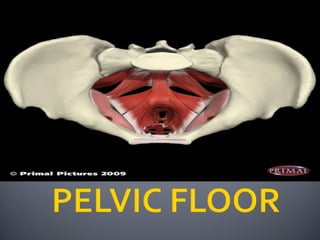
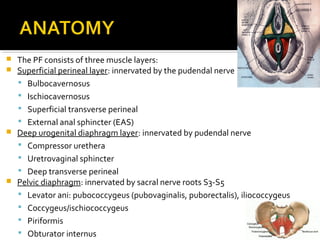
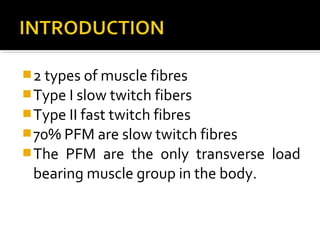
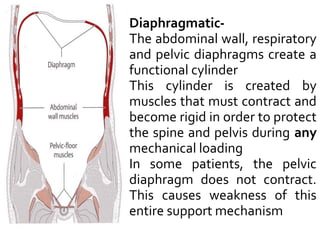
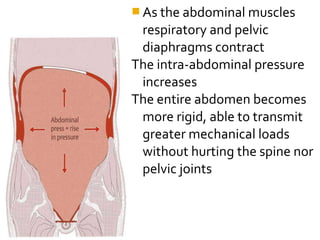
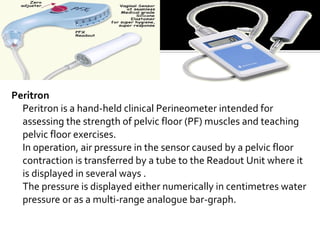
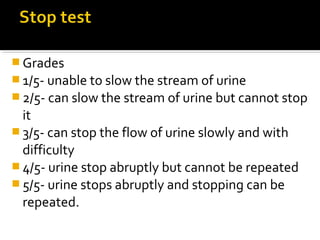
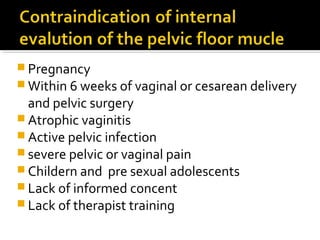
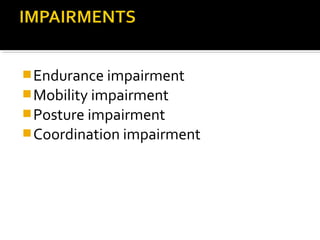
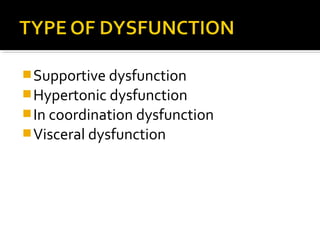
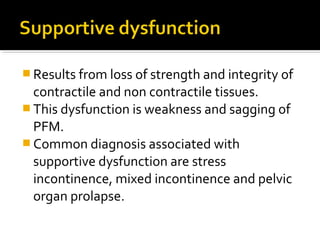
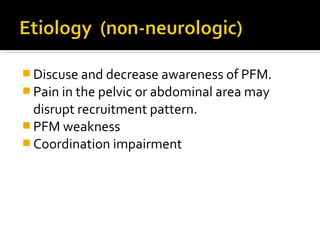
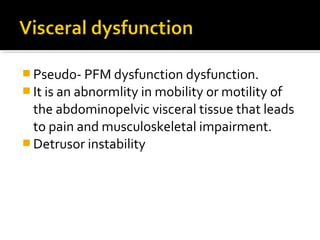
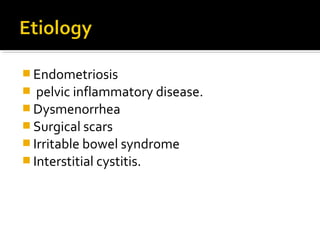
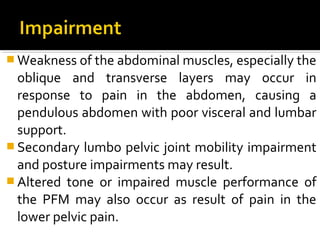
The document summarizes the pelvic floor muscles (PFM), including their three layers, innervation, fiber types, functions in support, continence and sexual function. Assessment methods are described like digital examination grading scales and tools like perineometers. Dysfunctions are outlined such as supportive, hypertonic, incoordination and visceral. Causes and characteristics are provided for each.