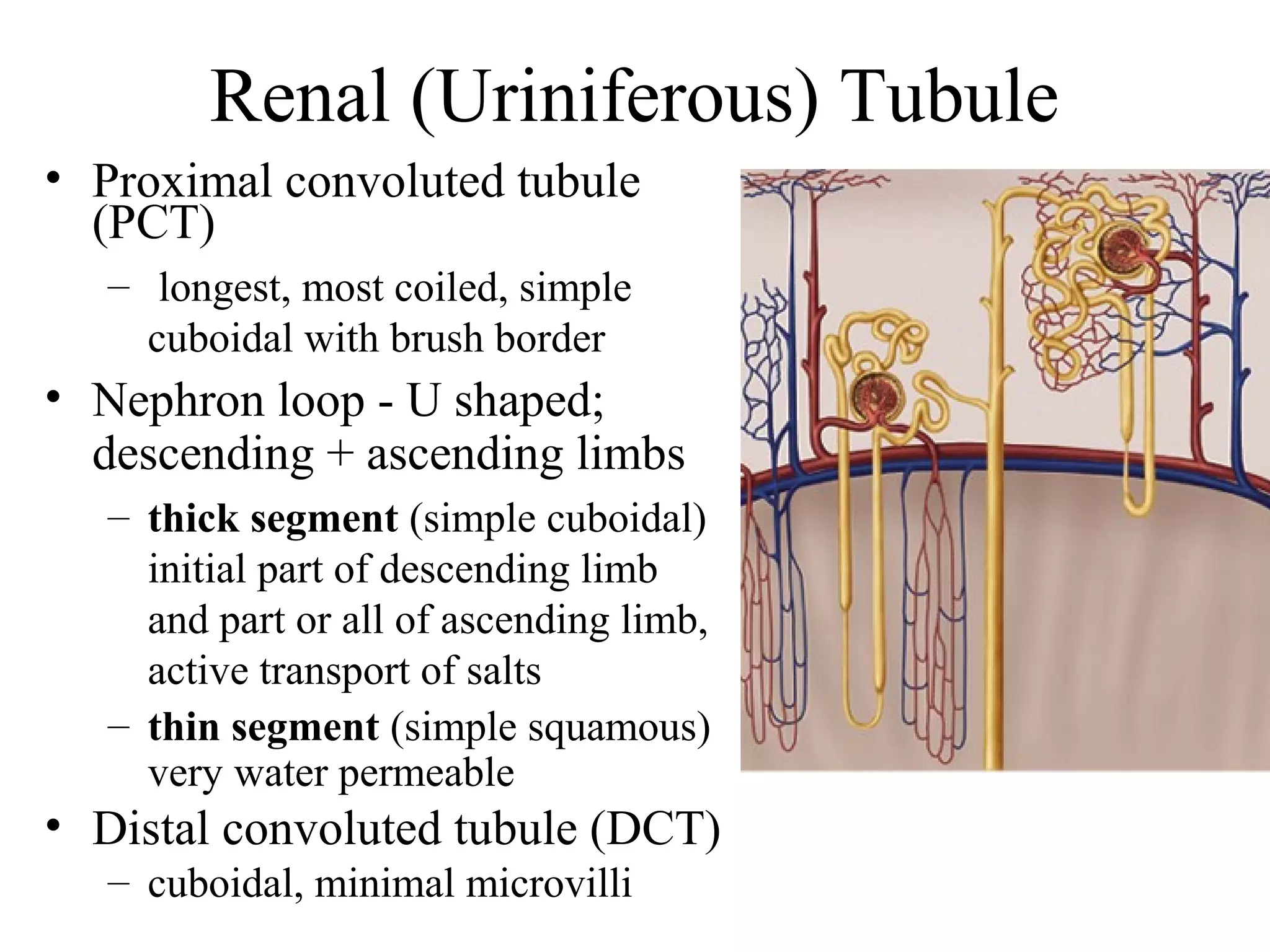
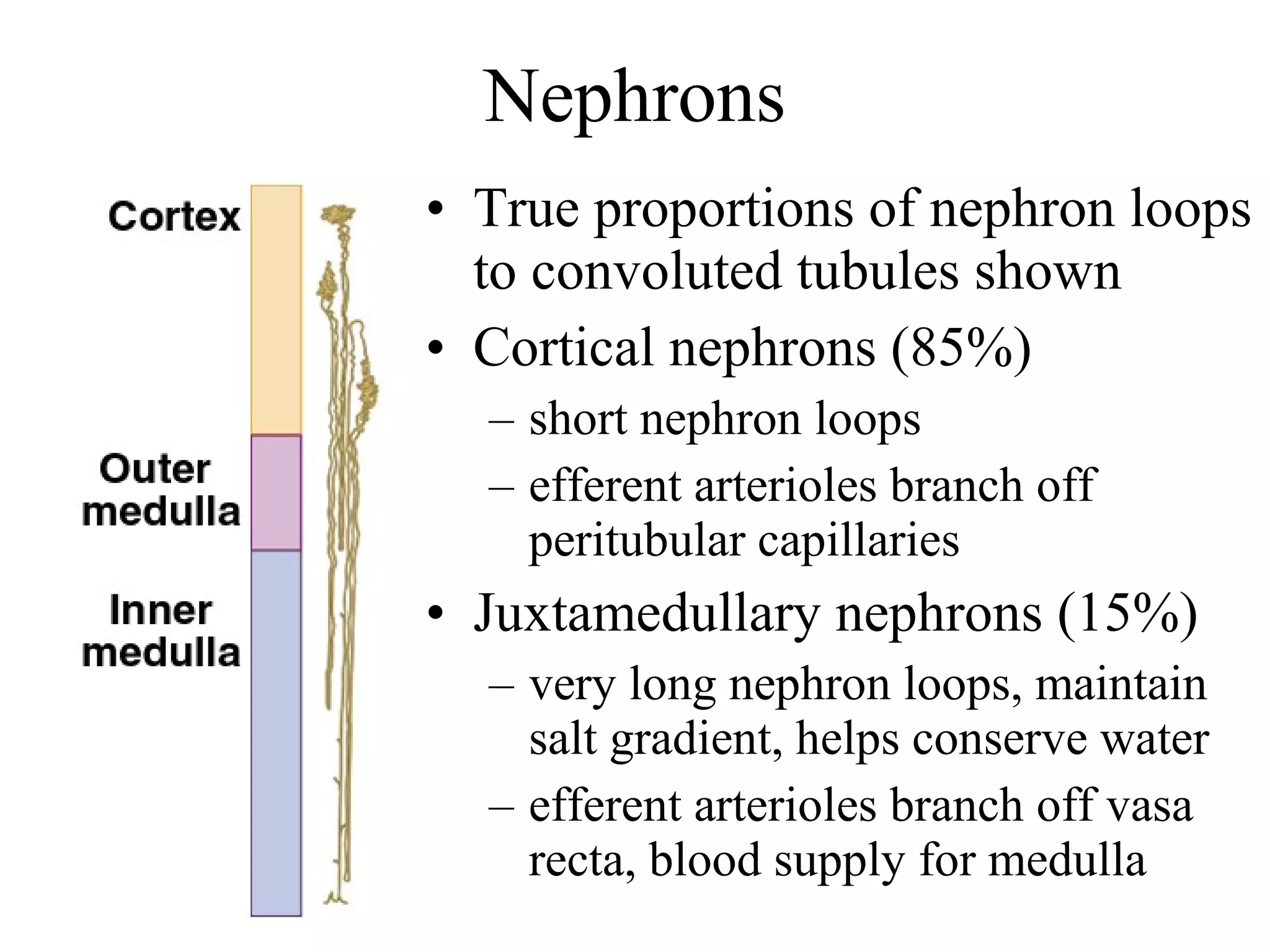
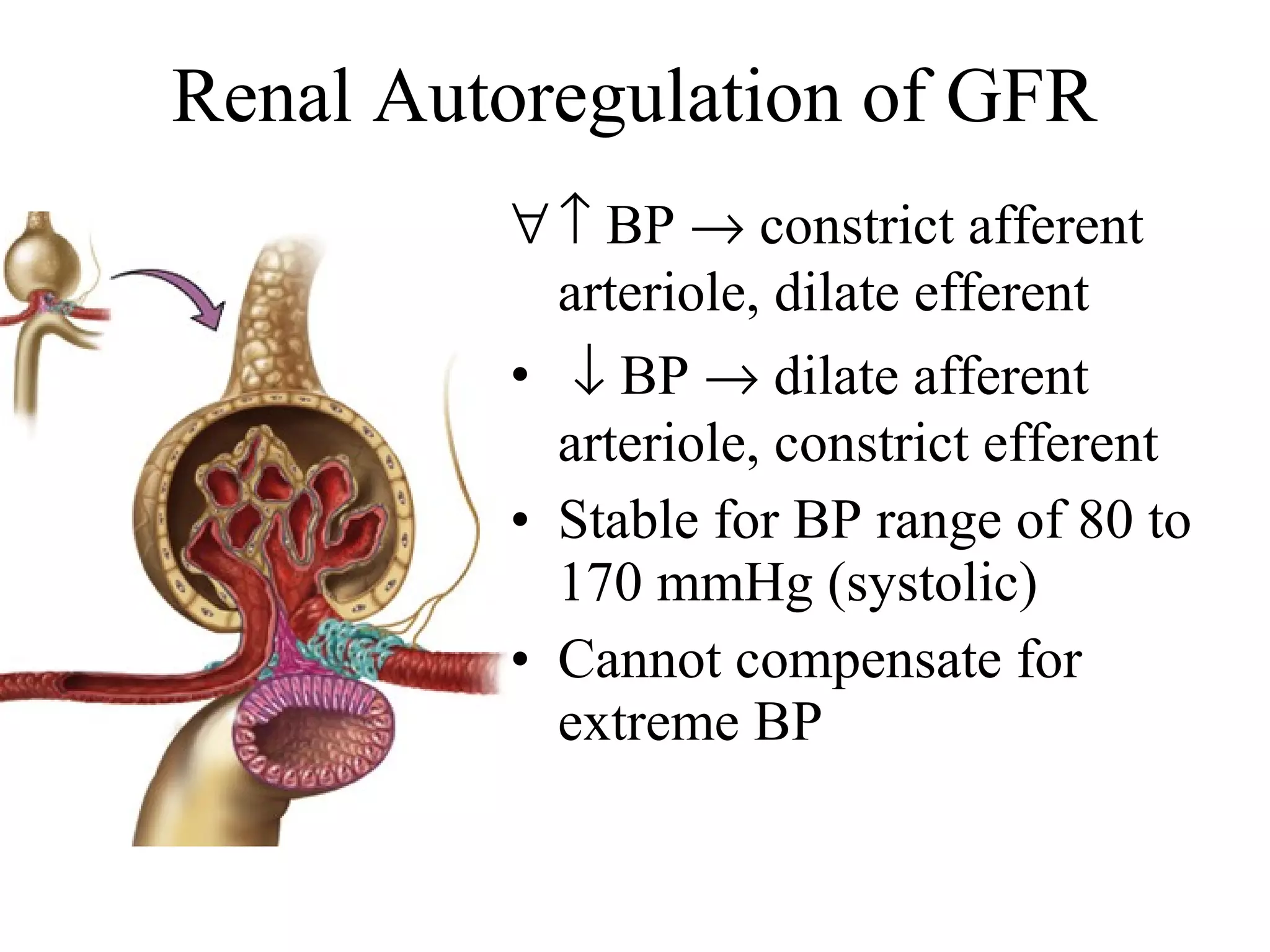
