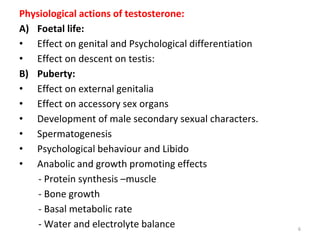
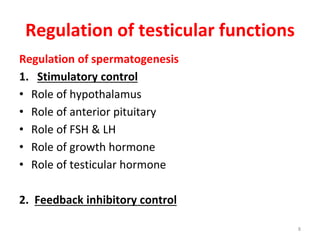
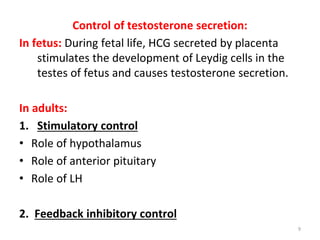
Testosterone is produced in the testes and is responsible for male sexual development and function. It regulates spermatogenesis, muscle growth, bone growth, and other physiological processes. Levels are controlled by the hypothalamus and pituitary gland through LH secretion. Semen analysis evaluates semen volume, pH, viscosity, and the presence of secretions from testes, seminal vesicles, prostate, and bulbourethral glands. Cryptorchidism is the failure of one or both testes to descend into the scrotum, which can impair fertility if not surgically corrected. Castration before puberty prevents sexual maturation and function, while after puberty secondary sex characteristics remain but sexual desire and function