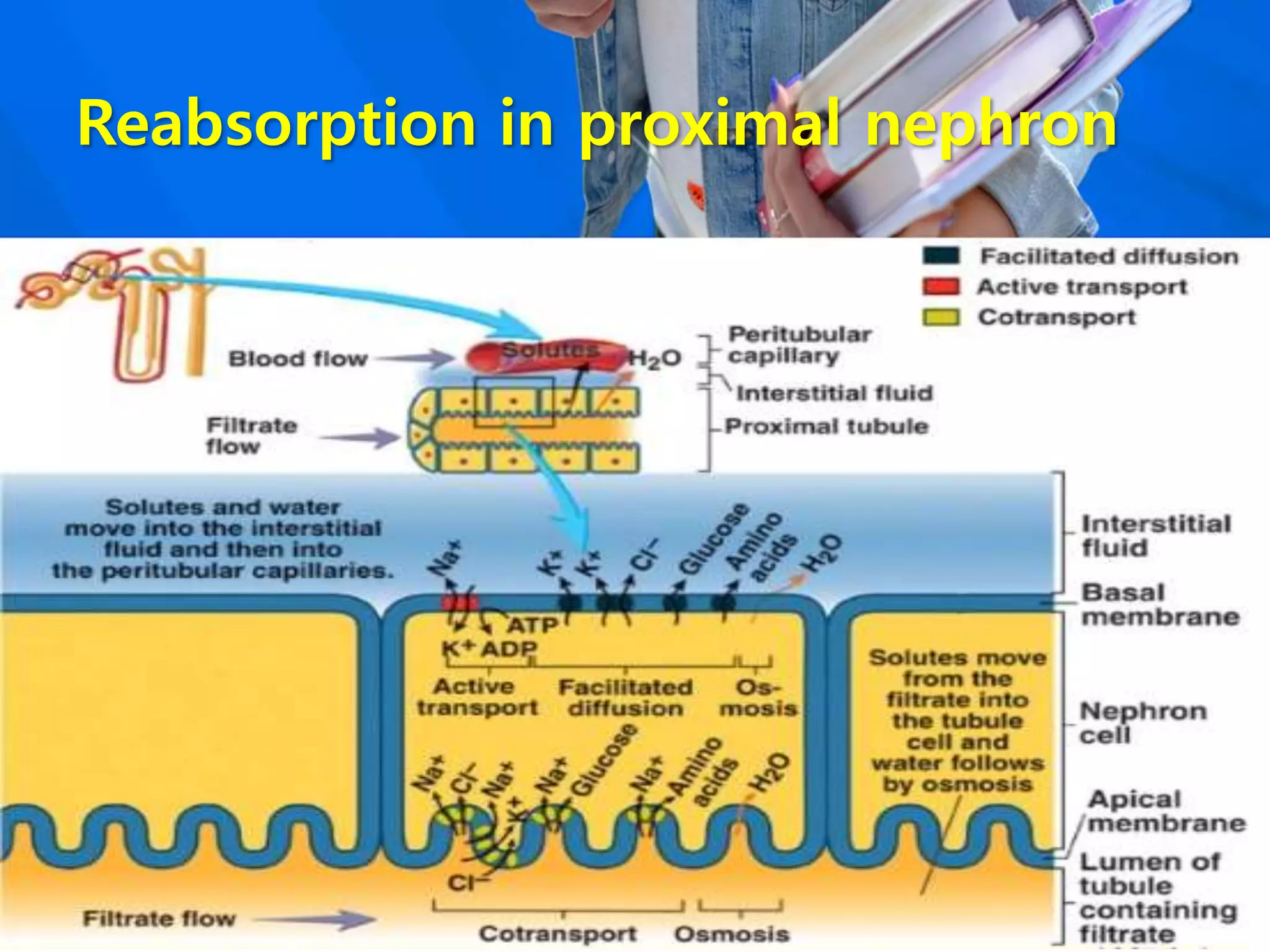
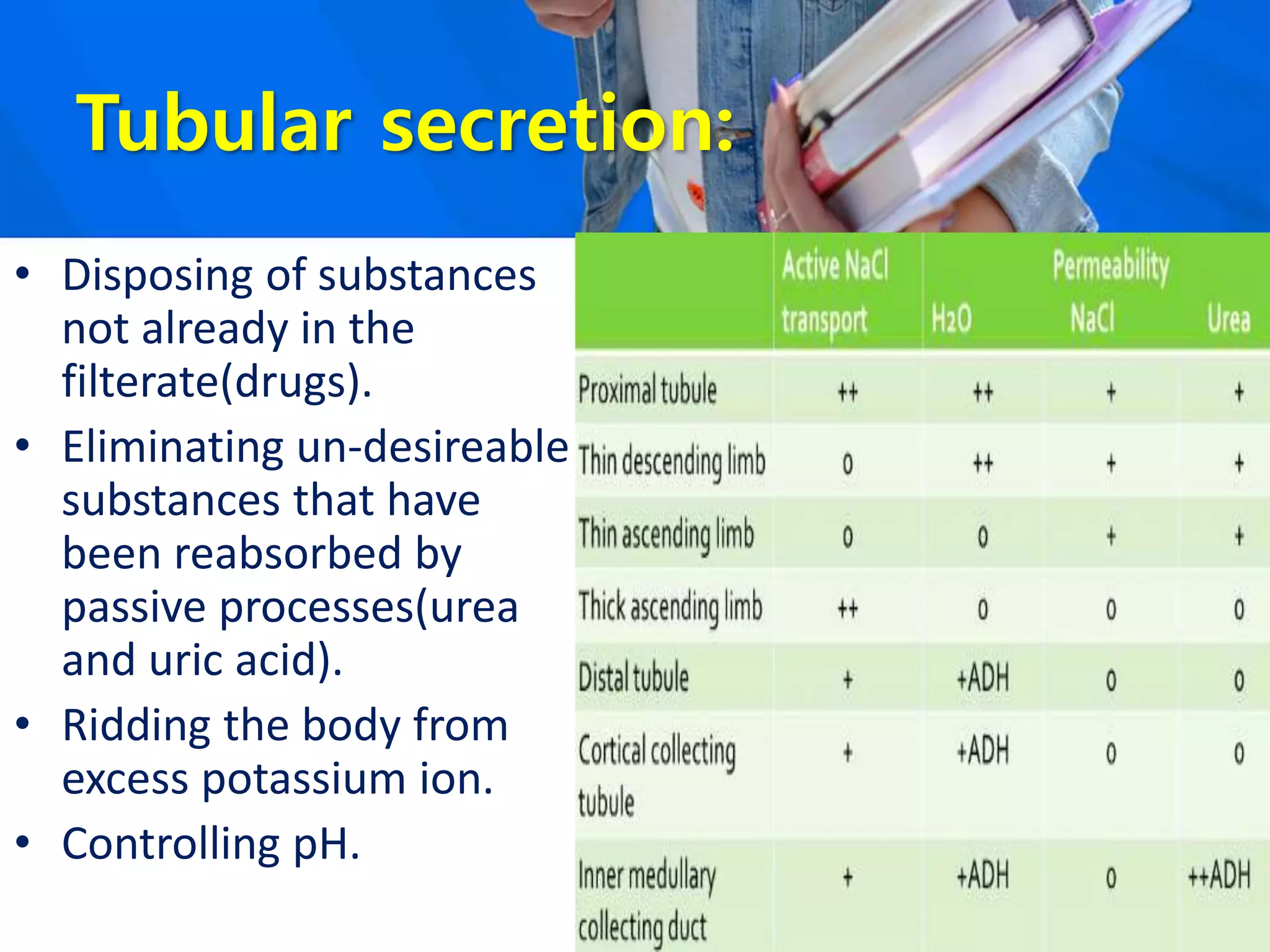
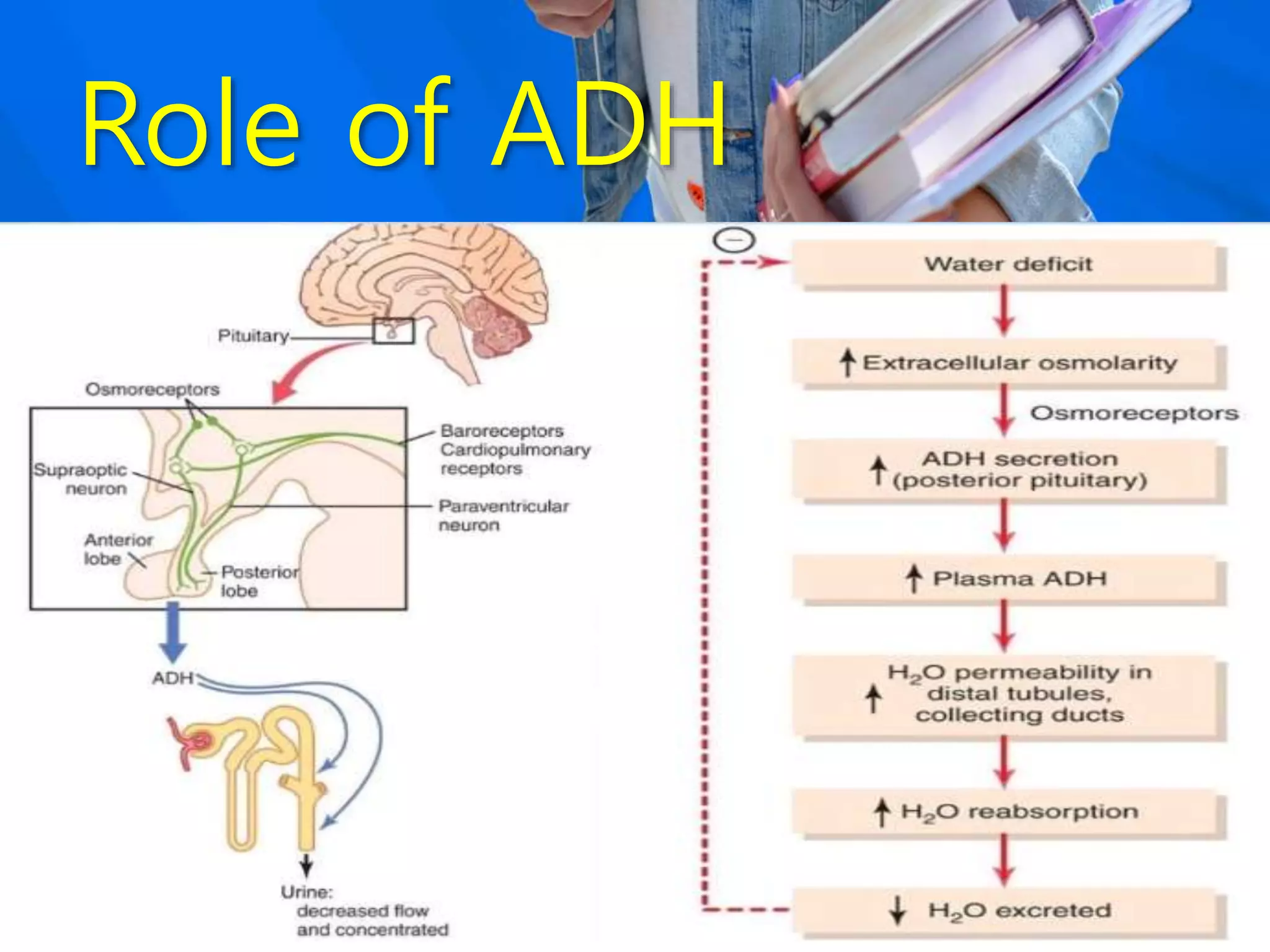
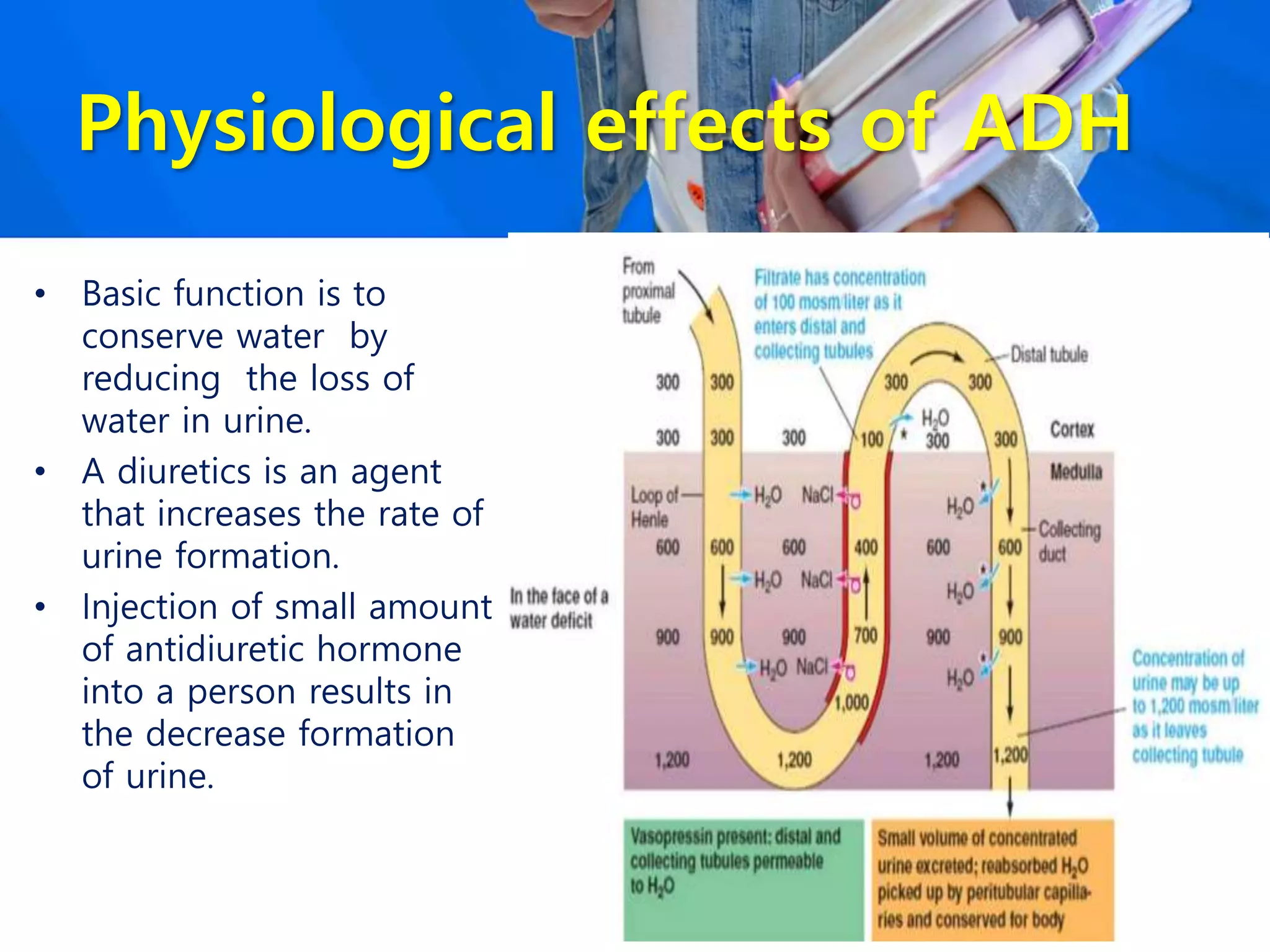
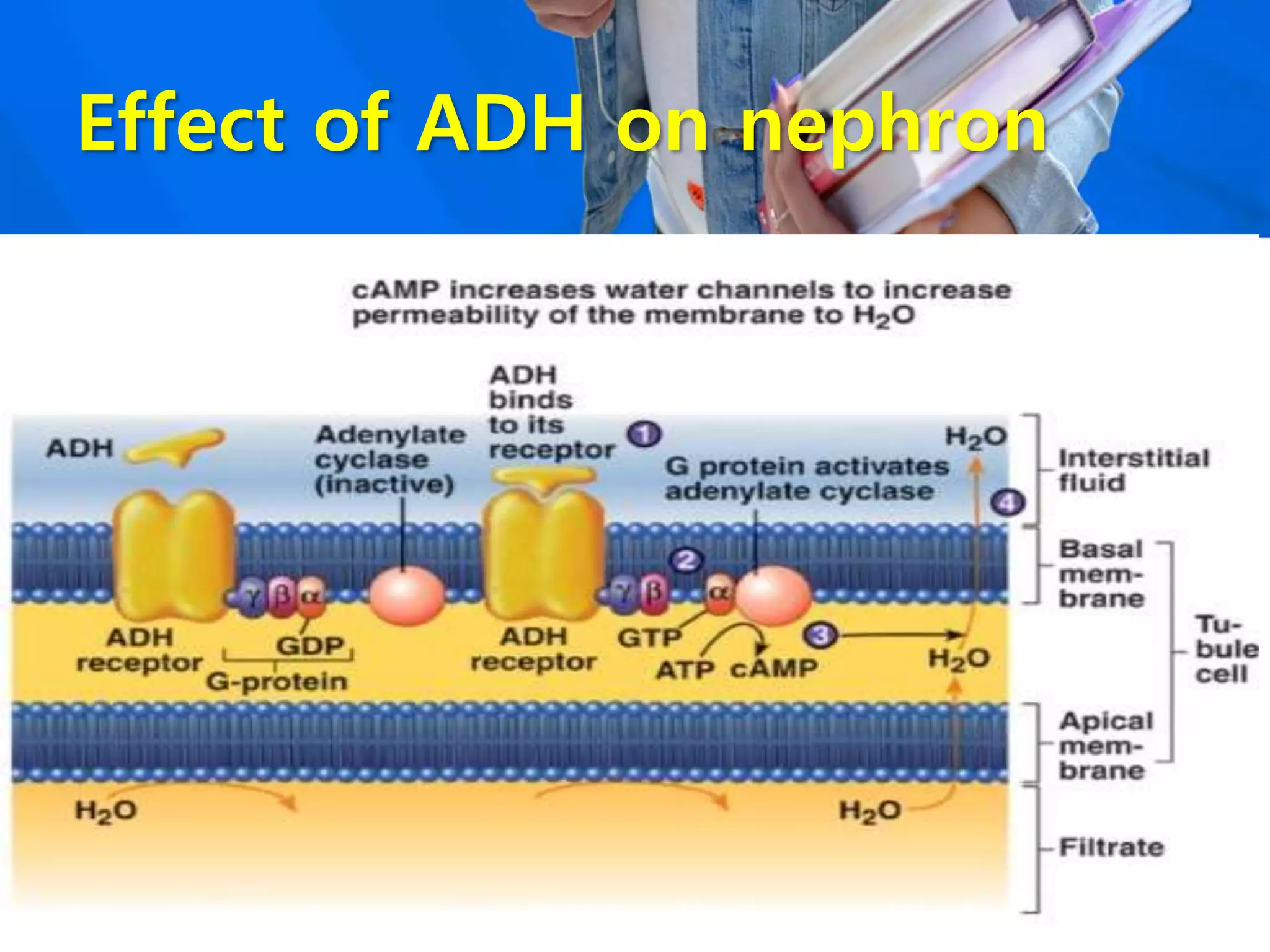
