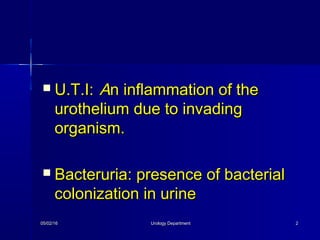
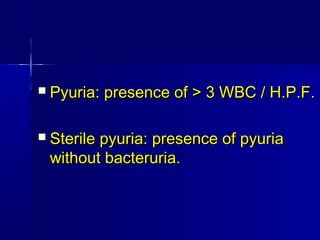
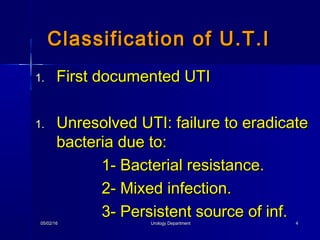
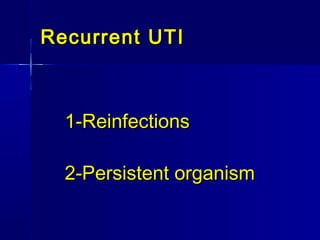
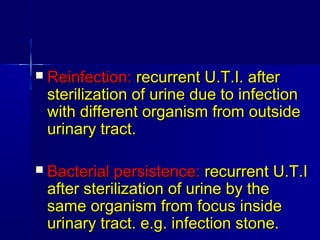
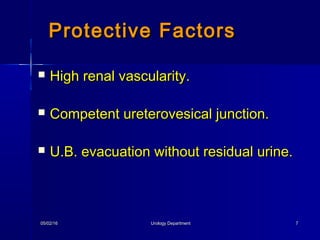
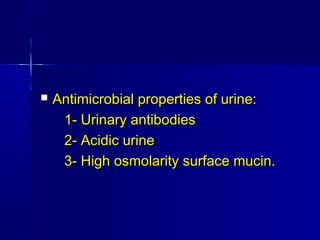
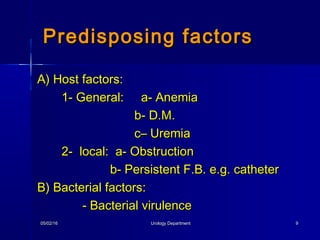
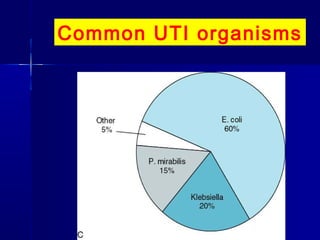
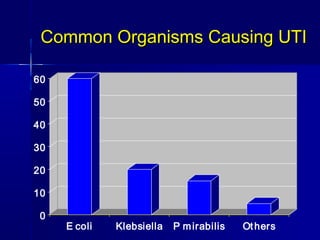
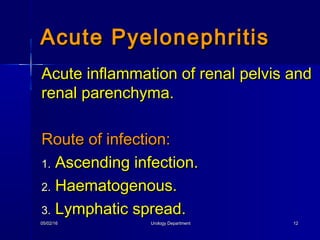
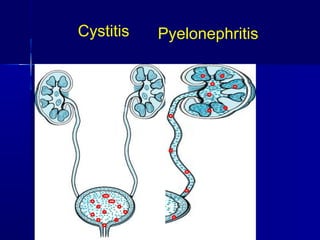
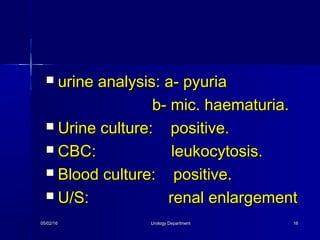
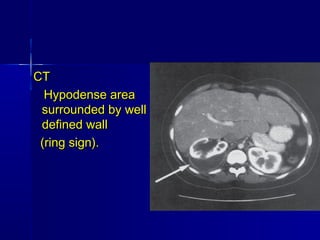
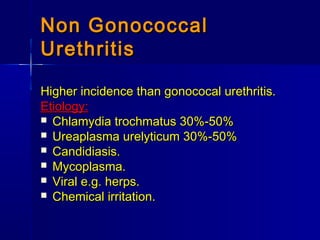
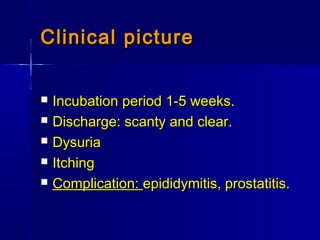
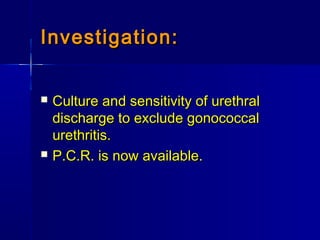
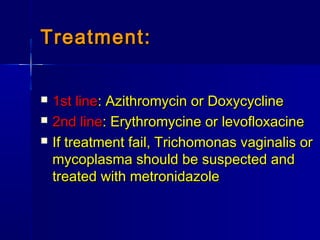
This document discusses various types of urinary tract infections including non-specific UTIs, acute cystitis, acute pyelonephritis, perinephric abscess, chronic pyelonephritis, and prostatitis. It defines key terms, describes clinical features and investigations, and outlines treatment approaches for each condition. Common organisms causing UTIs are also listed.