The document provides detailed information on pulmonary tuberculosis, including its:
- Etiology (Mycobacterium tuberculosis bacteria)
- Pathophysiology (bacteria enter lungs and multiply, immune response leads to inflammation and tubercle formation)
- Clinical manifestations (cough, fever, weight loss, chest pain)
- Diagnosis (tuberculin skin test, chest X-ray, sputum culture to confirm M. tuberculosis)
- Treatment (mainly with anti-TB medications)

![fundamental differences to mammalian respiration. The respiratory systems of
non-homeotherms are also very different to that of mammals.
Introduction:
Tuberculosis is an infectious disease that primarily affects the lung
parenchyma. It may also affects the other parts of the body including the meninges,
kidney, bones, lymph nodes. The primary infectious agent is mycobacterium
tuberculosis, it is an acid fast aerobic rod that grows slowly and is sensitive to heat
and ultraviolet light. Mycobacterium bovis, mycobacterium avium have rarely
been associated with the development of a TB infection. TB is a world wide health
problem that is associated with the poverty, malnutrition, over crowding,
substandard housing, inadequate healthcare.
Definition:
A highly variable communicable disease of humans and some other vertebrates
that is caused by the tubercle bacillus and rarely in the U.S by a related
mycobacterium[mycobacterium bovis], that affects especially the lungs but spread
to other areas such as kidney or spinal column and that is characterized by fever,
cough, difficulty in breathing, formation of tuberculosis, caseation, pleural
effusion, and fibrosis.
Etiology and risk factors:
Etiology for tuberculosis can be divided into three types:
1. Agent factors
2. Host factors
3. Environmental factors
Agent factors:
The causative organism is mycobacterium tuberculosis which is an acid
fast aerobic rod that grows slowly and is sensitive to heat and ultraviolet radiation.](https://image.slidesharecdn.com/tuberculosisfinal-191222072753/85/Tuberculosis-3-320.jpg)

![ Immigration from countries with high prevelance of TB [southeastern asia,
Africa, latin America]
Institutionalization.
Living in crowded, substandard housing.
Statistics related to tuberculosis:
According to WHO,
8.8 million cases noted.
1.1 million deaths in 2010.
In the united states:
11,182 cases of TB were reported in 2010.
In india each year approximately 2,20,000 deaths were reported due to TB.
According to WHO, statistics for 2011 giving an estimated incidence
figure of 2.2 million cases of TB for india out of a global incidence of 9.6
million cases.](https://image.slidesharecdn.com/tuberculosisfinal-191222072753/85/Tuberculosis-5-320.jpg)









![ Household family members of patients with active disease.
Patients with HIV infection
Patients with fibrotic leisons suggestive of old TB
Patients whose current PPD test results shows a change from
former test results, suggesting recent exposure to TB and possible
infection.
Users of IV injections or drugs
Patients with high risk co morbid conditions
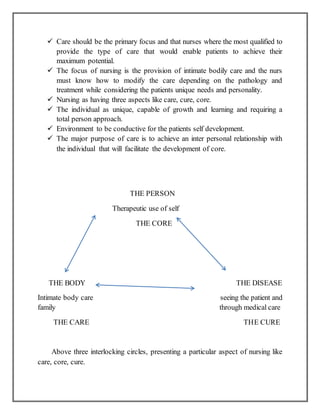
Directly observed treatment, short-course (DOTS, also known as TB-DOTS) :
it is the name given to the tuberculosis (TB) control strategy recommended by
the world health organization.[1]According to WHO, "The most cost-effective way
to stop the spread of TB in communities with a high incidence is by curing it. The
best curative method for TB is known as DOTS."
DOTS have five main components:
Government commitment (including political will at all levels, and
establishment of a centralized and prioritized system of TB monitoring,
recording and training)
Case detection by sputum smear microscopy
Standardized treatment regimen directly of six to nine months observed by a
healthcare worker or community health worker for at least the first two months
Drug supply
A standardized recording and reporting system that allows assessment of
treatment results
Nursing management:
Nursing management includes promoting airway clearance, advocating
adherence to the treatment regimen, promoting activity and nutrition and
preventing transmission.
Promoting airway clearance:
Safe expectoration of sputum
Safe sputum disposal](https://image.slidesharecdn.com/tuberculosisfinal-191222072753/85/Tuberculosis-17-320.jpg)







![Infection with M. tuberculosis can evolve from containment in the host, in which
the bacteria are isolated within granulomas (latent TB infection), to a contagious
state, in which the patient will show symptoms that can include cough, fever,
night sweats and weight loss. Only active pulmonary TB is contagious. In many
low-income and middle-income countries, TB continues to be a major cause of
morbidity and mortality, and drug-resistant TB is a major concern in many
settings. Although several new TB diagnostics have been developed, including
rapid molecular tests, there is a need for simpler point-of-care tests. Treatment
usually requires a prolonged course of multiple antimicrobials, stimulating
efforts to develop shorter drug regimens. Although the Bacillus Calmette–Guérin
(BCG) vaccine is used worldwide, mainly to prevent life-threatening TB in
infants and young children, it has been ineffective in controlling the global TB
epidemic. Thus, efforts are underway to develop newer vaccines with improved
efficacy. New tools as well as improved programme implementation and
financing are necessary to end the global TB epidemic by 2035.
Vishal Goyal, Vijay Kadam, Prashant Narang and Vikram Singh,drug-
resistant pulmonary tuberculosis (DR-TB) is a significant public health issue that
considerably deters the ongoing TB control efforts in India. A systematic review
of published studies reporting prevalence of DR-TB from biomedical databases
(PubMed and IndMed) was conducted. Meta-analysis was performed using
random effects model and the pooled prevalence estimate (95% confidence
interval [CI]) of DR-TB, multidrug resistant (MDR-) TB, pre-extensively
drugresistant (pre-XDR) TB and XDR-TB were calculated across two study
periods (decade 1: 1995 to 2005; decade 2: 2006 to 2015), countrywide and in
different regions. Heterogeneity in this meta-analysis was assessed using I2
statistic. Results: A total of 75 of 635 screened studies that fulfilled the inclusion
criteria were selected. Over 40% of 45,076 isolates suspected for resistance to
any first-line anti-TB drugs tested positive. Comparative analysis revealed a
worsening trend in DR-TB between the two study decades (decade 1: 37.7%
[95% CI = 29.0; 46.4], n = 25 vs decade 2: 46.1% [95% CI = 39.0; 53.2], n =
36). The pooled estimate of MDR-TB resistance was higher in previously treated
patients (decade 1: 29.8% [95% CI = 20.7; 39.0], n = 13; decade 2: 35.8% [95%
CI = 29.2; 42.4], n = 24) as compared with the newly diagnosed cases (decade 1:
4.1% [95% CI = 2.7; 5.6], n = 13; decade 2: 5.6% [95% CI = 3.8; 7.4], n = 17).
Overall, studies from Western states of India reported highest prevalence of DR-
TB (57.8% [95% CI = 37.4; 78.2], n = 6) and MDR-TB (39.9% [95% CI = 21.7;
58.0], n = 6) during decade 2. Prevalence of pre-XDR TB was 7.9% (95% CI =
4.4; 11.4, n = 5) with resistance to fluoroquinolone (66.3% [95% CI = 58.2;
74.4], n = 5) being the highest. The prevalence of XDR-TB was 1.9% (95% CI =](https://image.slidesharecdn.com/tuberculosisfinal-191222072753/85/Tuberculosis-28-320.jpg)