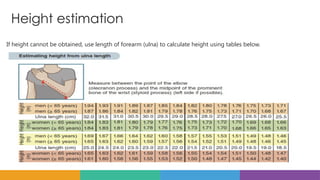
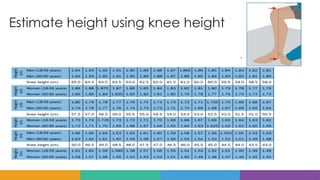
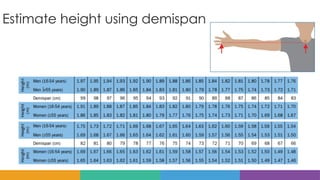
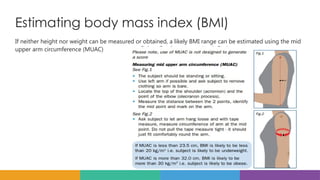
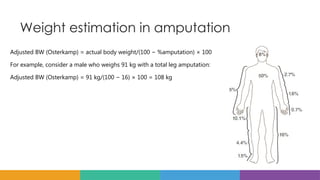
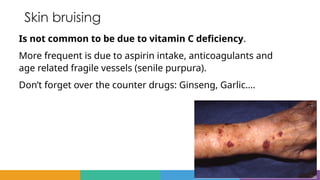
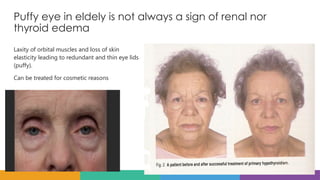
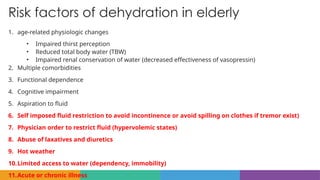
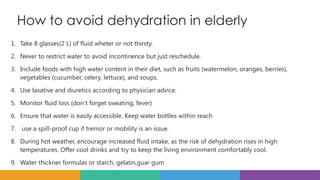
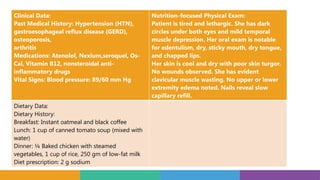
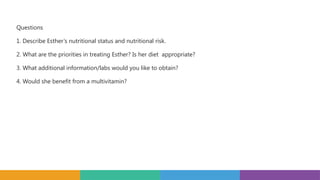
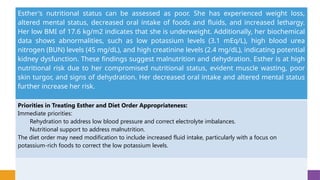
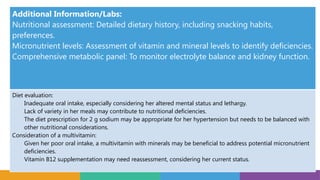
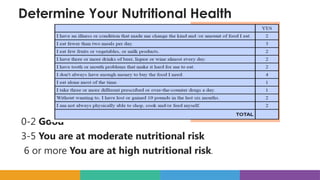
The document provides guidelines on geriatric nutrition, covering challenges in assessing body weight and nutritional status in elderly patients, and highlights specific conditions affecting appetite and hydration in this population. It discusses the importance of regular monitoring of measurements like mid upper arm circumference (MUAC) for tracking weight changes and addresses the complexities involved in diagnosing dehydration and nutritional deficiencies. A case study of an elderly female, Esther, exemplifies the critical need for nutritional support, hydration, and further assessment due to her malnutrition and dehydration signs.