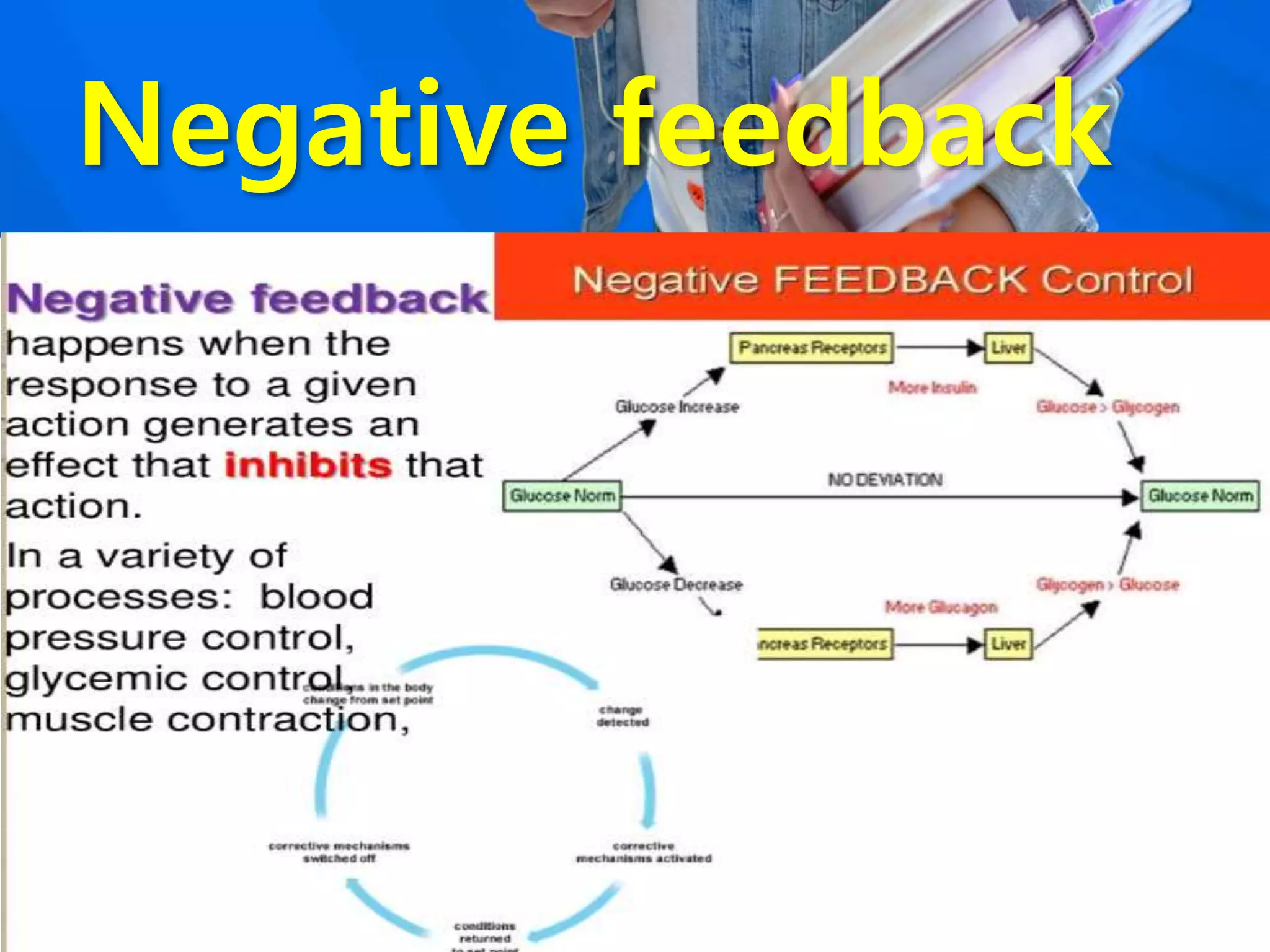
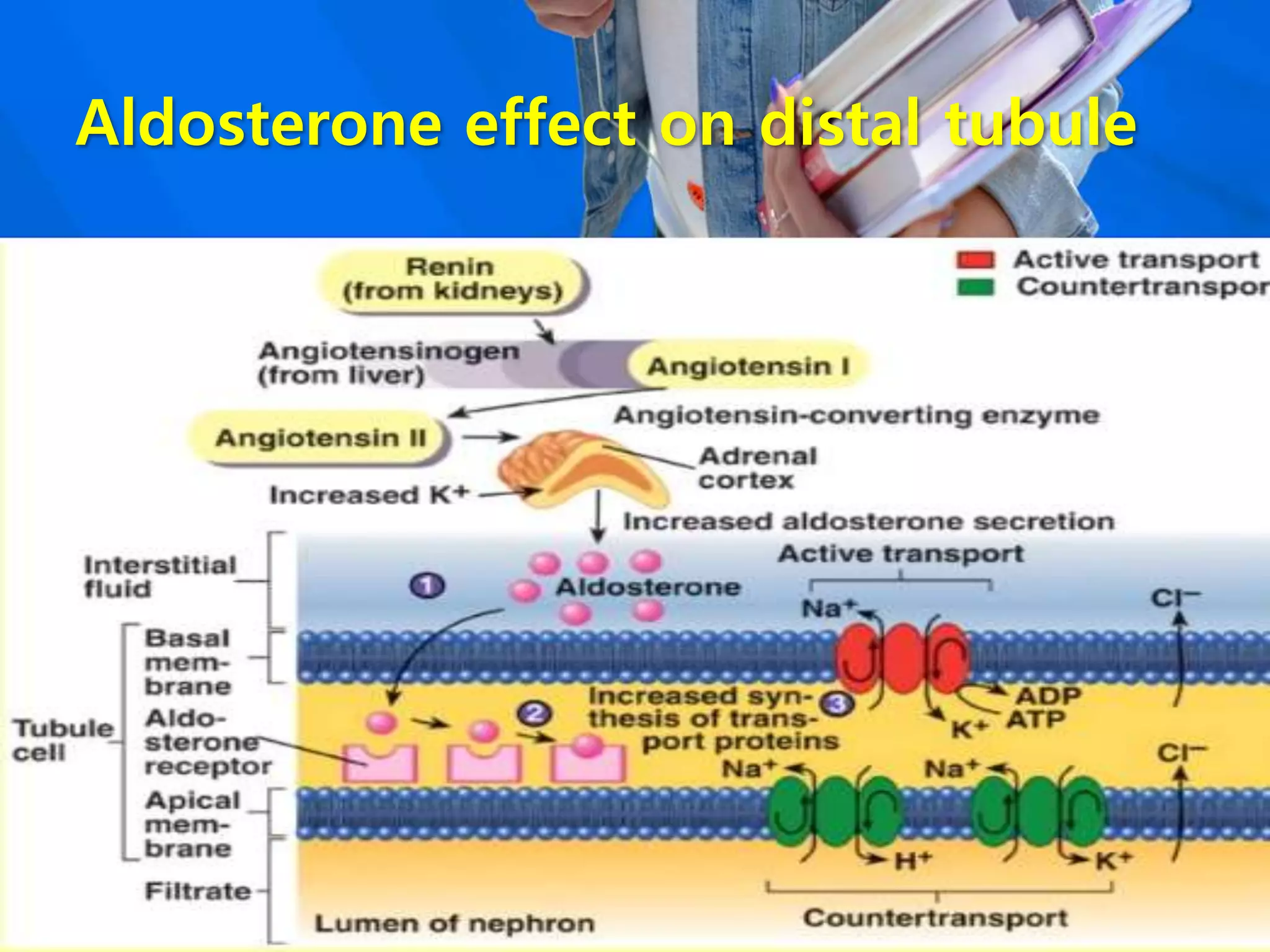
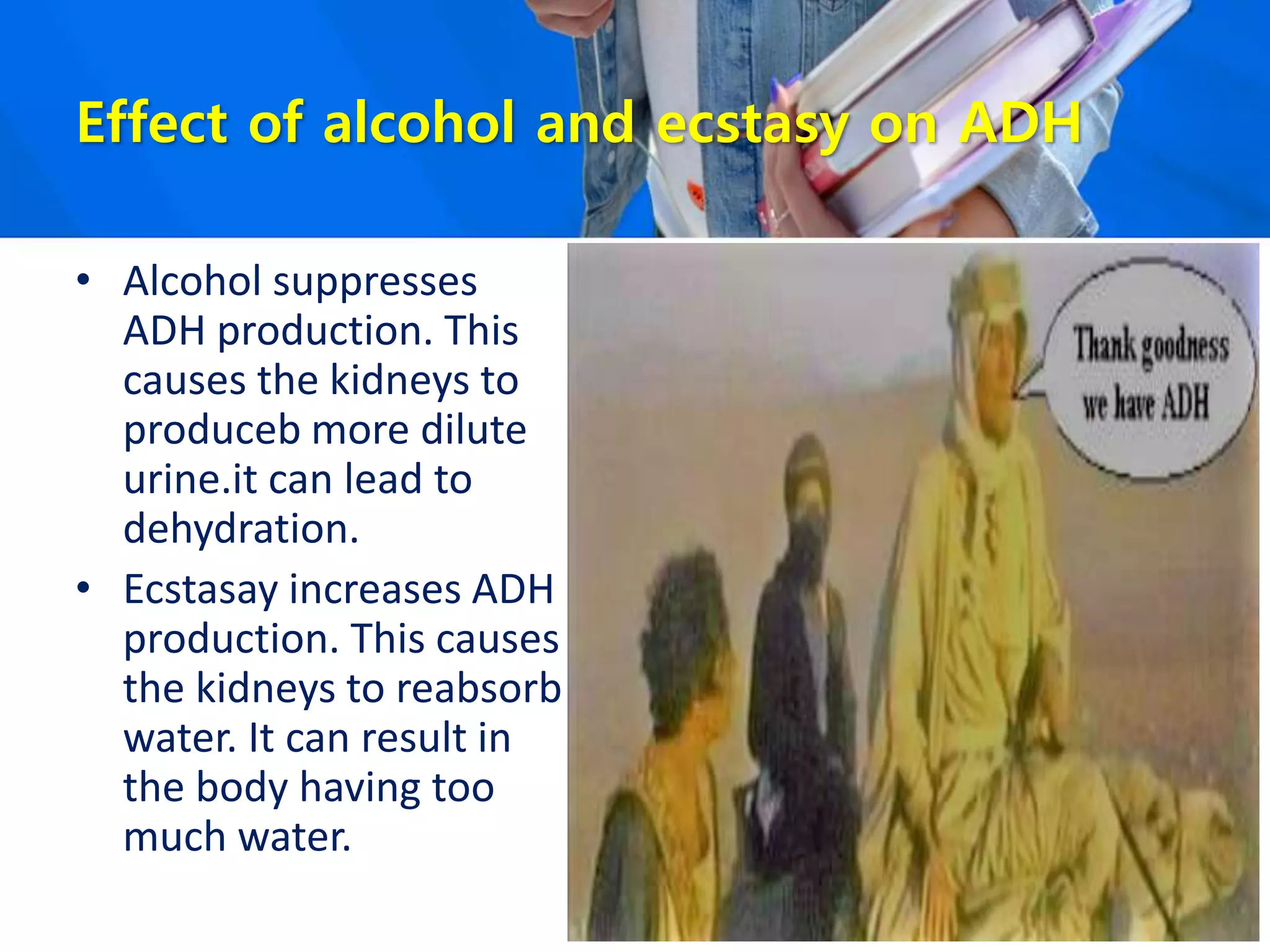
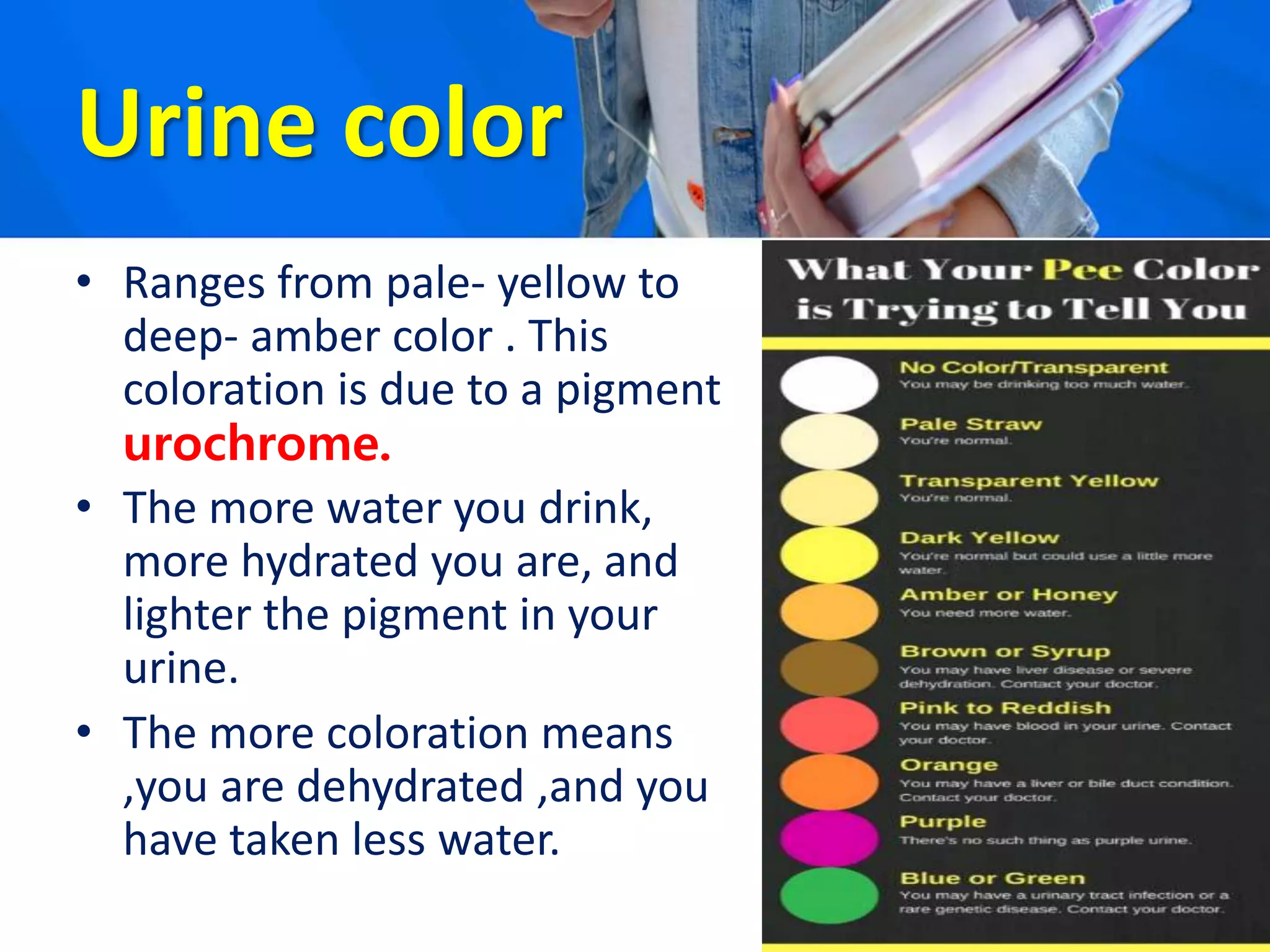
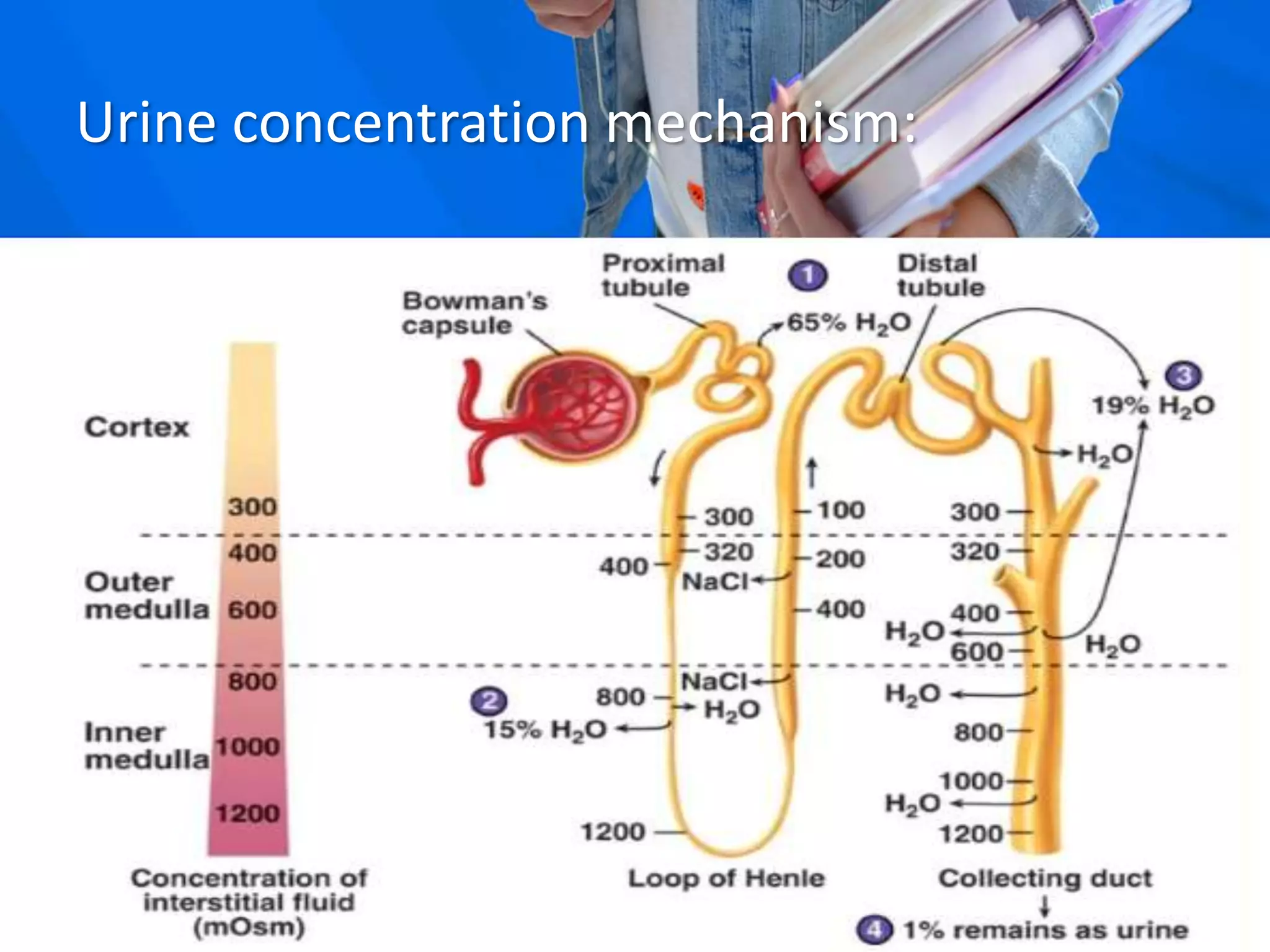
