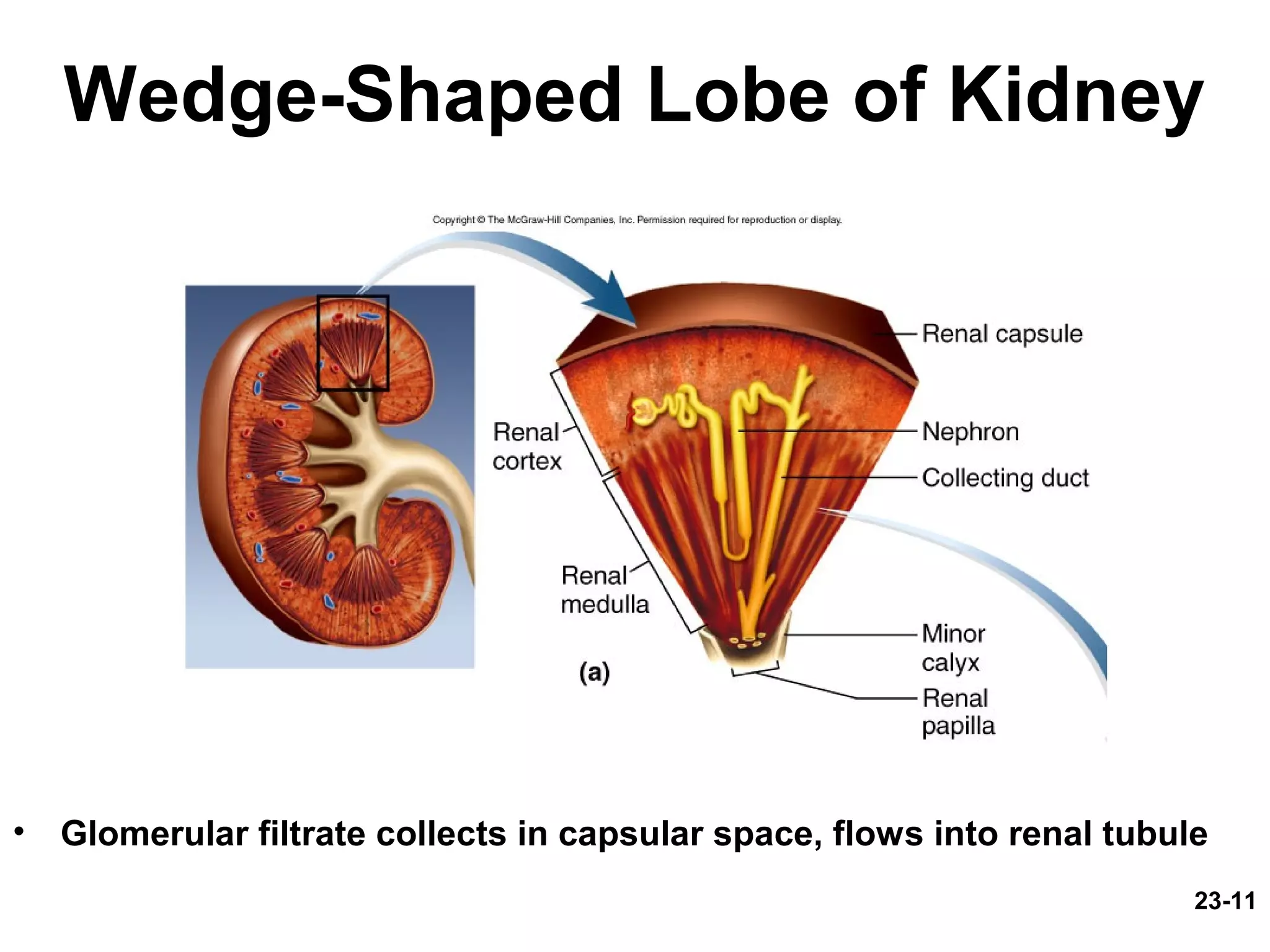
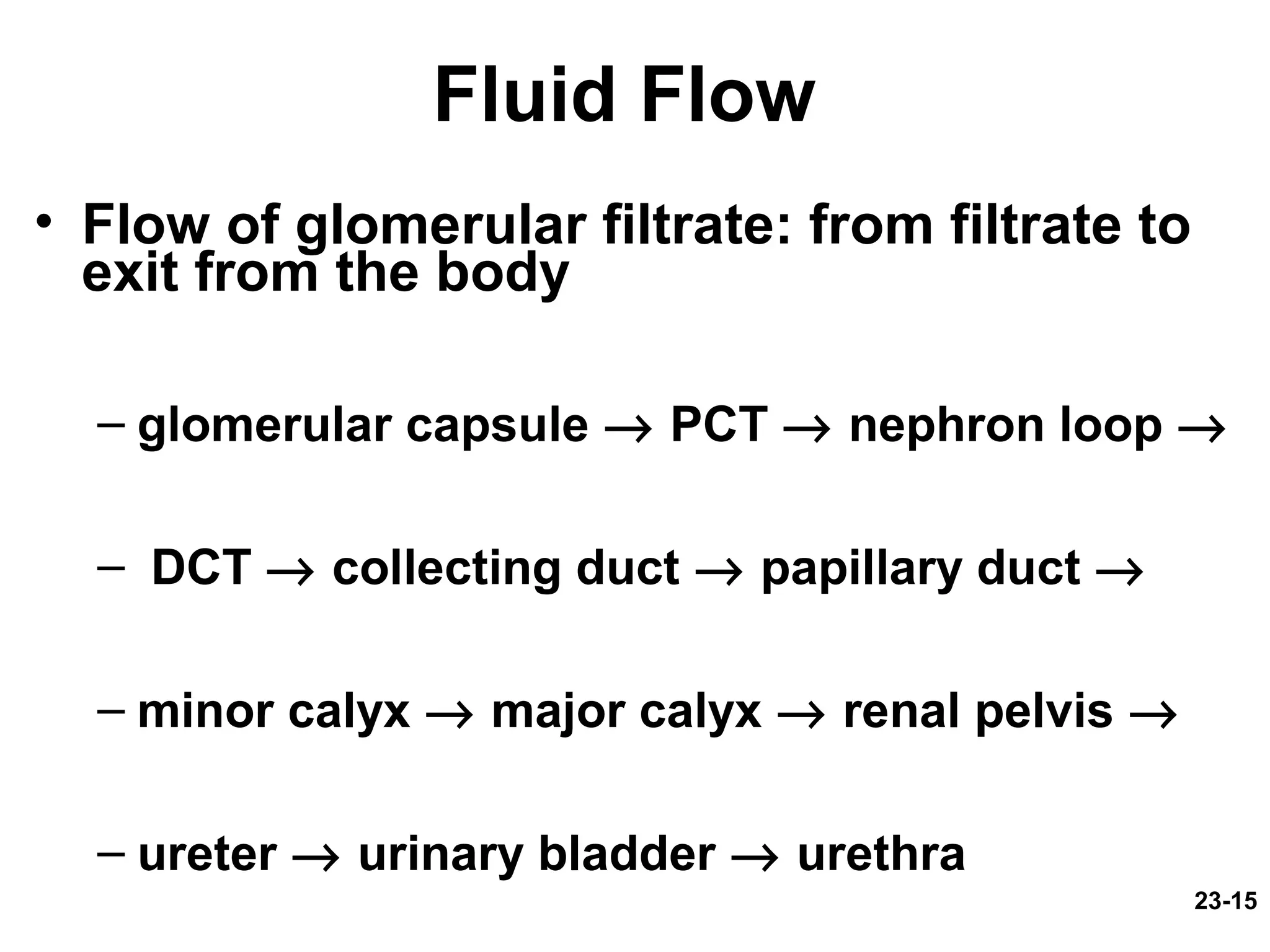
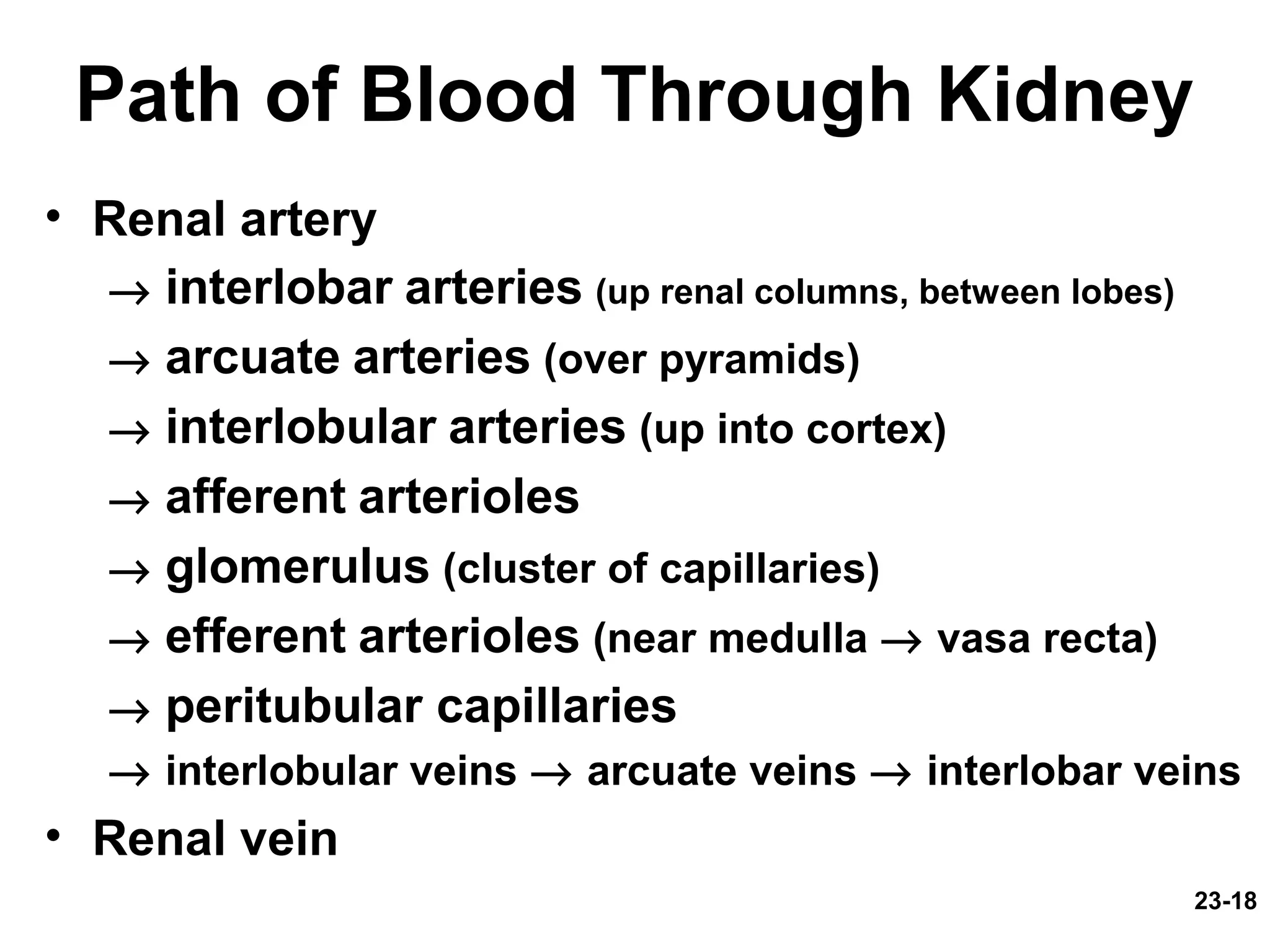
