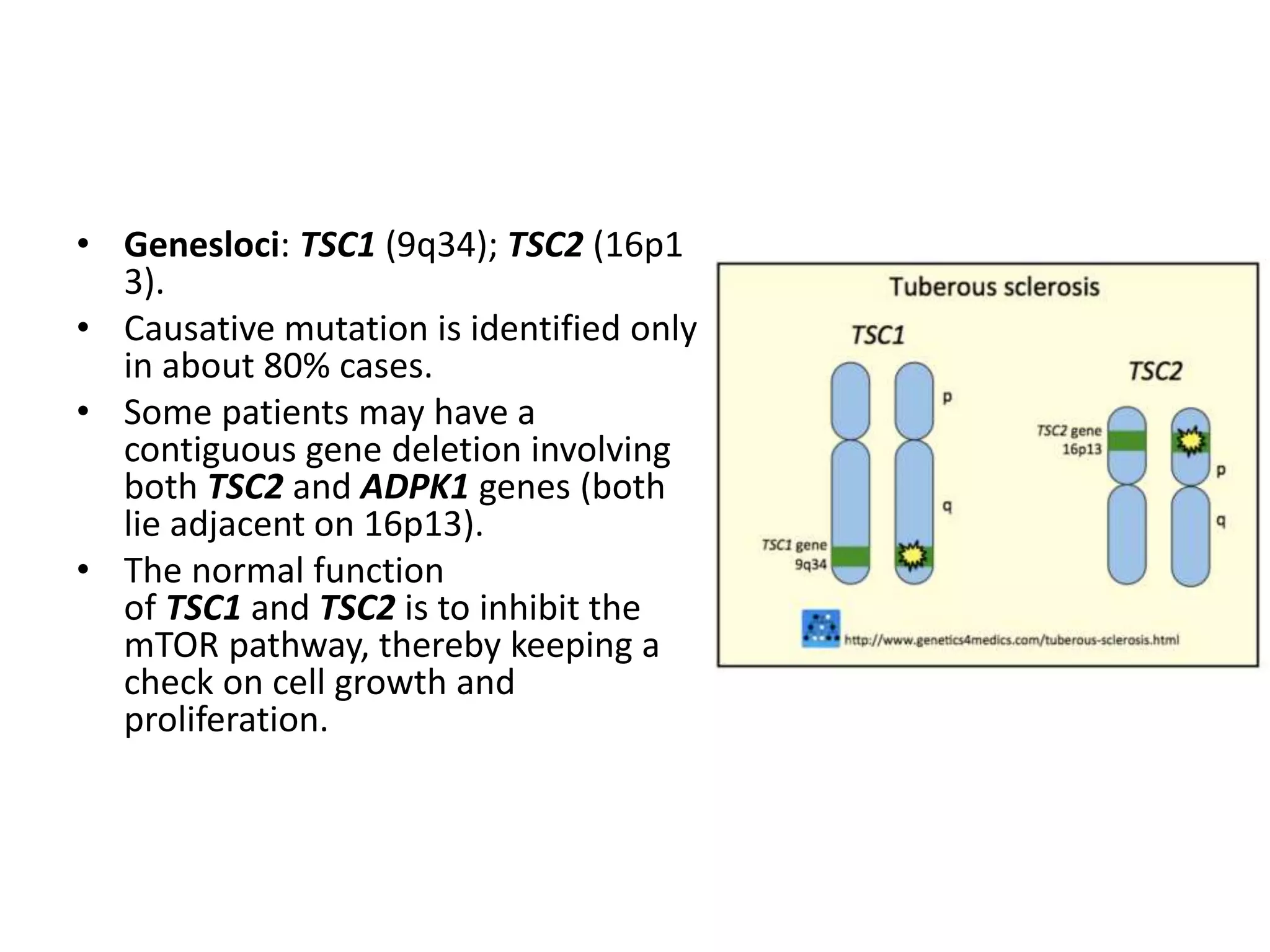
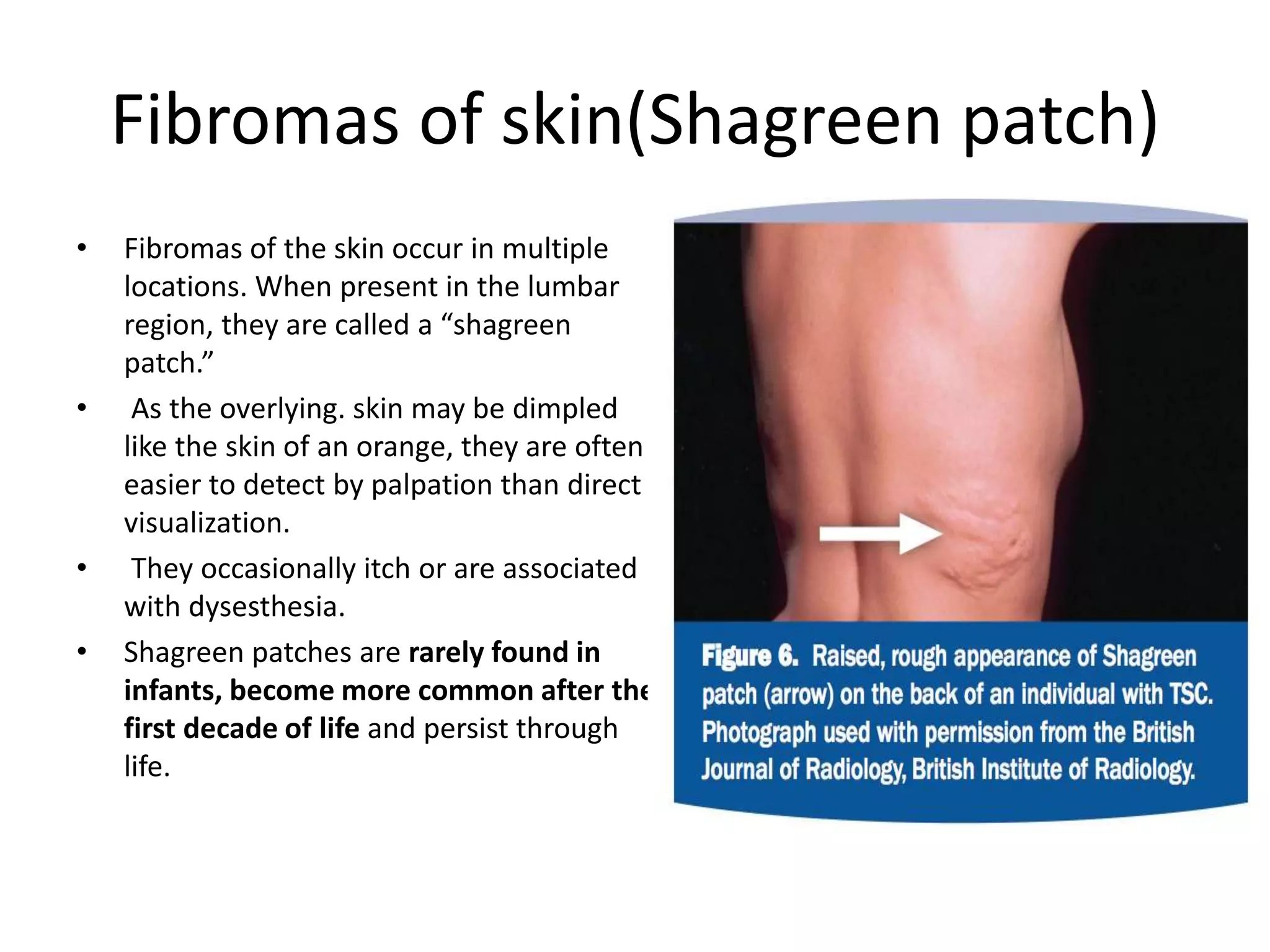
Tuberous sclerosis is a genetic disorder characterized by the growth of noncancerous tumors in multiple organs like the skin, brain, kidneys, and heart. It is caused by mutations in either the TSC1 or TSC2 genes. The signs and symptoms vary between people but can include skin abnormalities like hypomelanotic macules, facial angiofibromas, and shagreen patches. Neurological effects include seizures, developmental delays, and noncancerous brain tumors like subependymal nodules and subependymal giant cell astrocytomas. It has an autosomal dominant inheritance pattern and affects approximately 1 in 6,000 newborns. While there is no cure, treatment focuses