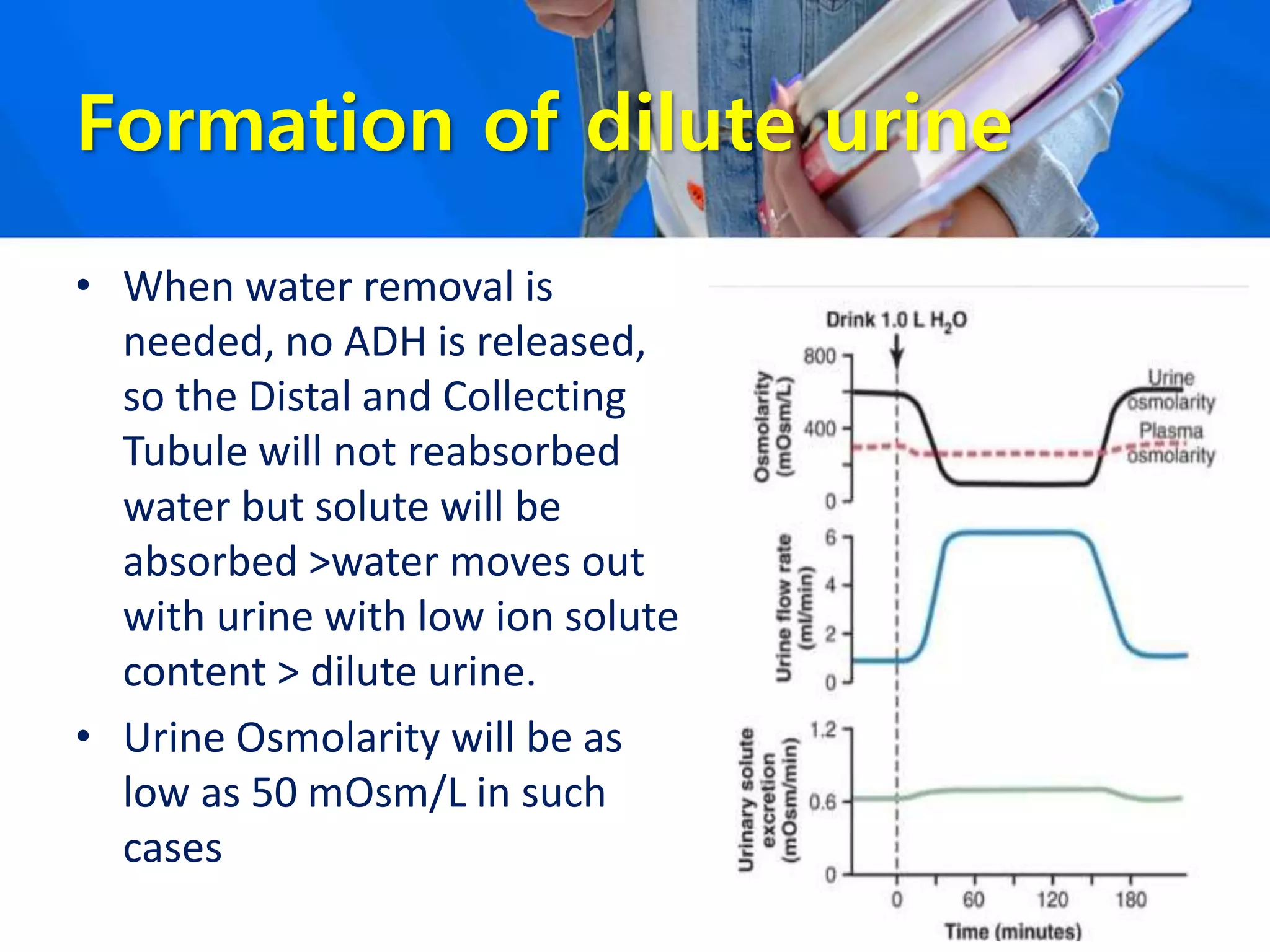
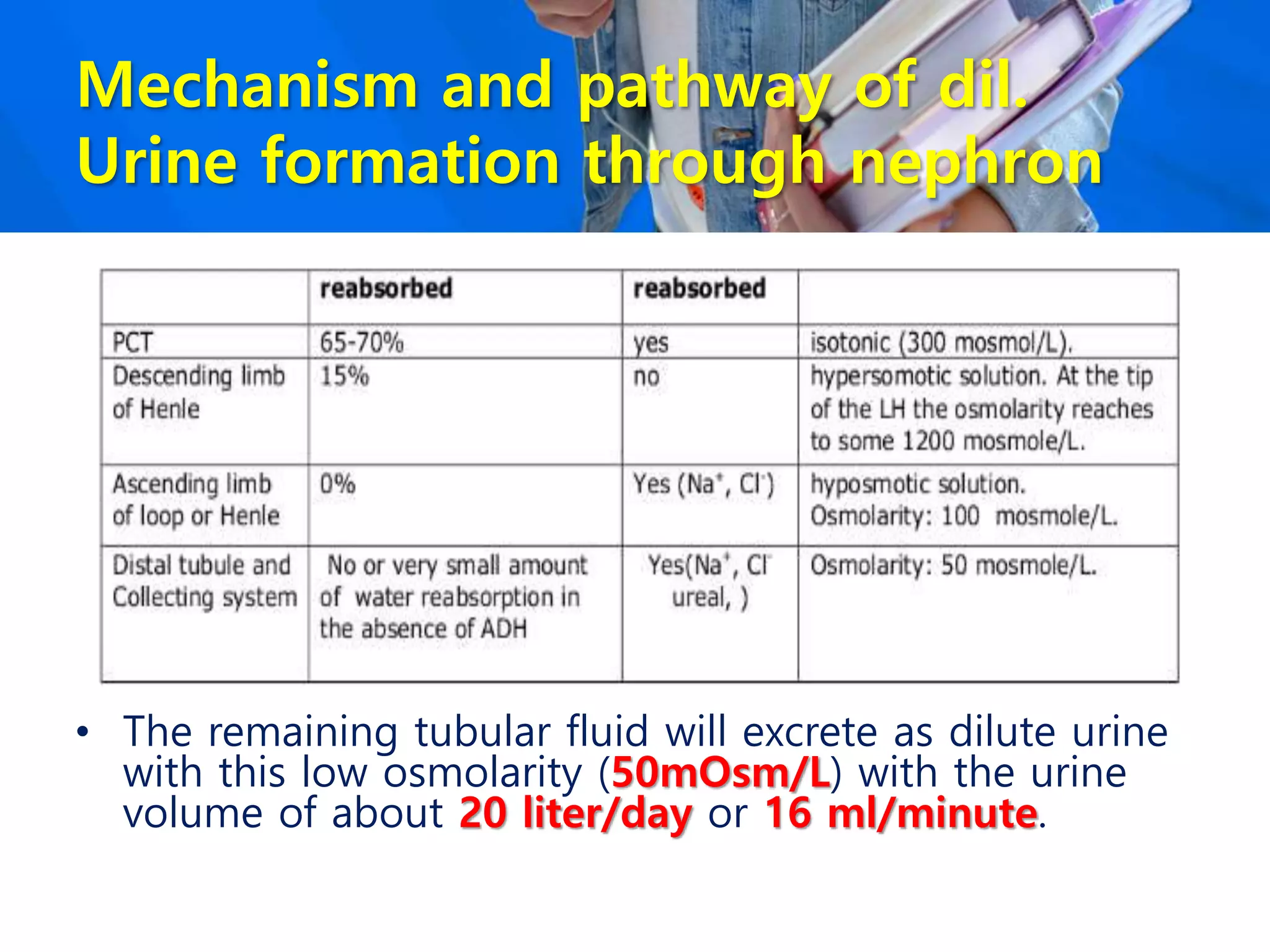
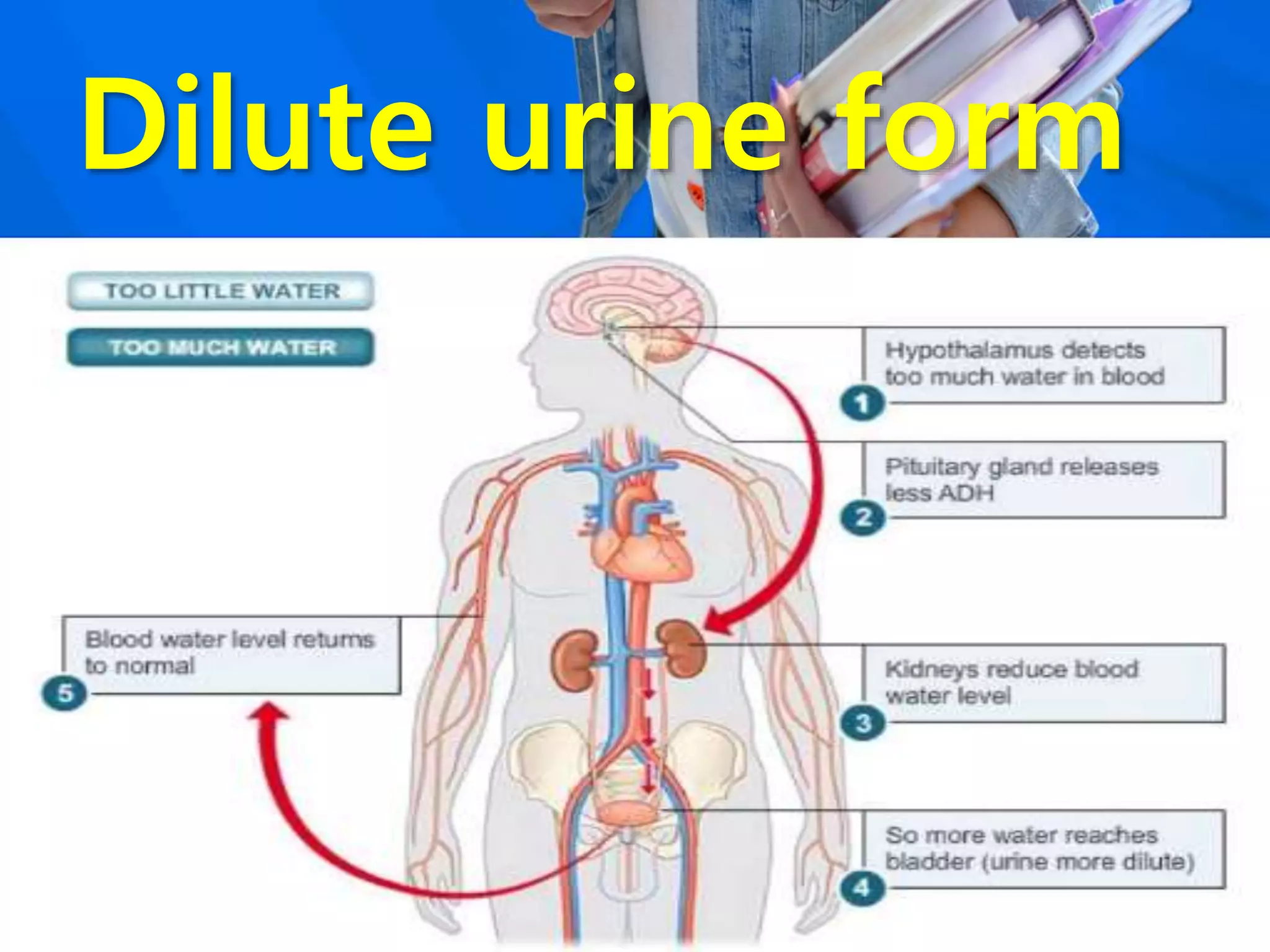
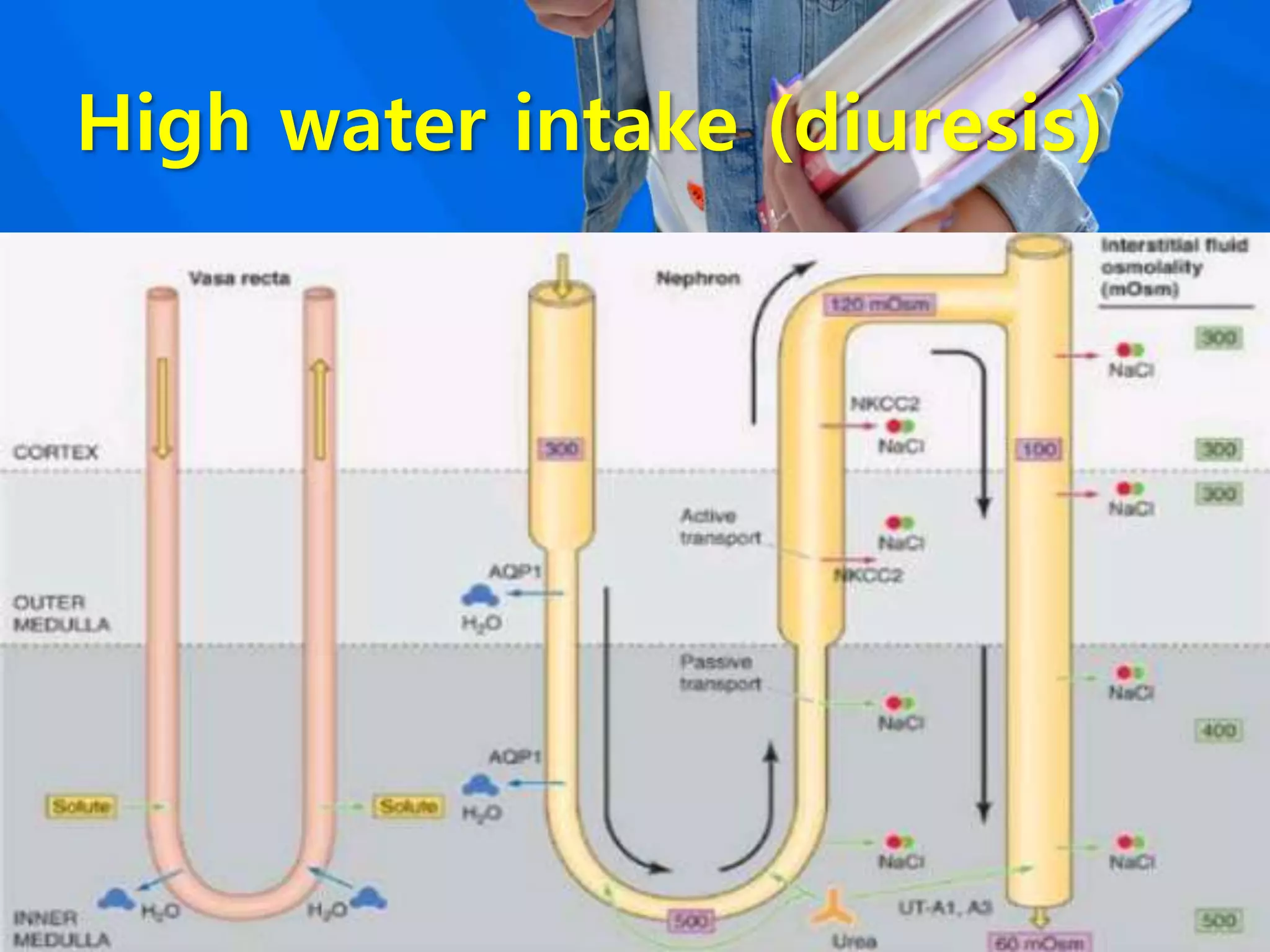
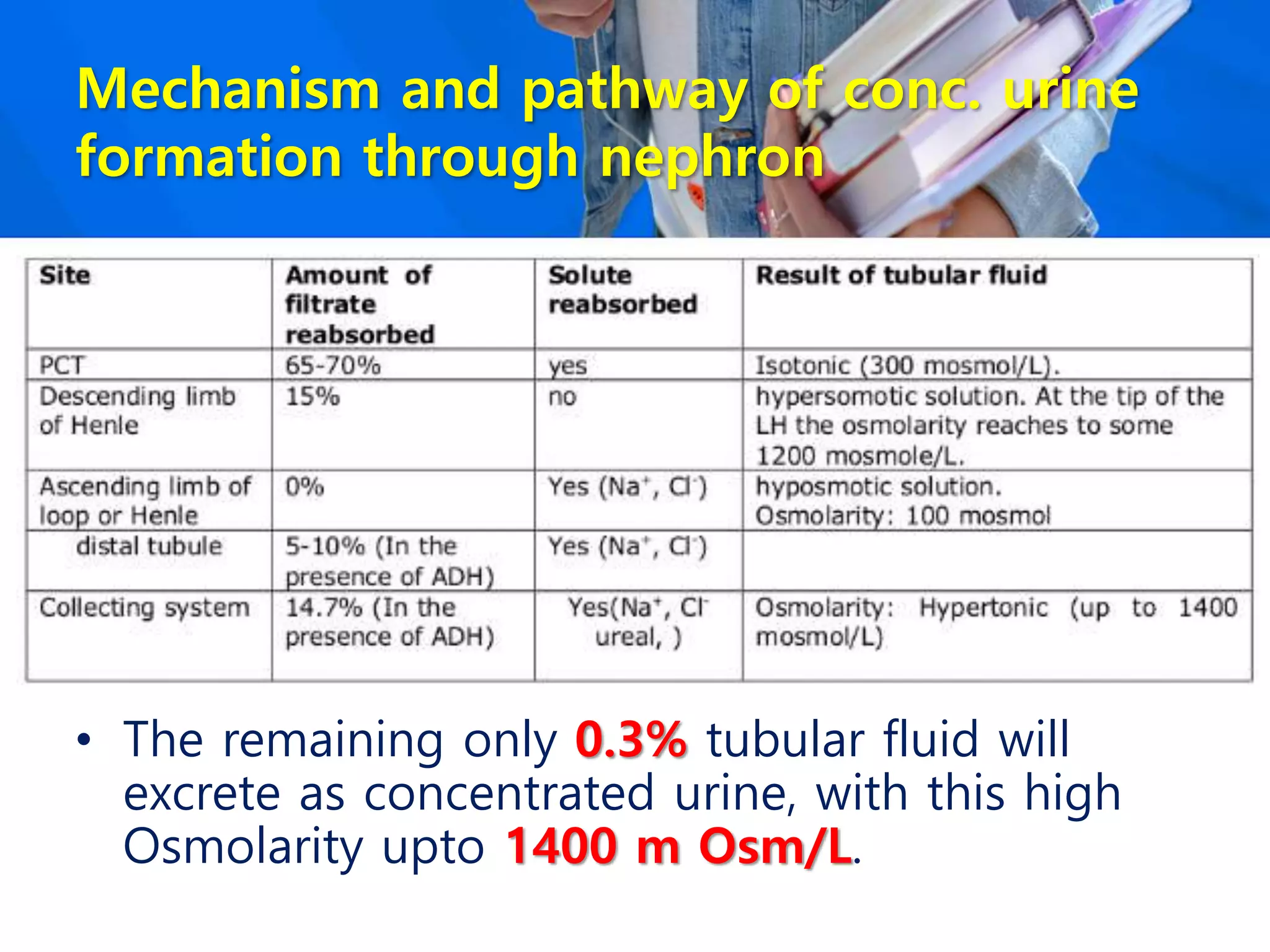