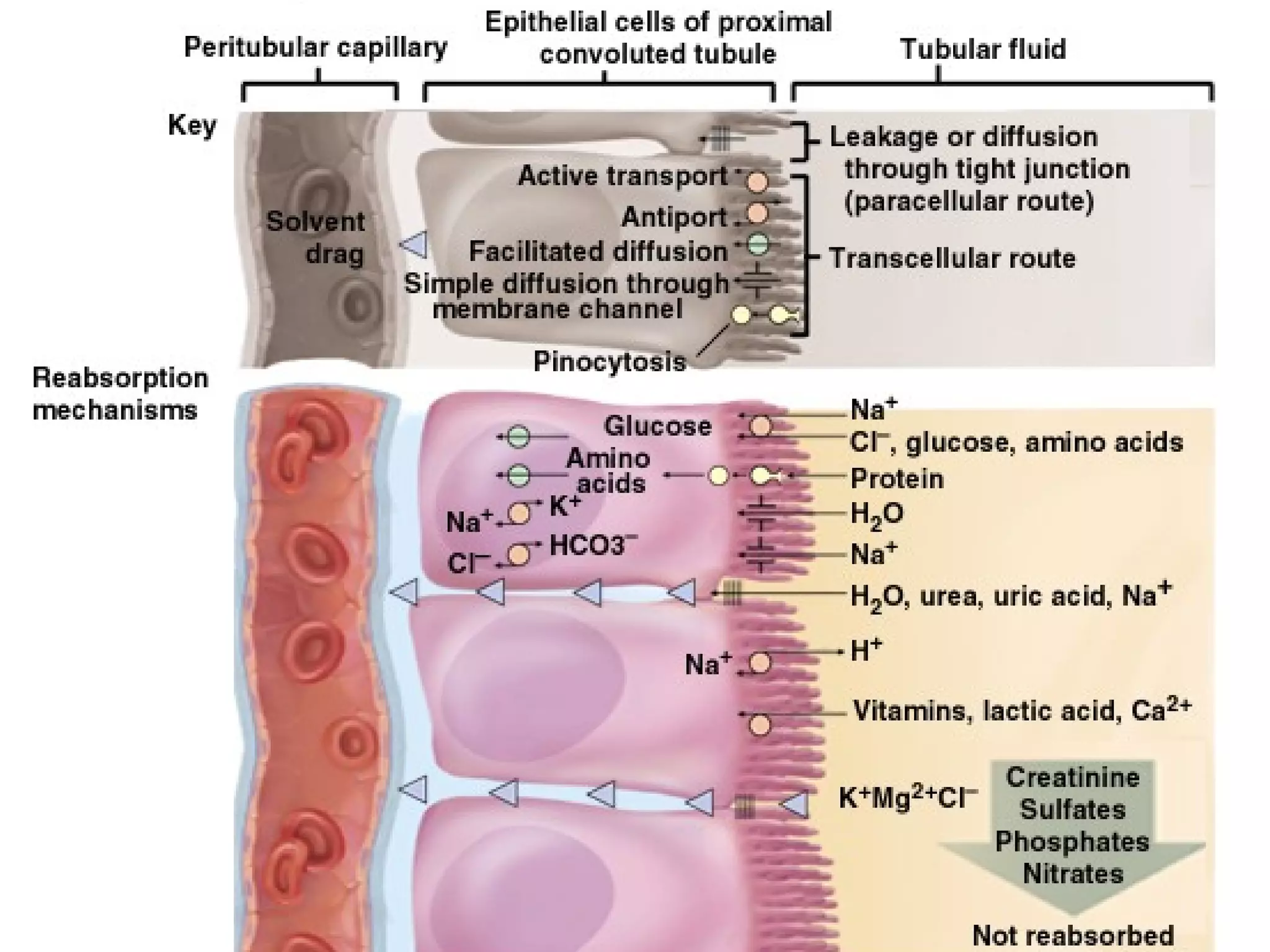
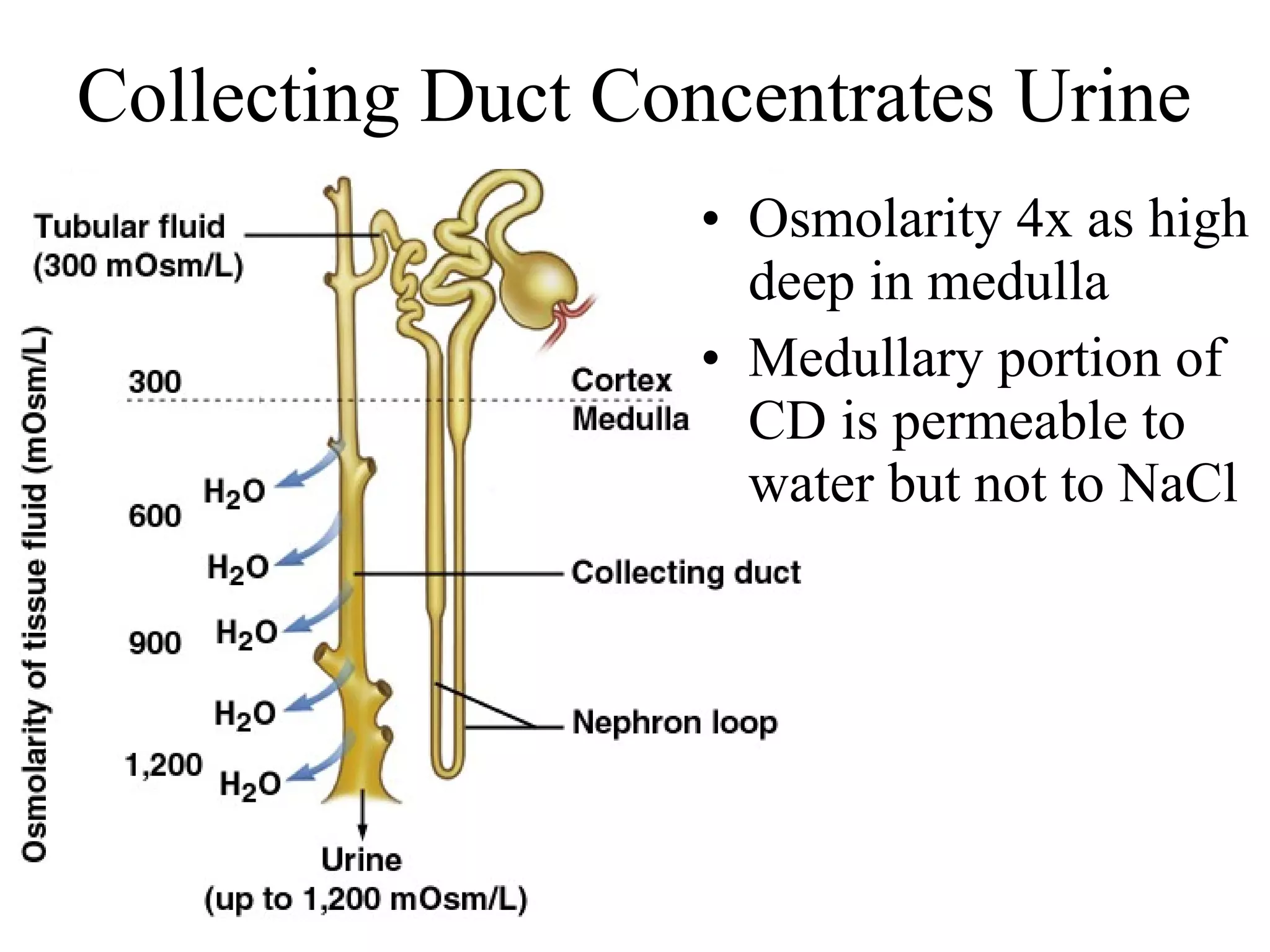
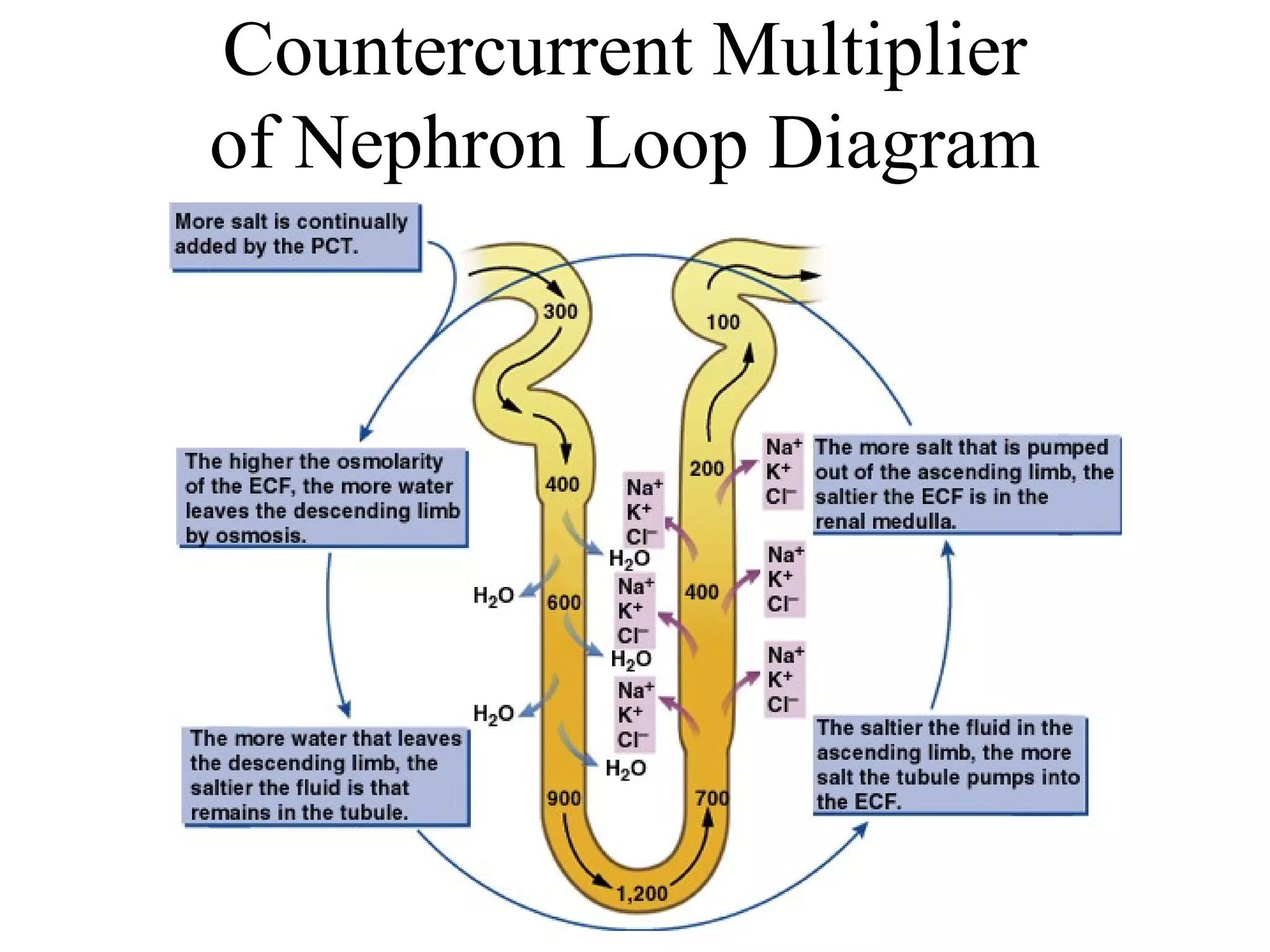
The urinary system filters wastes from the blood and regulates fluid balance through the kidneys and urine production. The kidneys contain nephrons which filter blood to form urine and regulate electrolyte and acid-base balance. Urine passes from the kidneys through ureters to the bladder and is eliminated through the urethra. Precise control of filtration, reabsorption and secretion allows the kidneys to regulate fluid balance and remove nitrogenous and other wastes from the body.