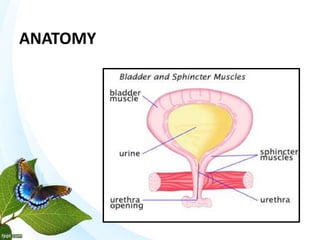
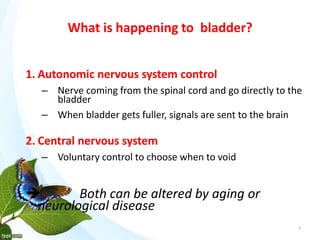
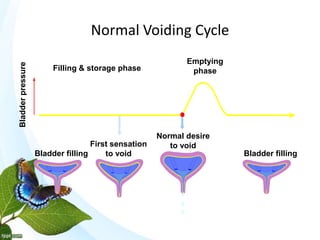
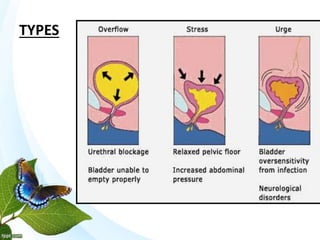
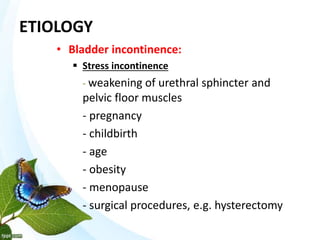
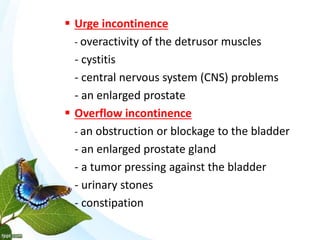
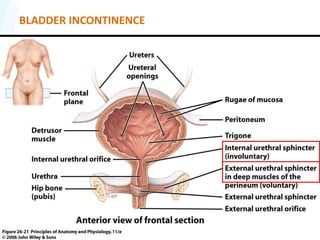
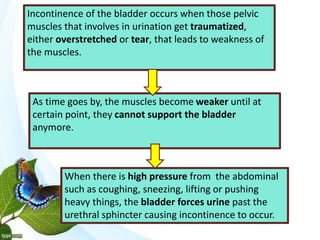
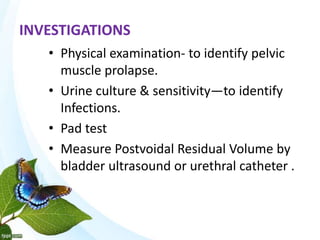
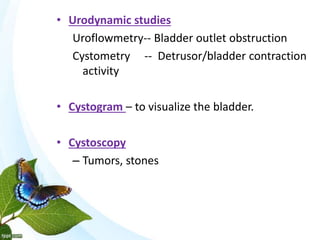
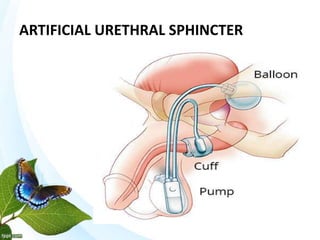
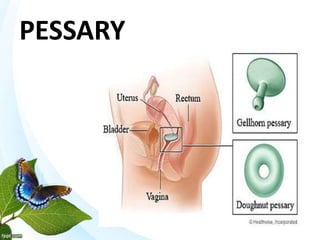
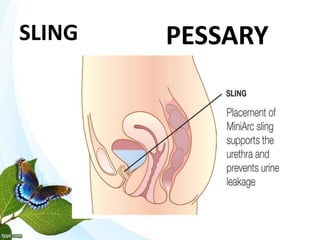
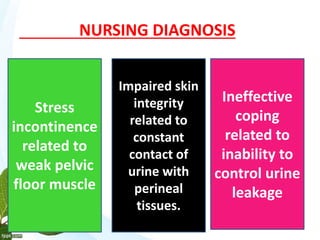
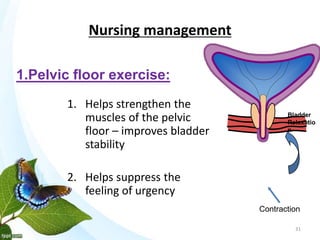
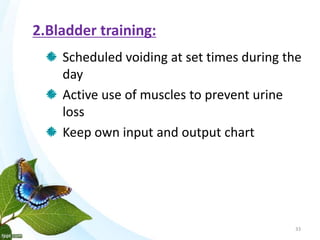
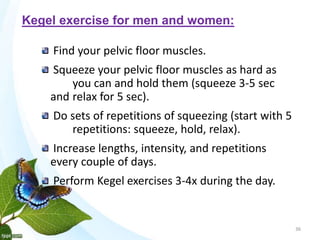
Urinary incontinence, or the inability to control urination, can be caused by issues with the bladder, urethra, or pelvic floor muscles. There are several types of incontinence including stress, urge, overflow, and mixed. Incontinence is evaluated through physical exams, urine tests, pad tests, and urodynamic studies. Treatment options include pelvic floor exercises, bladder training, medication, medical devices, and surgery to address the underlying causes. Nursing care focuses on strengthening muscles, managing symptoms, and preventing skin breakdown.