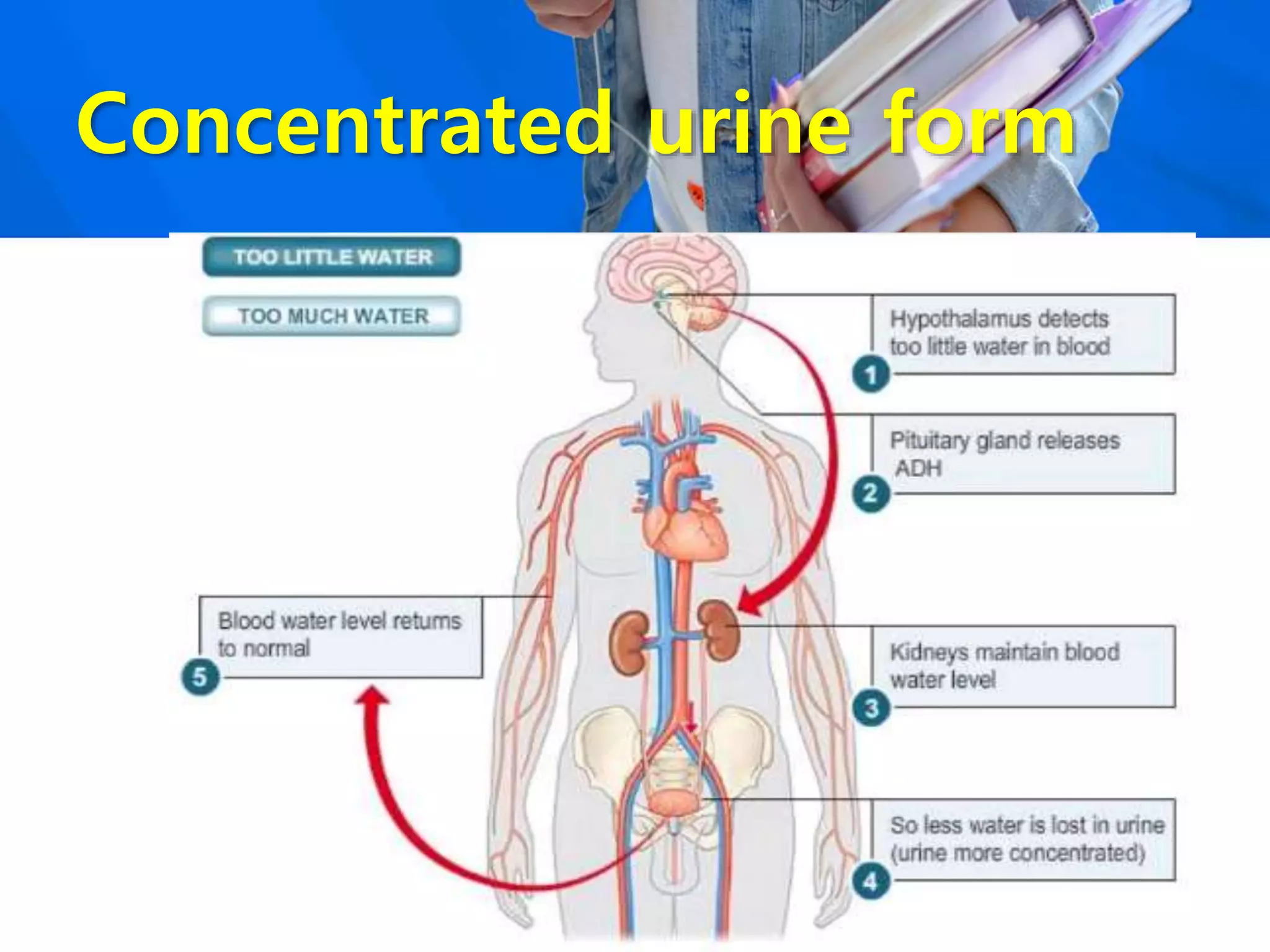
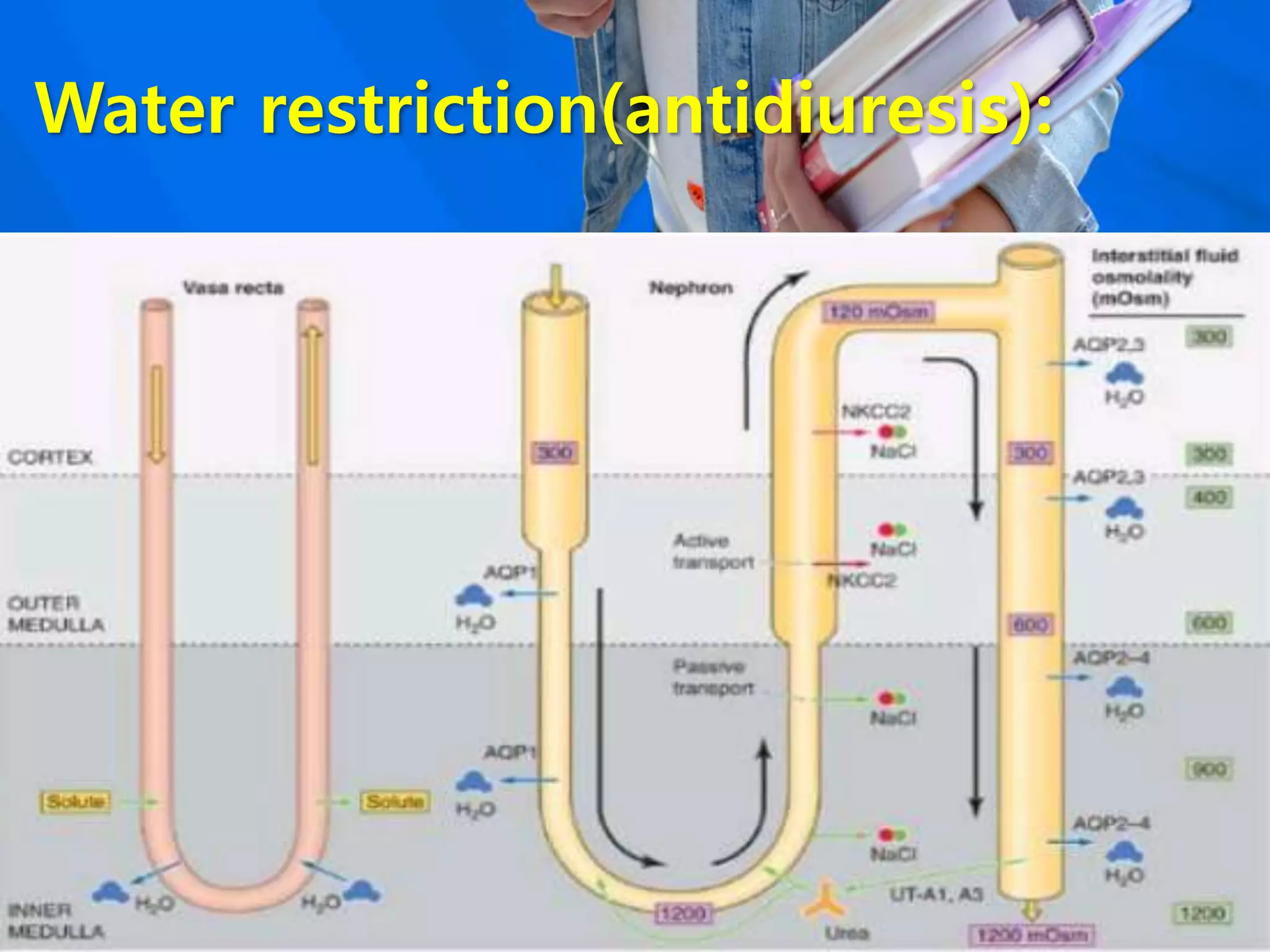
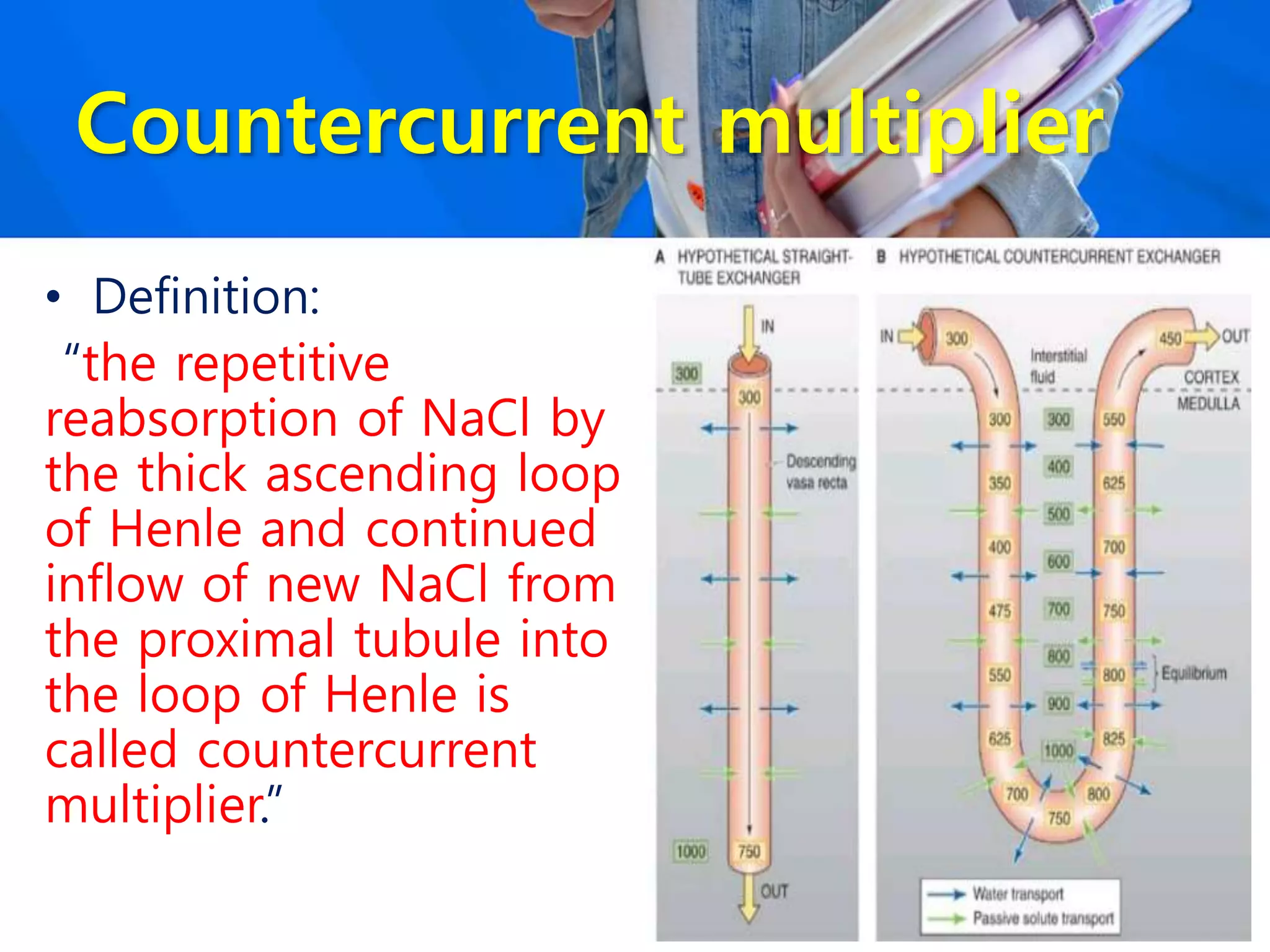
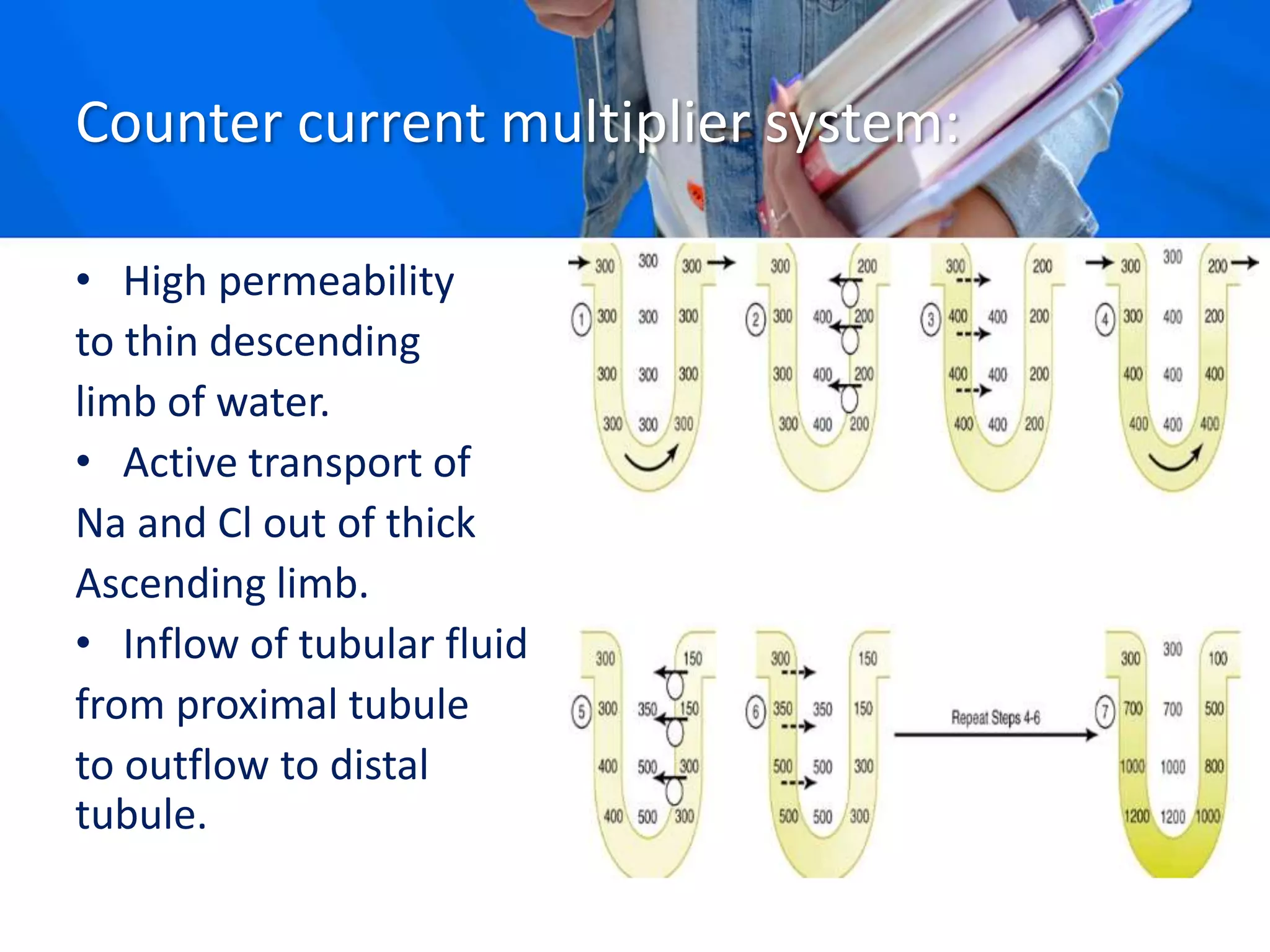
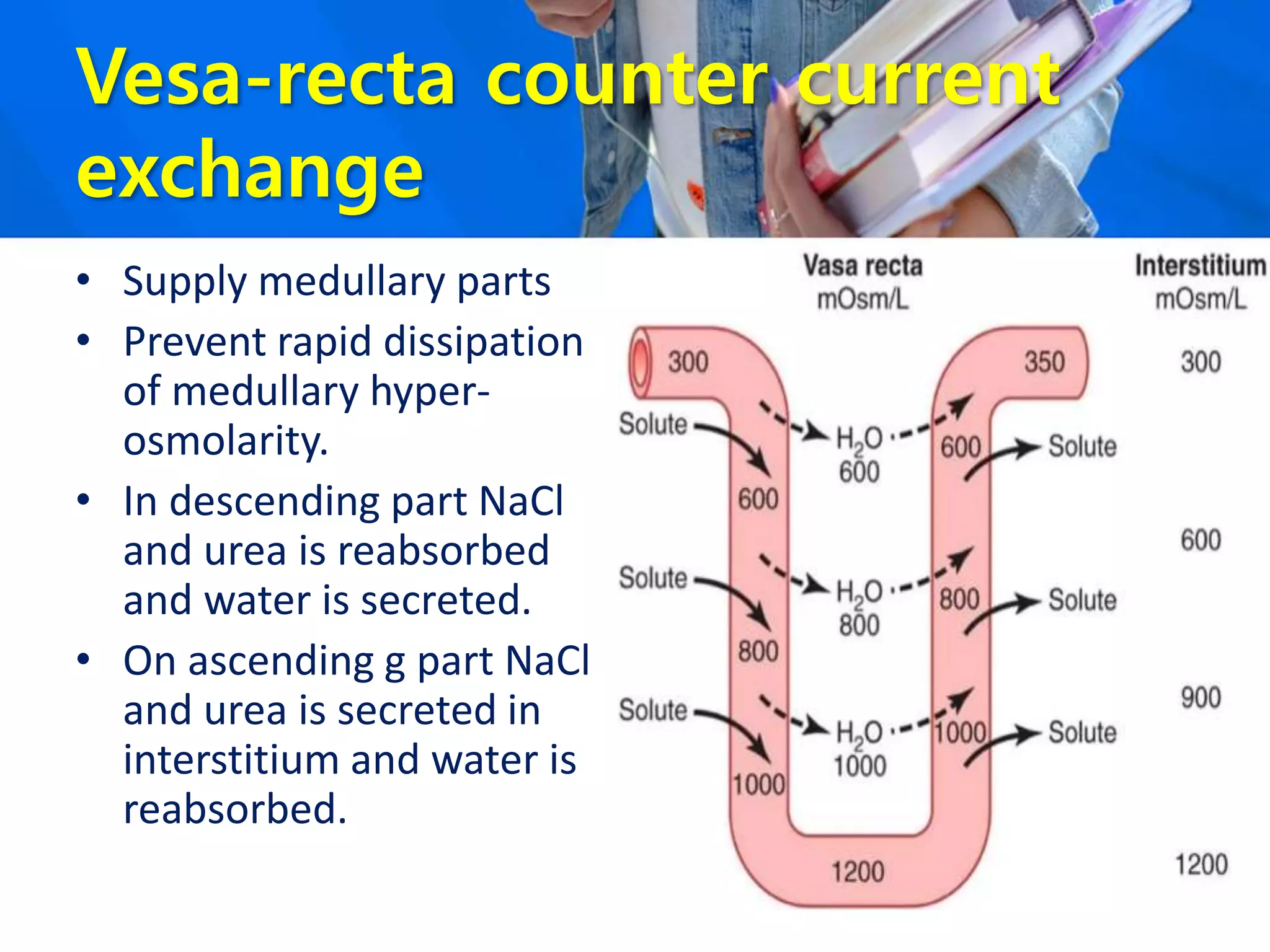
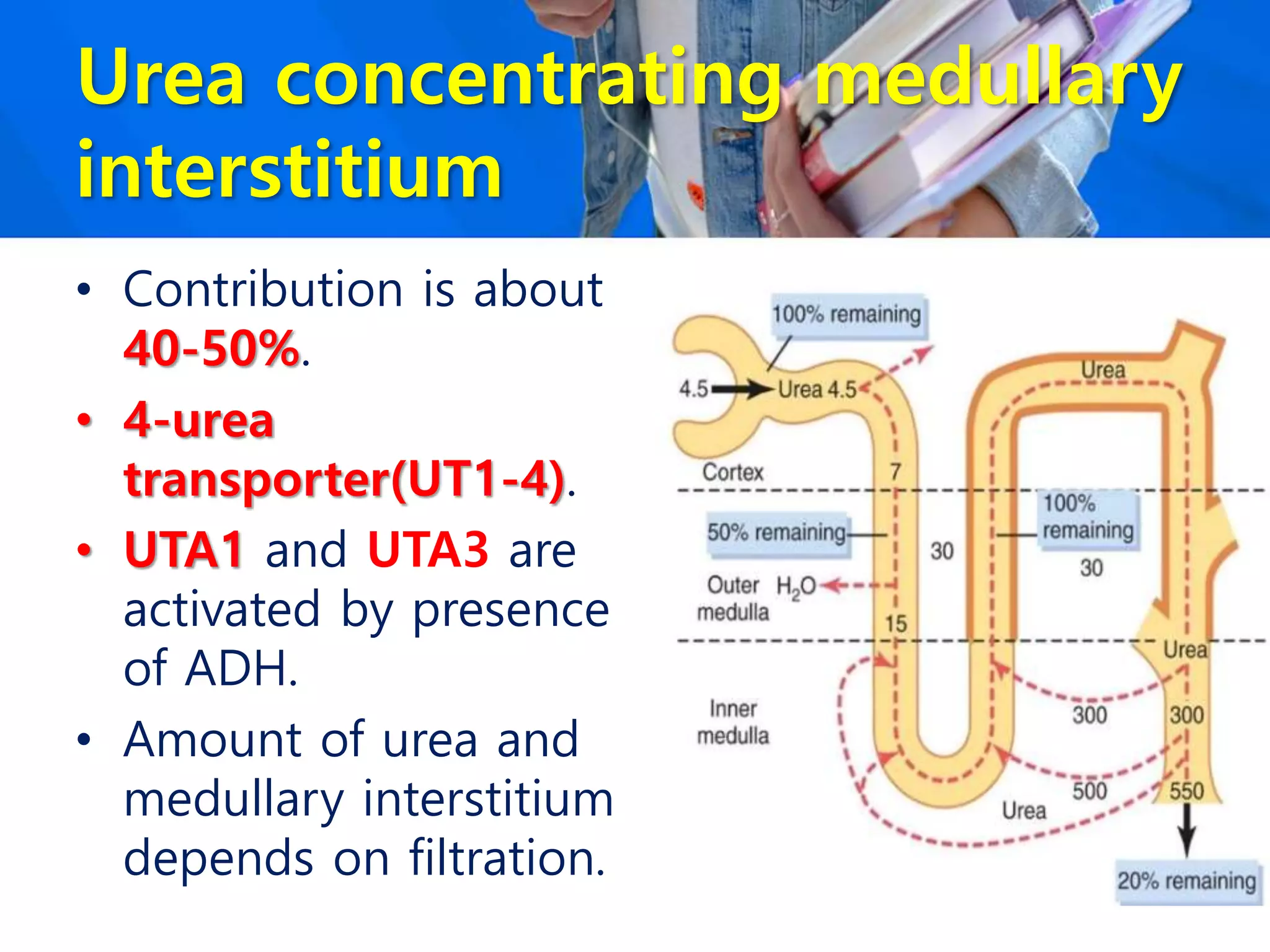