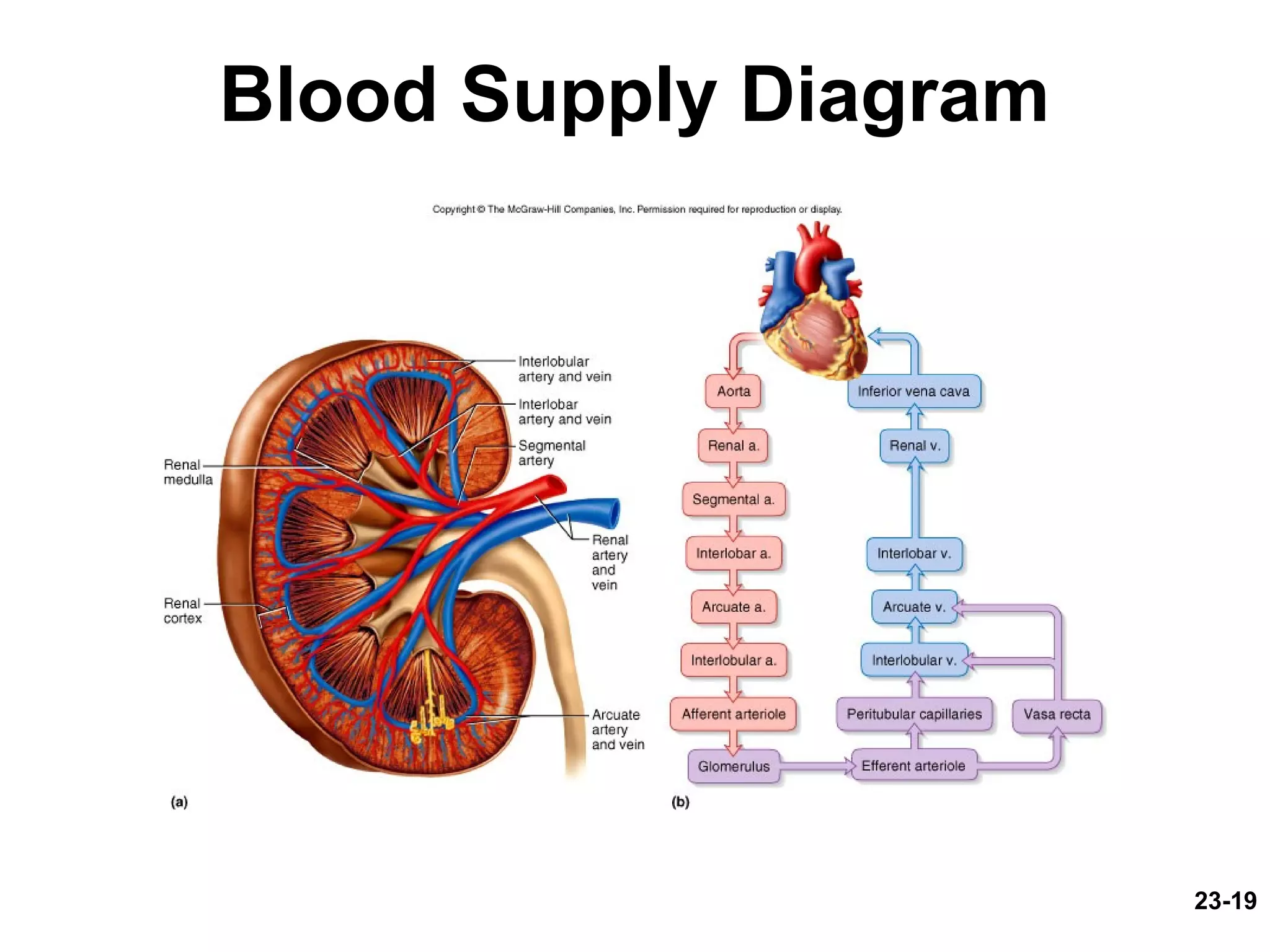
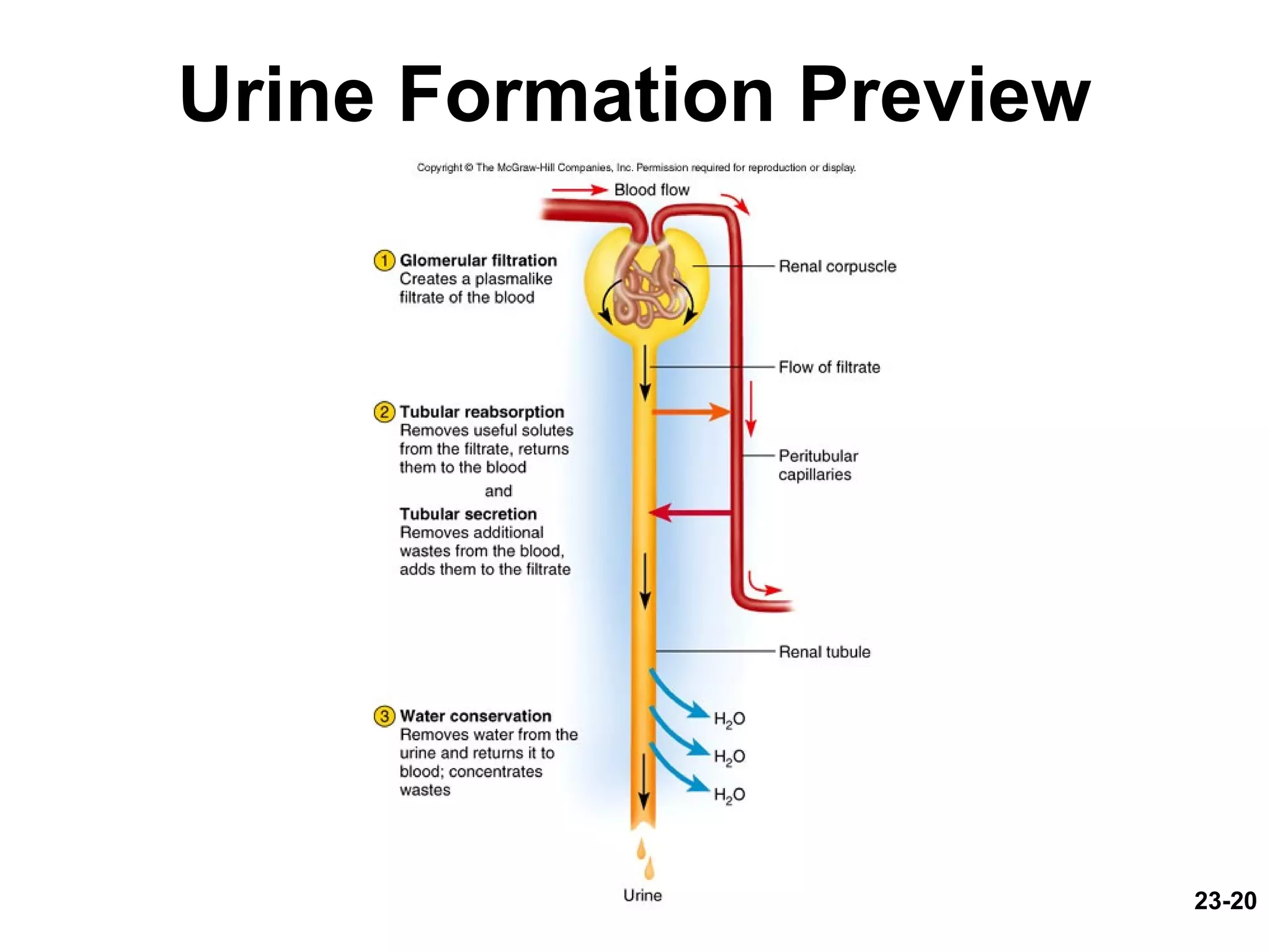
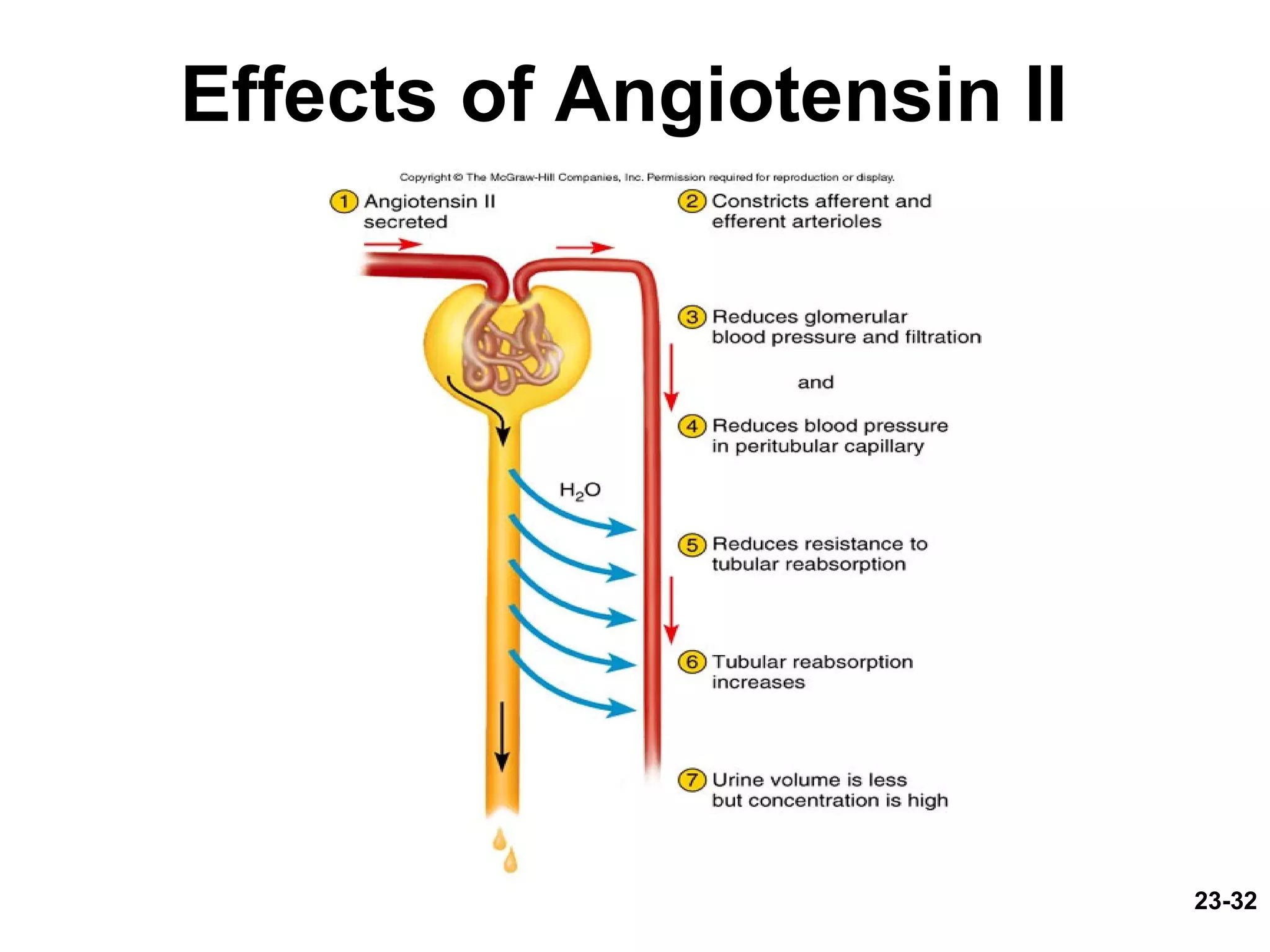
