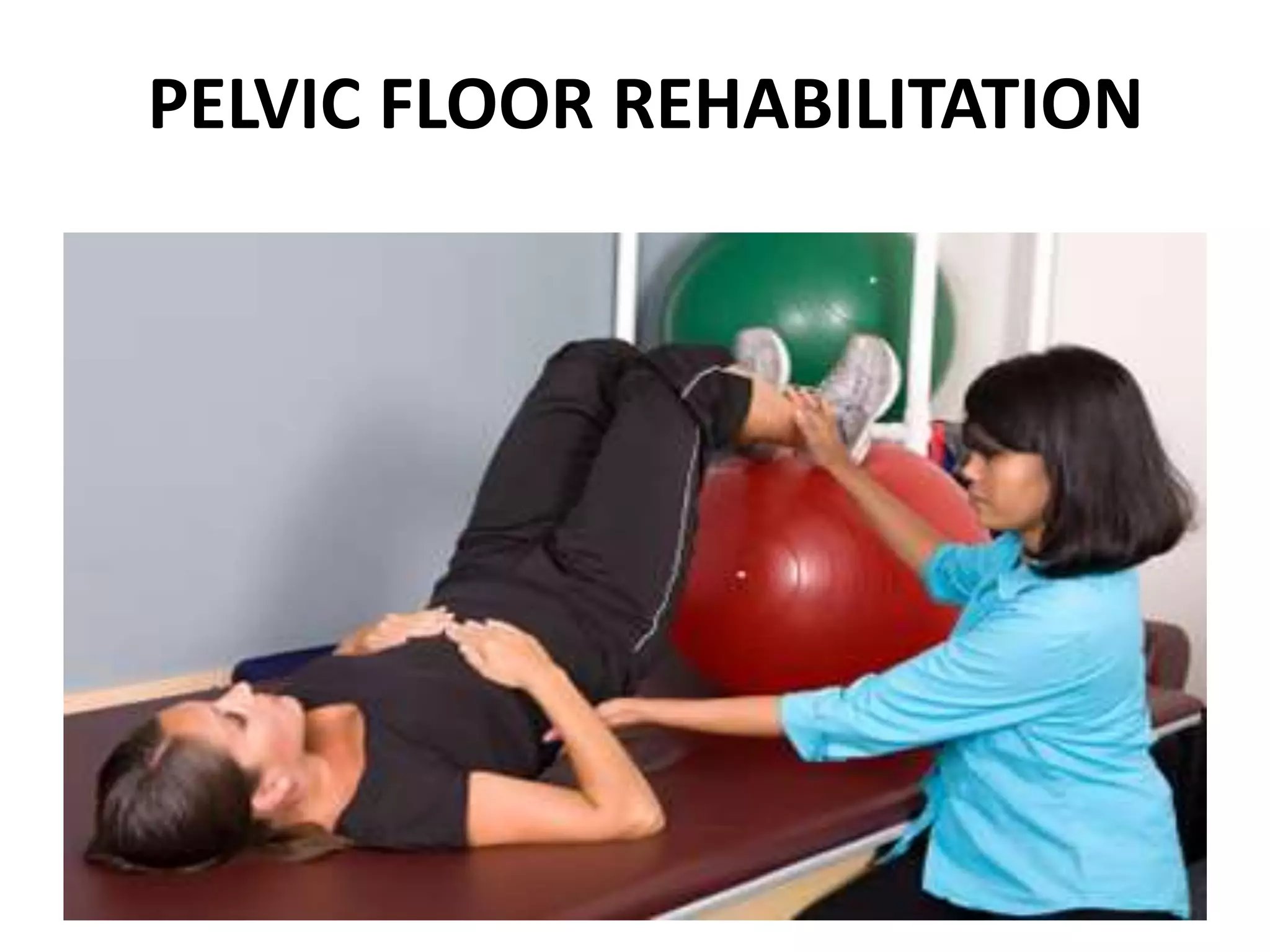
The document discusses pelvic floor rehabilitation, including identifying the pelvic floor muscles, common pelvic floor exercises, proper technique, common errors to avoid, and functional retraining exercises like coughing and sneezing that require coordinated pelvic floor and abdominal muscle activation.