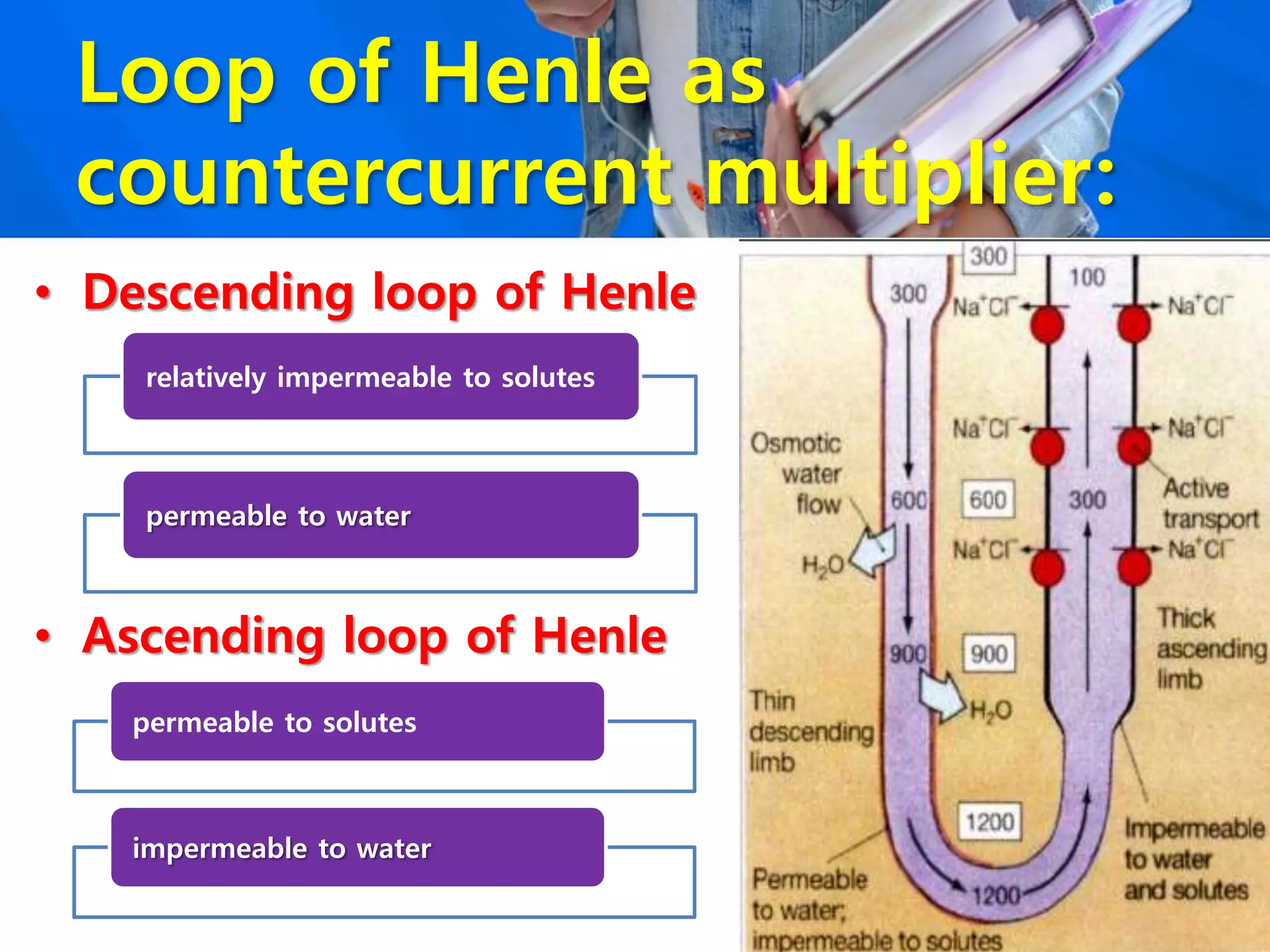
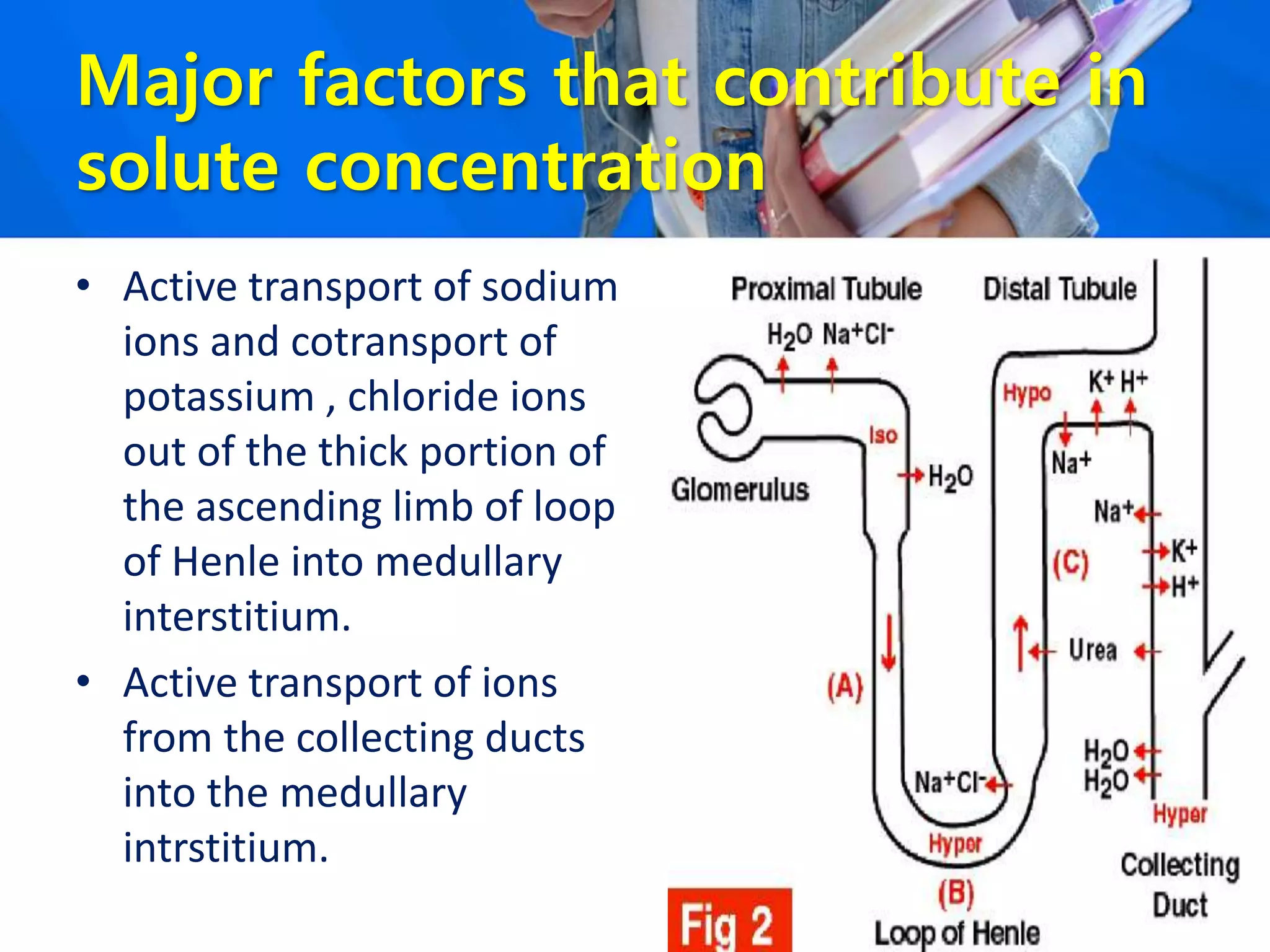
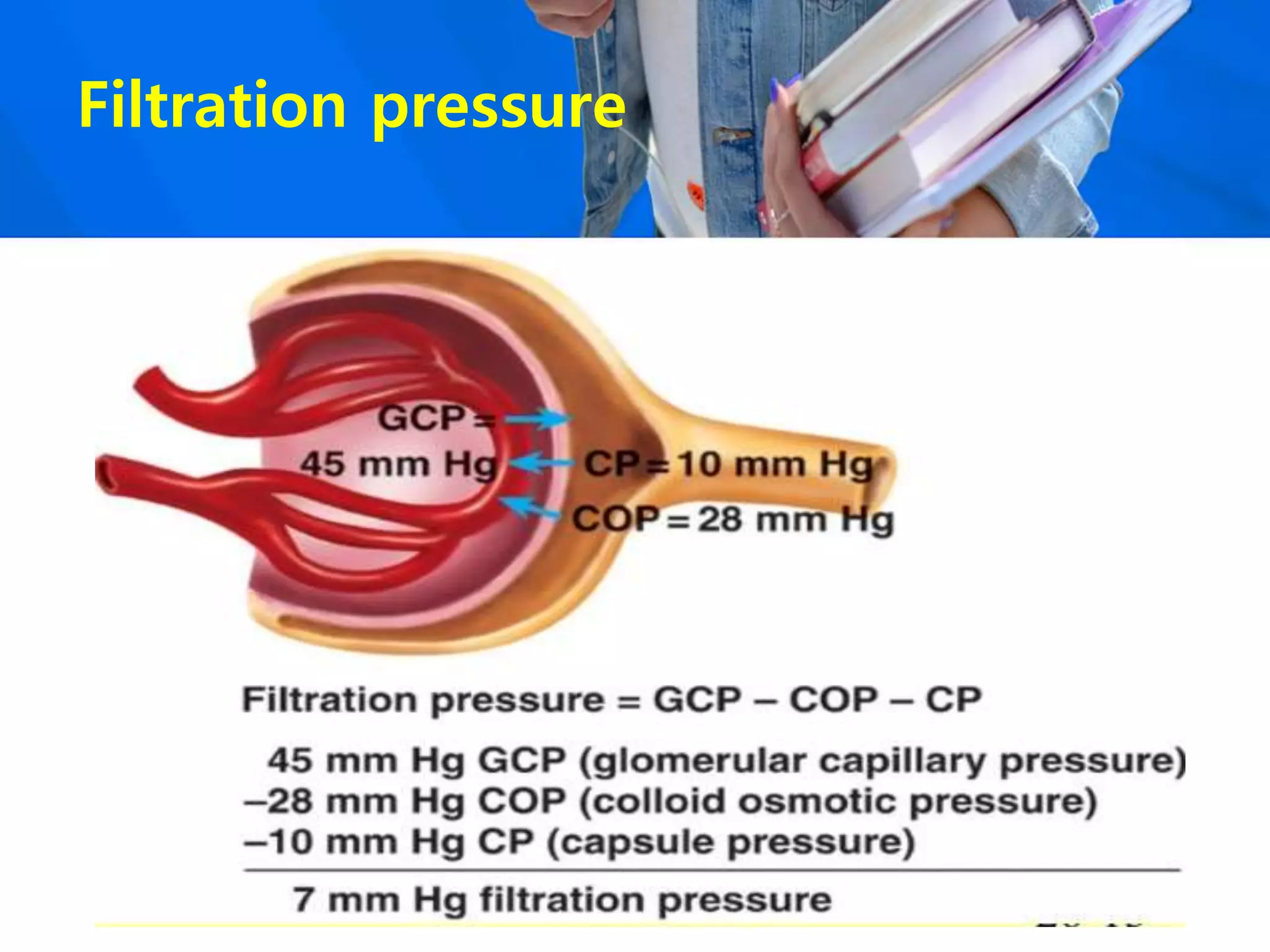
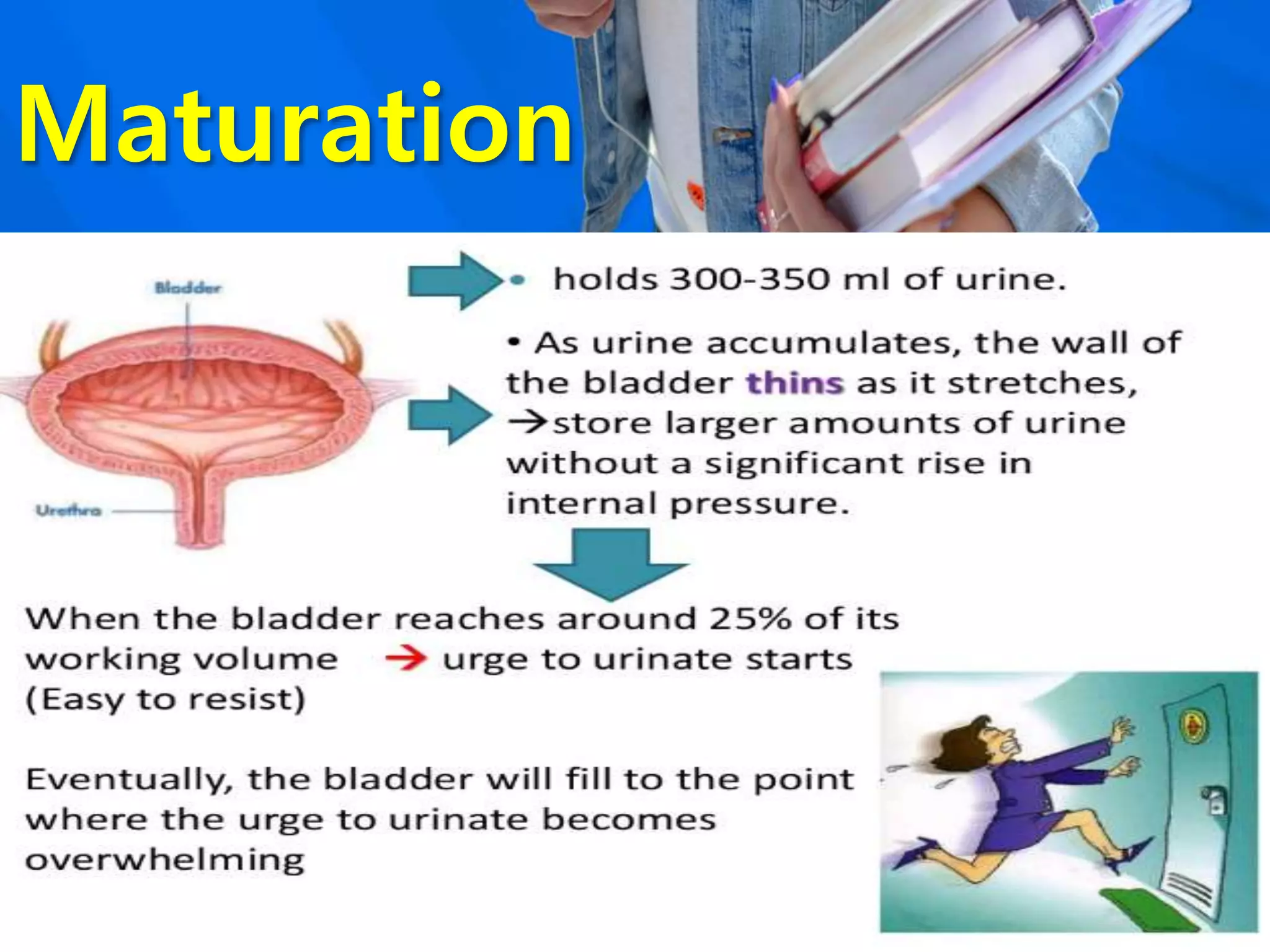
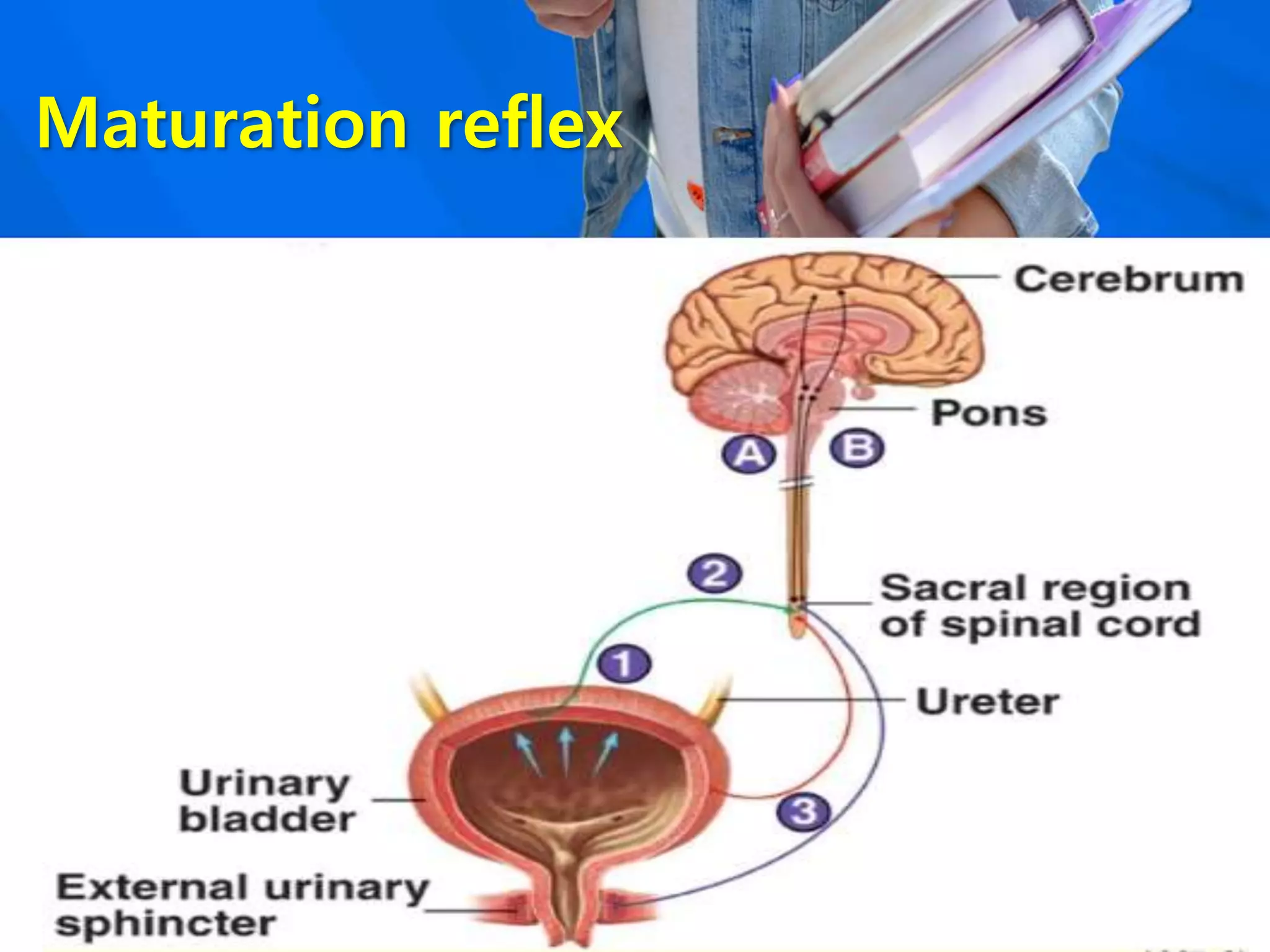