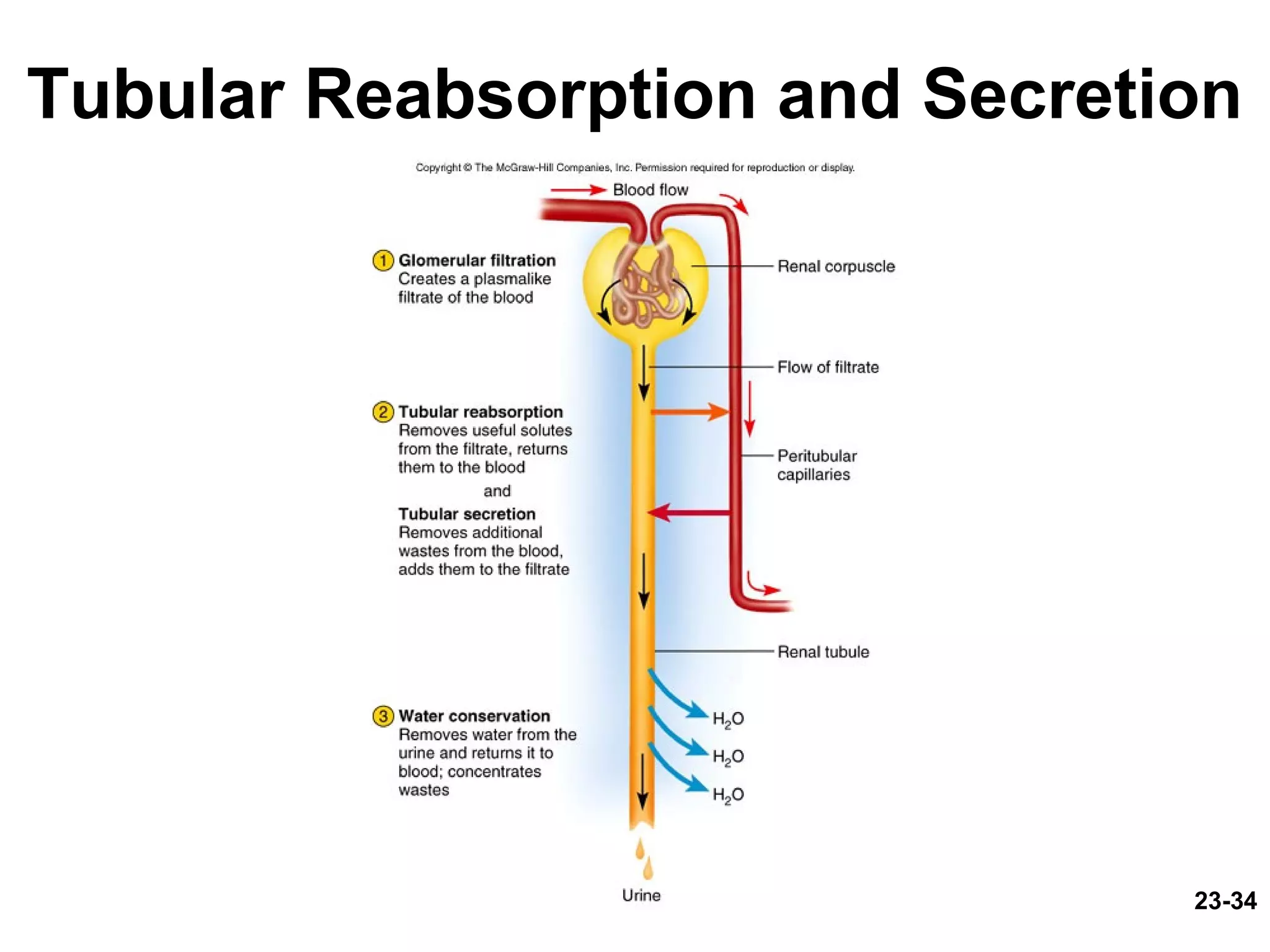
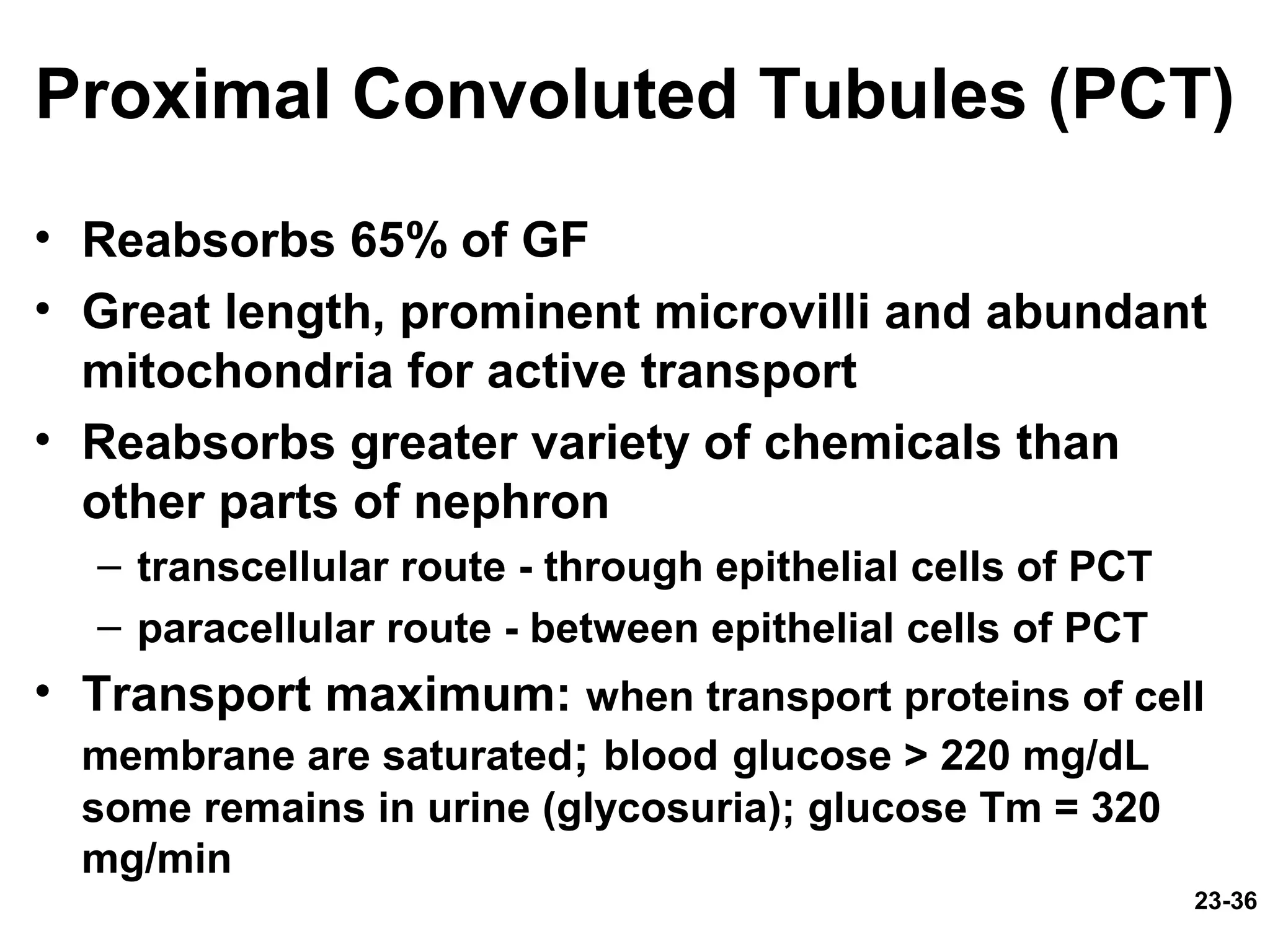
