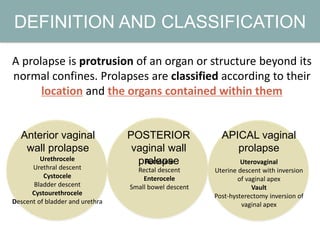
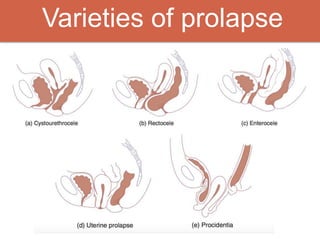
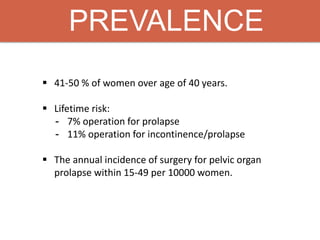
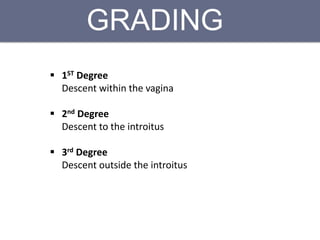
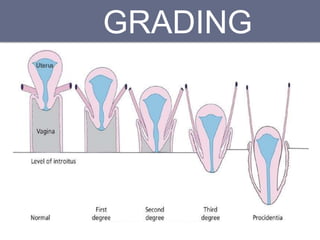
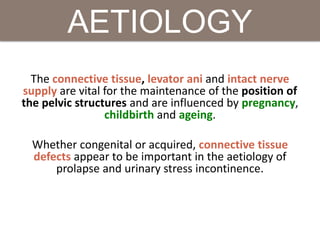
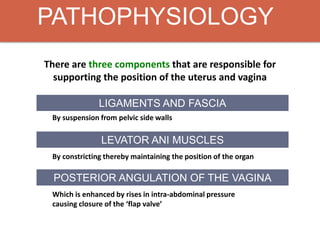
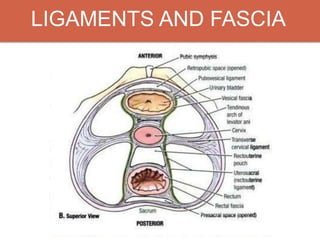
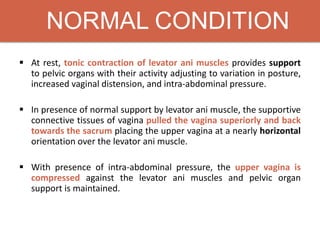
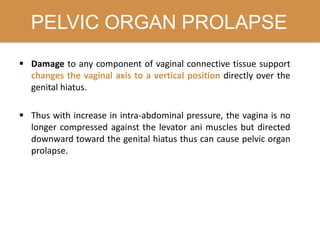
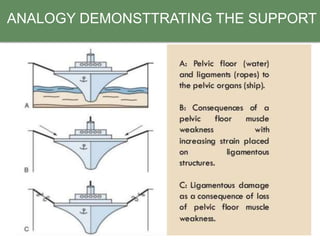
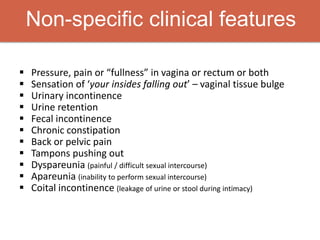
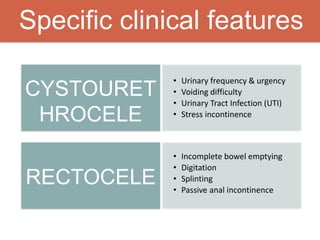
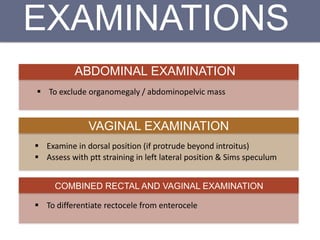
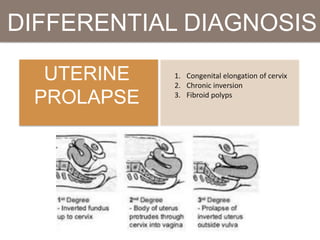
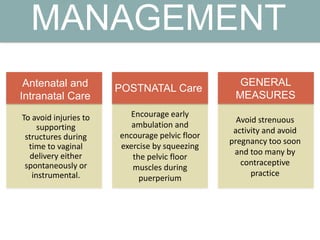
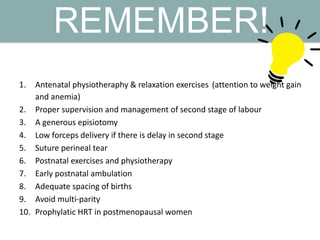
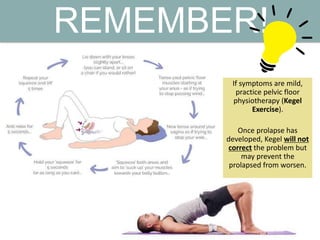
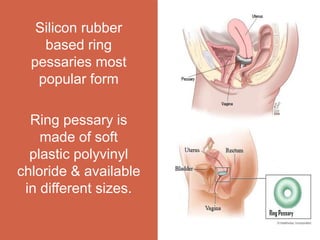
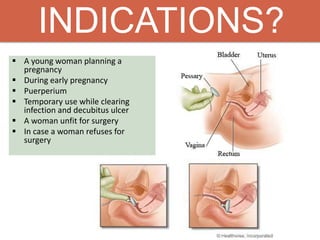
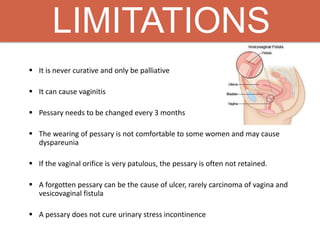
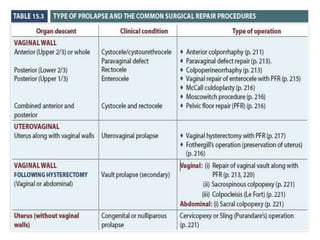
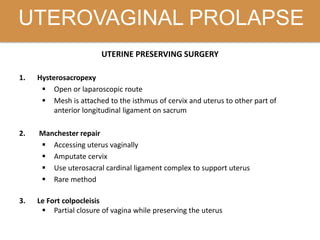
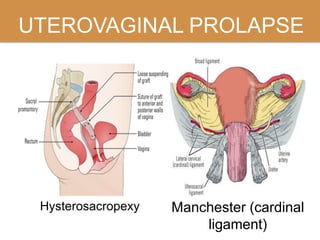
Pelvic organ prolapse is the descent of pelvic organs from their normal position. It is caused by weakness in the pelvic floor muscles and supporting tissues. Prolapse can affect the bladder, uterus, rectum, or small intestine and is graded based on the degree of descent. Risk factors include childbirth, age, obesity, and chronic coughing. Symptoms vary depending on the affected organ but may include pressure, pain, urinary issues, or bowel dysfunction. Treatment ranges from pelvic floor exercises to pessaries to surgery based on severity. Surgical options aim to restore anatomy and support the pelvic organs.