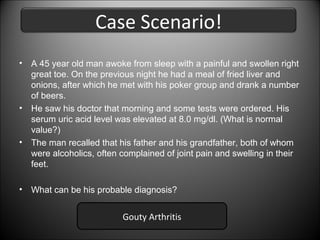
A 45-year-old man awoke with a painful and swollen right great toe after eating fried liver and drinking beer the night before. His uric acid level was elevated at 8.0 mg/dl, above the normal range. Both his father and grandfather, who were alcoholics, often had joint pain and swelling in their feet. The man likely has gouty arthritis, which is caused by elevated uric acid levels and is known to be associated with alcohol consumption and genetic predisposition.







![Hyperuricemia
Defined as a plasma urate concentration > 7.0 mg/dl
Increased production of uric acid
Primary
• Adenine phosphoribosyl
transferase (APRT)
• Hypoxanthine-Guanine
phosphoribosyl
transferase [Lesch-Nyhan
Syndrome]
• Increased phosphoribosyl
pyrophosphatase activity.
Secondary
• Myeloproliferative
disease
• Lymphoproliferative
disease
• Hemolitic anemia
• Drugs:
Low-doses
salicylate,
diuretis,
pyrazinamide,
ethambutol,
nicotinamide,
ethanol,
cytotoxic
drugs.
Decreased excretion of uric acid
• Alterated uric acid excretion could result
from decreased glomerular filtration,
decreased tubular secretion or enhanced
tubular reabsorption.
• Diabetic ketoacidosis, starvation,
lactic
acidosis, and salicylate intoxication are
accompanied by accumulations of organic
acids
(B-hydroxybutyrate, acetoacetate,
lactate or salicylates) that compete with
urate for tubular secretion.](https://image.slidesharecdn.com/uricacid-131021102938-phpapp02/85/Uric-acid-11-320.jpg)


![Glucose-6-phosphatase (G6Pase) deficiency
1. Also known as von Gierke's disease.
2. Unable to dephosphorylate G6P.
3. Glucose-6-P goes into Pentose Phosphate shut.
4. Excess production of ribose-5-phosphate.
5. Cause hypoglcemia as liver fails to form glucose from
glycogen. [Glycogen storage disease type I (GSD I)]](https://image.slidesharecdn.com/uricacid-131021102938-phpapp02/85/Uric-acid-14-320.jpg)


