The document discusses various laboratory methods for the diagnosis of Mycobacterium tuberculosis infection and tuberculosis, including:
1) Microscopic examination of sputum or other samples to look for acid-fast bacilli via staining techniques.
2) Culture-based techniques to isolate M. tuberculosis from samples on solid or liquid media over several weeks.
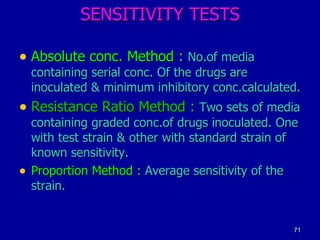
3) Biochemical and molecular tests to identify M. tuberculosis and determine drug resistance from cultures.
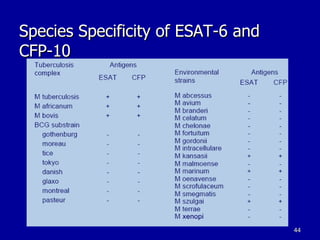
4) Immunological tests like the Mantoux test, interferon-gamma release assays, and ELISPOT to detect immune responses to M. tuberculosis antigens.









































![Whole Blood IFN- Assay QuantiFERON-TB Test Cellestis ESAT-6 CFP 10 Mitogen Control TMB COLOR Stage 1 Whole Blood Culture Stage 2 IFN-gamma ELISA Nil Control Incubate -> INF- from sensitized T-cells Draw blood + heparin Aliquot blood & add antigen Harvest plasma from above settled cells Measure [ IFN- ] in ‘Sandwich’ ELISA Computerized interpretation](https://image.slidesharecdn.com/labdiag-tb-111211062920-phpapp02/85/Lab-diag-tb-43-320.jpg)