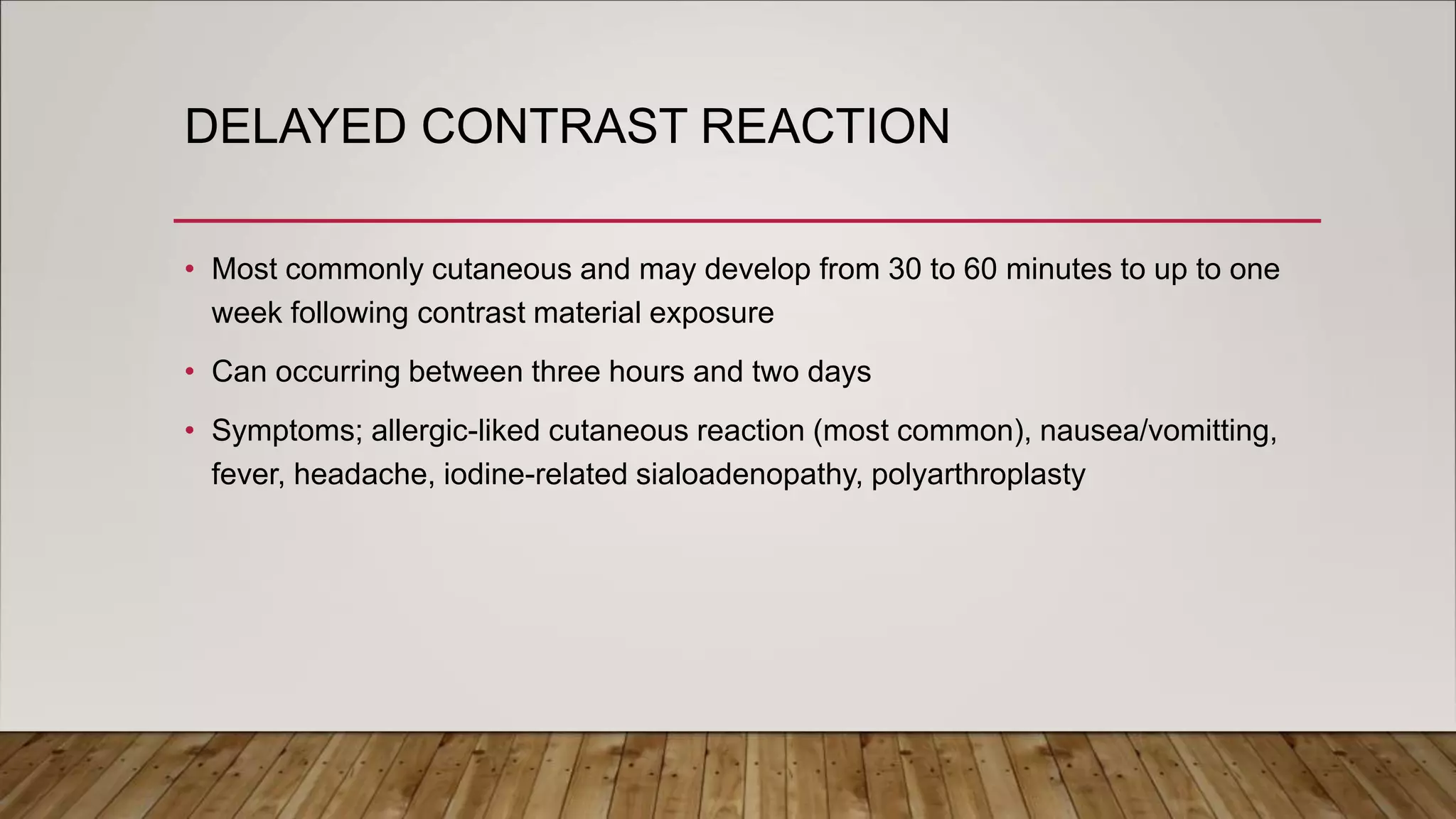
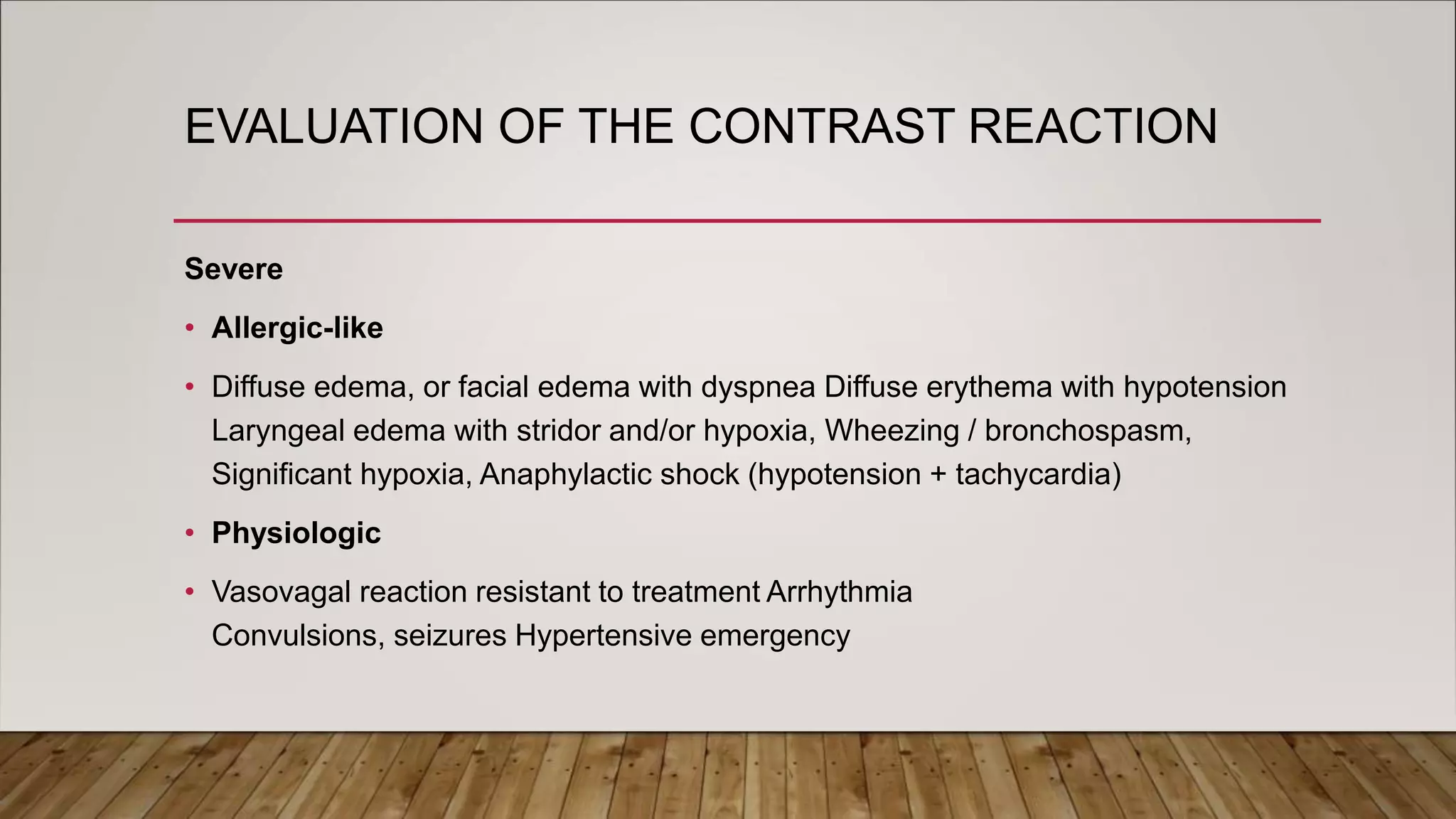
This document discusses contrast media used in radiology. It describes different types of contrast agents including iodinated, MR, and negative contrast agents. Iodinated contrast media can be ionic or non-ionic, and non-ionic agents have fewer adverse effects. Risk factors for contrast reaction include allergy, asthma, renal insufficiency, and cardiac issues. Reactions range from mild to severe and treatments involve medications like antihistamines, epinephrine, and IV fluids. Contrast-induced nephropathy is a deterioration of renal function caused by iodinated contrast and risk is highest in those with pre-existing severe renal insufficiency.