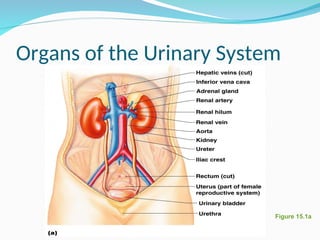
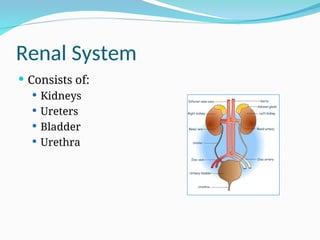
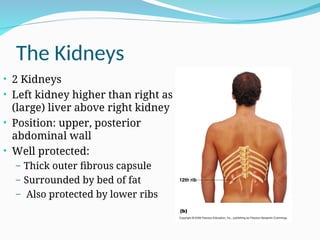
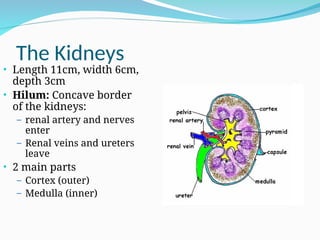
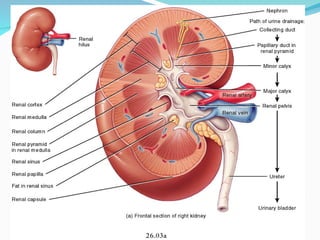
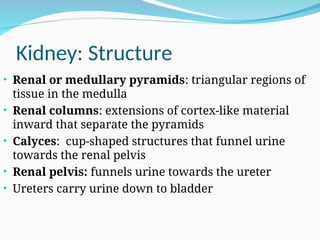
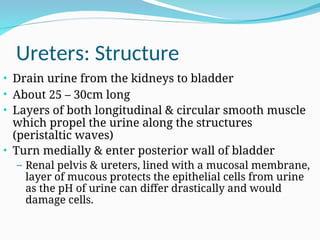
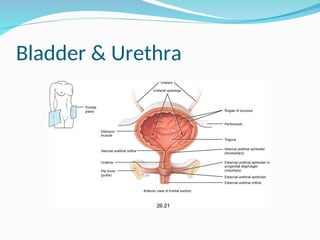
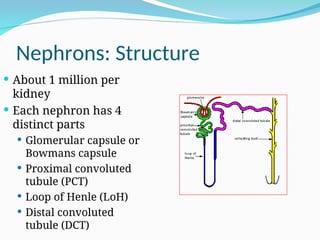
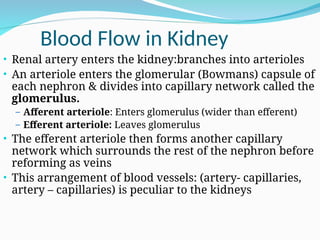
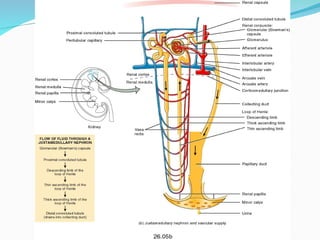
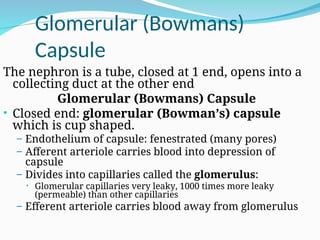
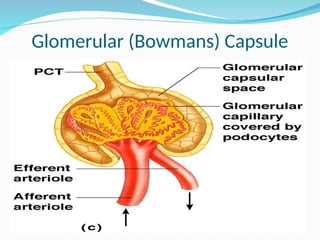
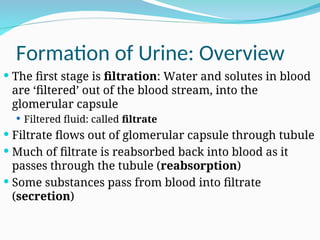
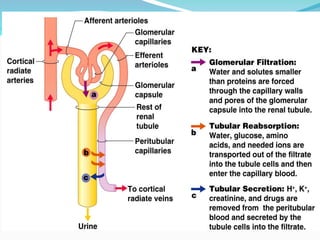
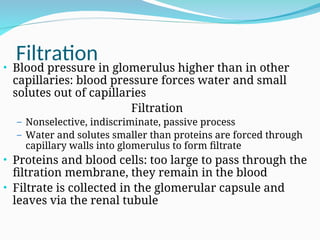
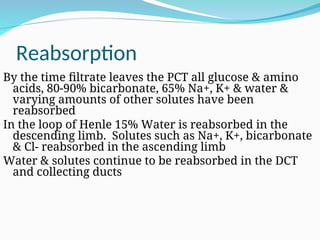
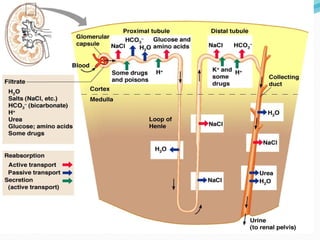
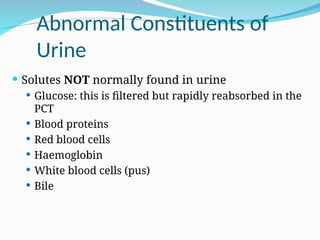
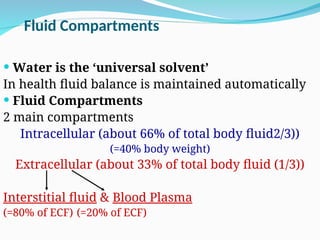
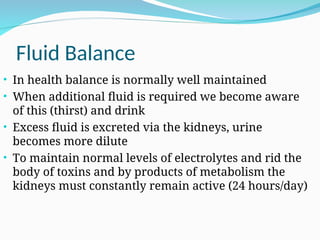
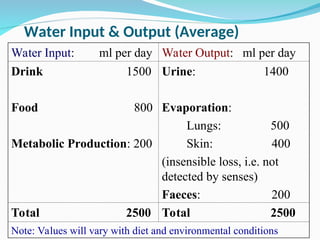
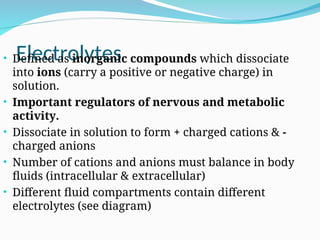
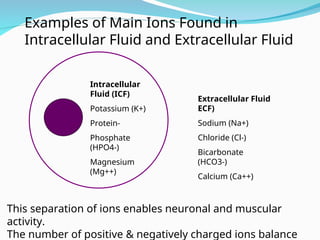
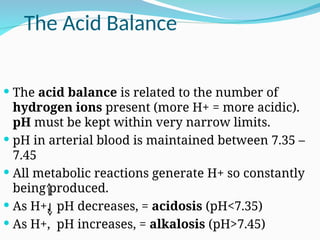
The document outlines the anatomy and functions of the renal system, detailing components such as kidneys, ureters, bladder, and urethra, as well as the processes involved in urine formation, including filtration, reabsorption, and secretion. It also discusses the hormonal regulation of fluid and electrolyte balance, emphasizing the kidneys' role in homeostasis and waste elimination. Additionally, the document covers fluid compartments, the significance of electrolytes, and the importance of maintaining acid-base balance.