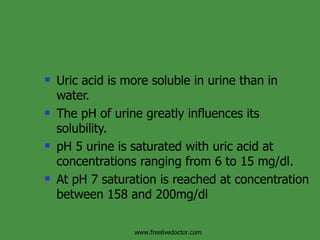
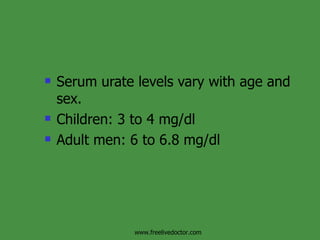
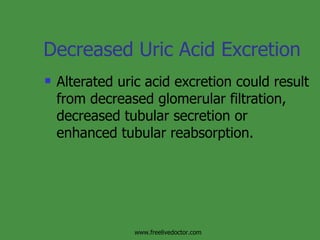
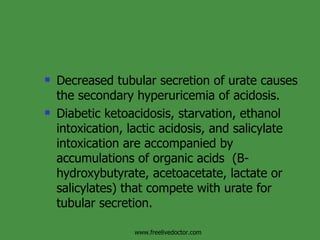
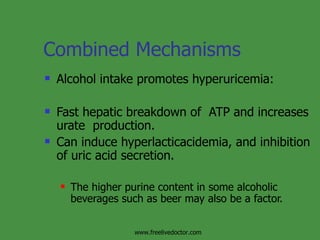
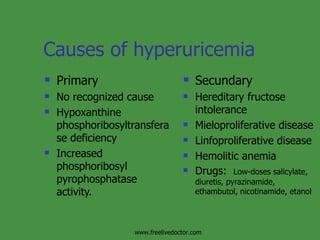
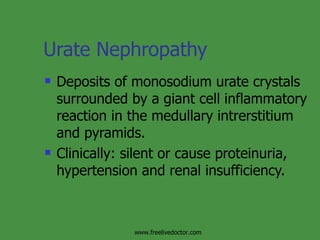
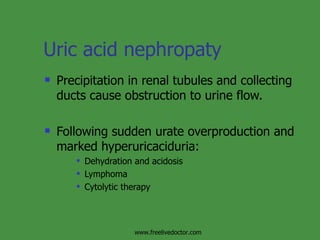
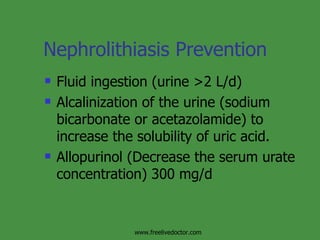
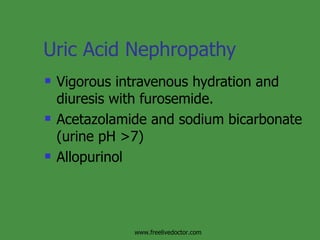
The document discusses hyperuricemia and gout. It defines hyperuricemia as a plasma urate concentration greater than 7.0 mg/dl and can result from increased urate production, decreased urate excretion, or a combination. Gout is caused by the deposition of monosodium urate crystals in the joints and other tissues, which can cause acute inflammatory arthritis. The first metatarsophalangeal joint is commonly affected. Treatment involves medications like colchicine, NSAIDs, or glucocorticoids for acute attacks and urate-lowering therapies for long-term management.