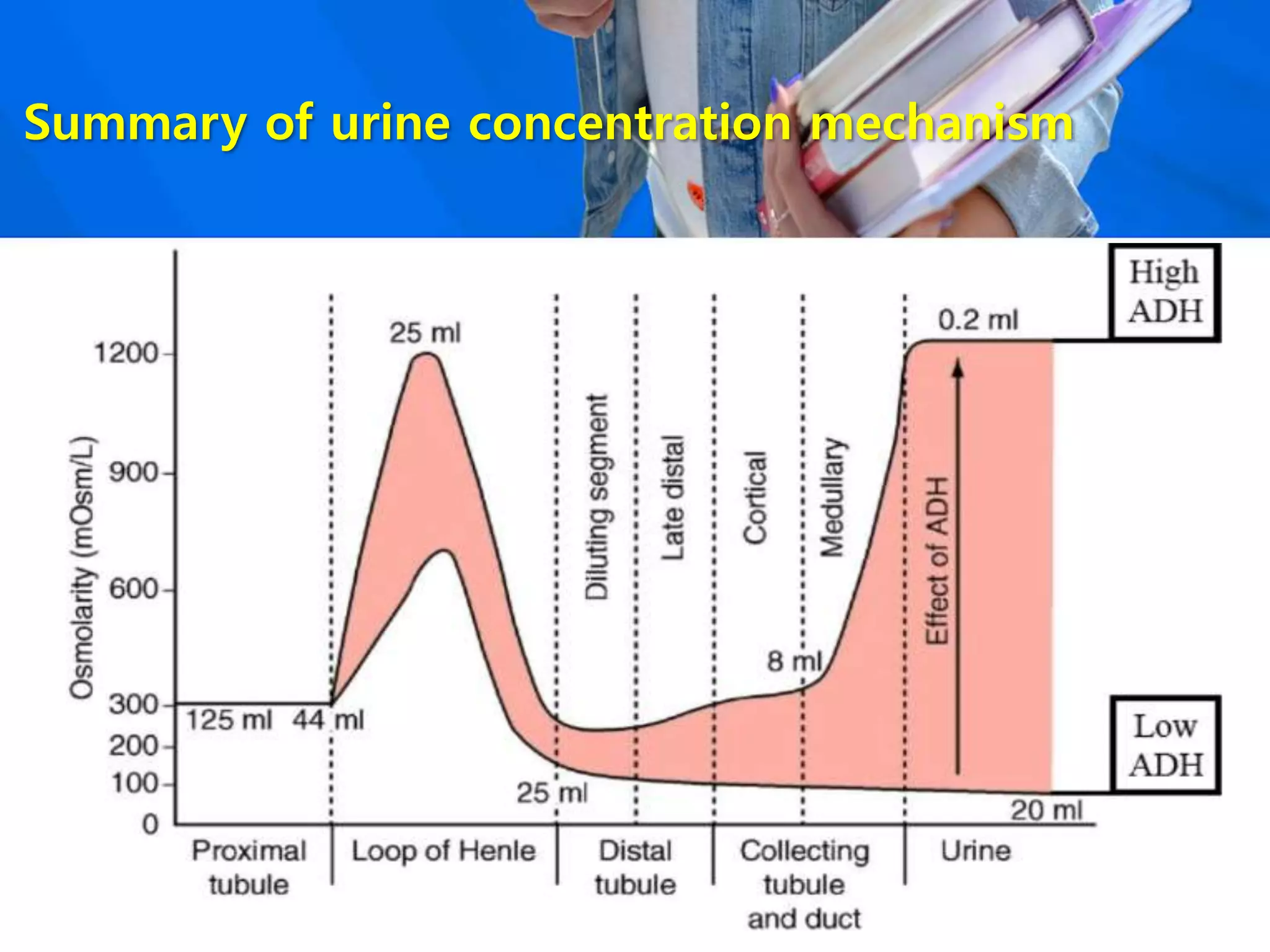
The document discusses urine concentration and the urinary system. It describes how the kidney regulates water and electrolyte balance through processes like glomerular filtration, tubular reabsorption, and tubular secretion in the nephron. Antidiuretic hormone (ADH) allows the kidney to concentrate urine by promoting water reabsorption in the collecting duct. A countercurrent mechanism in the loop of Henle also helps build up solute concentration. Disorders can occur if there are issues with ADH signaling or the countercurrent system that prevent proper urine concentration.