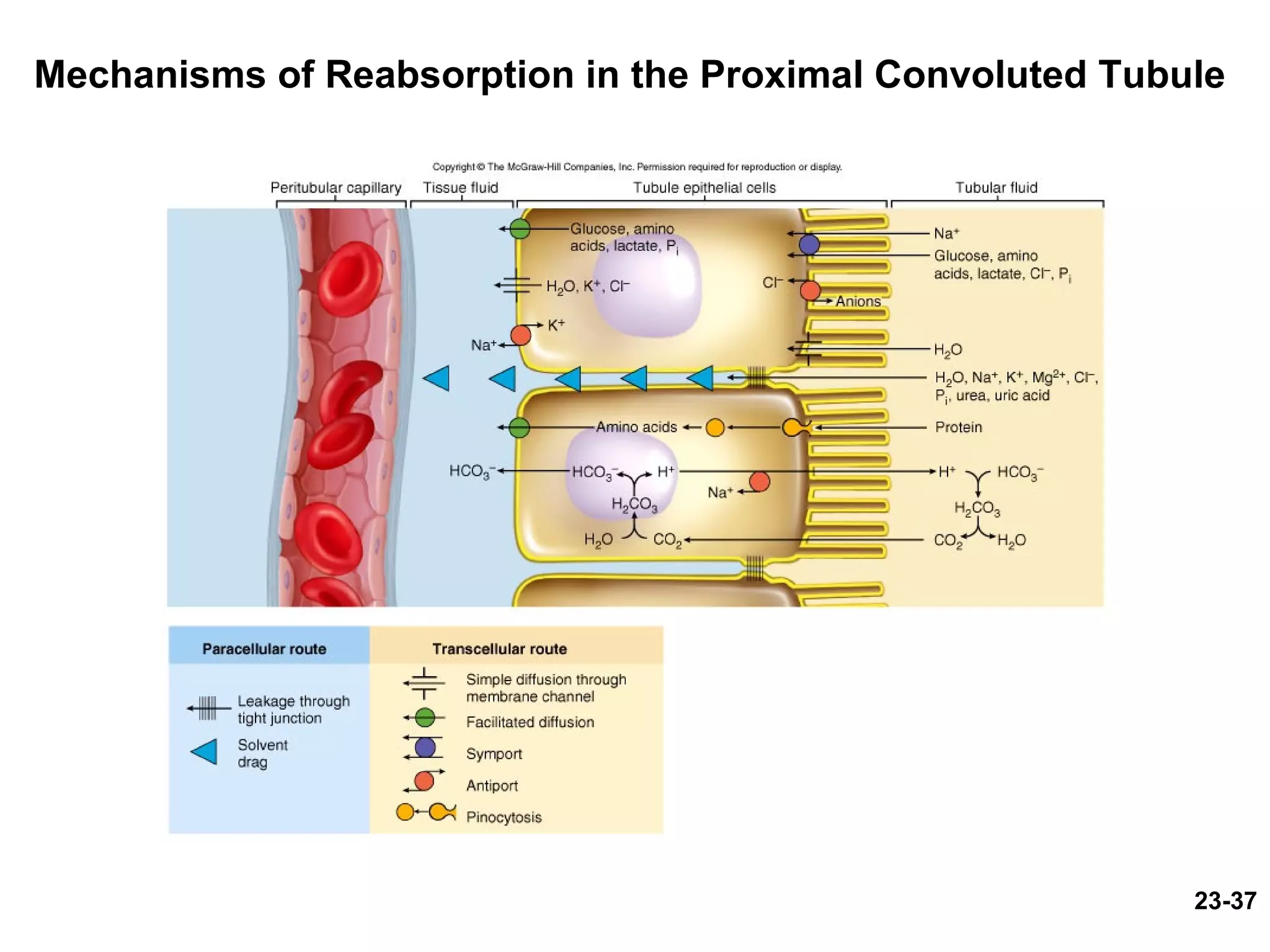
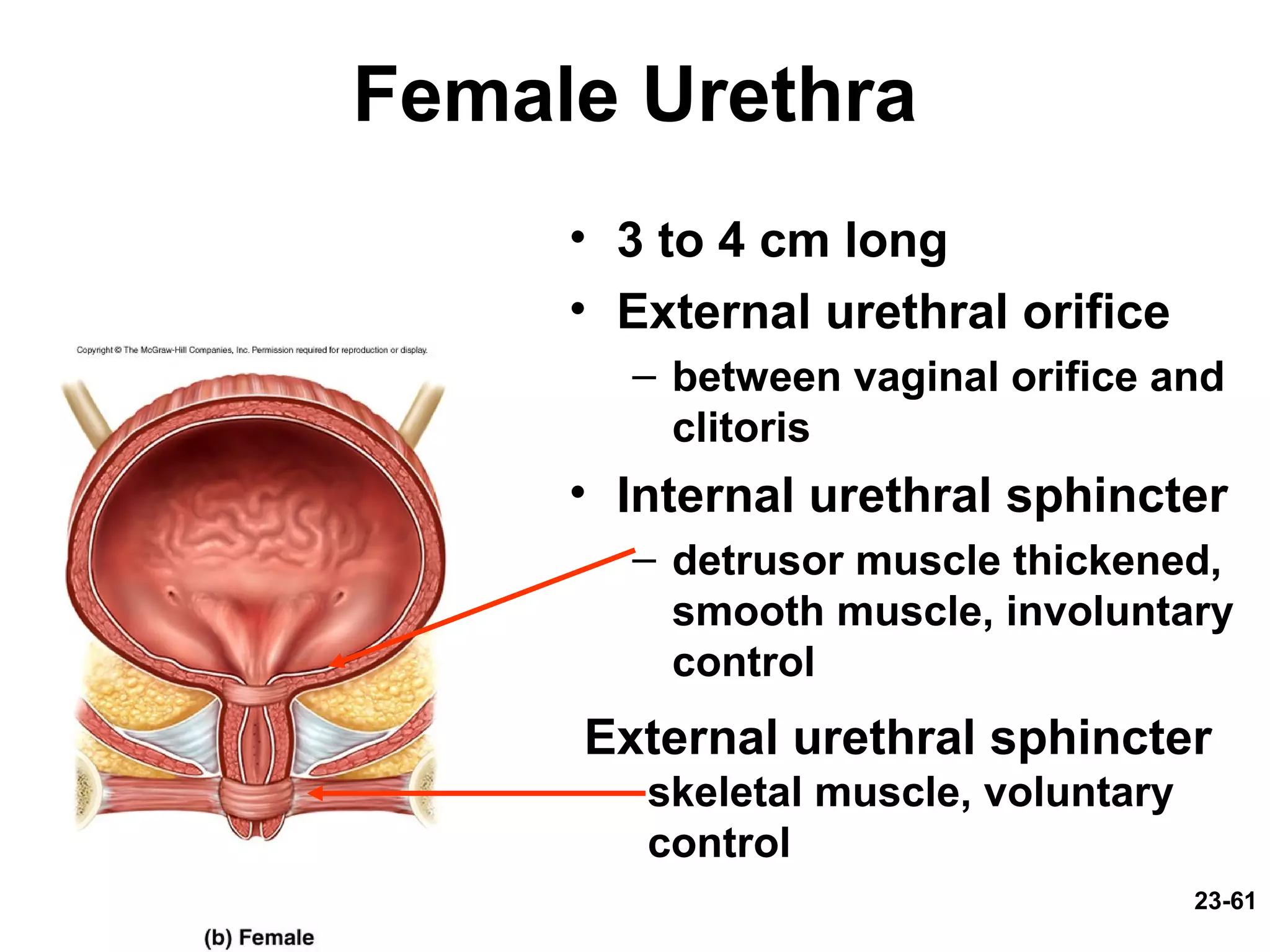
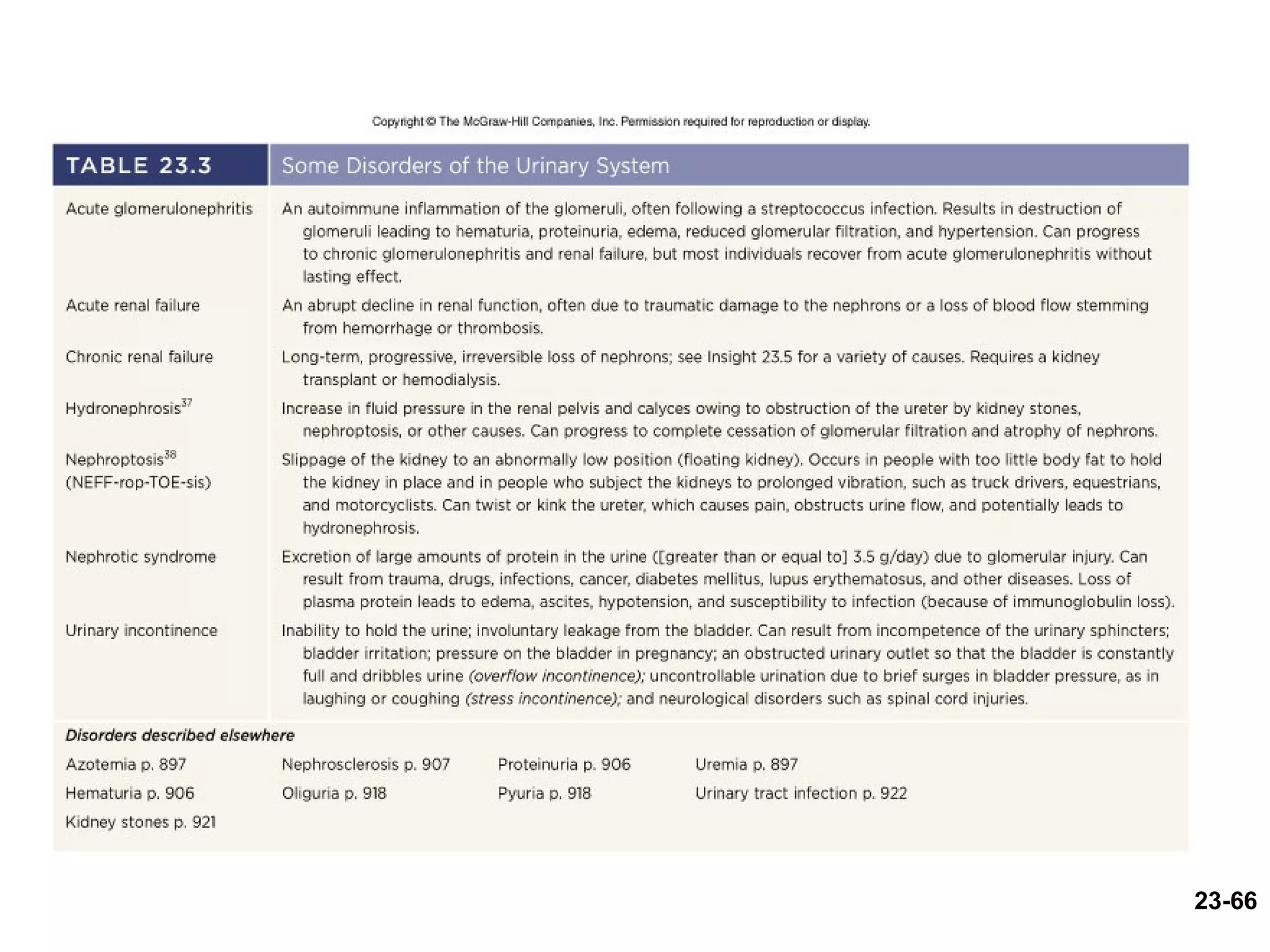
The urinary system filters wastes from the blood and removes them from the body as urine. The kidneys filter blood to form urine and regulate fluid and electrolyte balance. Each kidney contains millions of nephrons, the functional units of filtration. Urine is transported from the kidneys to the bladder via ureters and is stored in the bladder until elimination through the urethra. Hormones help regulate urine concentration and output to maintain fluid homeostasis.