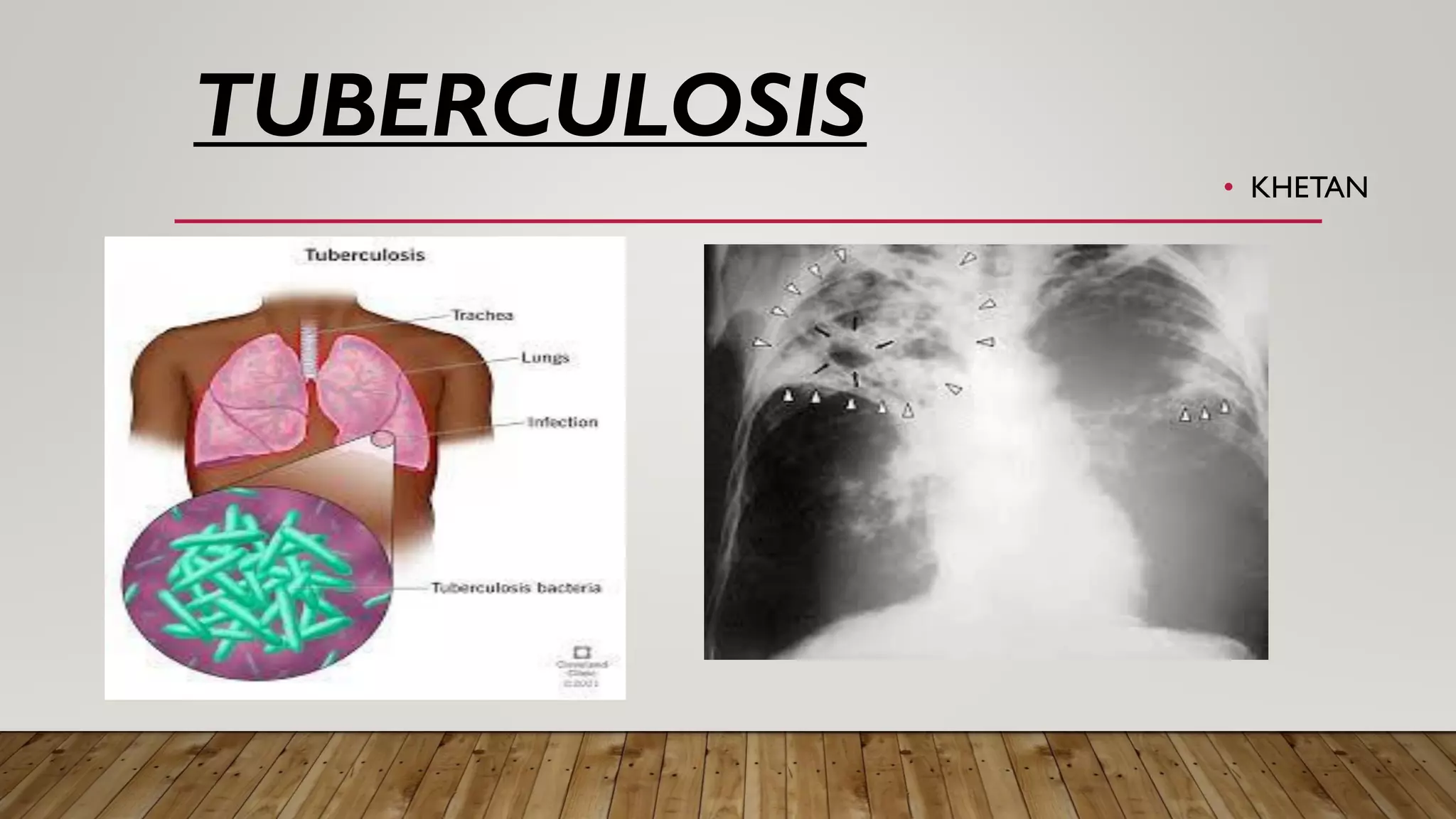
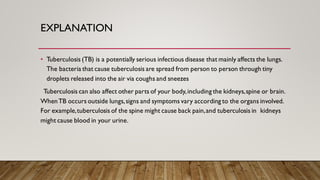
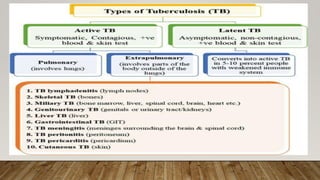
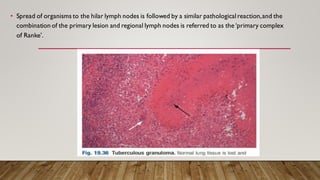
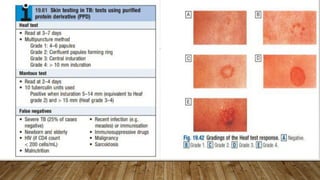
Tuberculosis is an infectious disease that mainly affects the lungs and is caused by the Mycobacterium tuberculosis bacteria. It spreads through tiny droplets released into the air via coughs and sneezes. Common symptoms include coughing for more than three weeks, coughing up blood or mucus, chest pain, unintentional weight loss, fever, and night sweats. Diagnosis involves skin tests, blood tests, chest x-rays, and sputum samples. Treatment requires taking combinations of antibiotics for several months. Complications can include spinal pain, joint damage, meningitis, and liver or kidney problems.