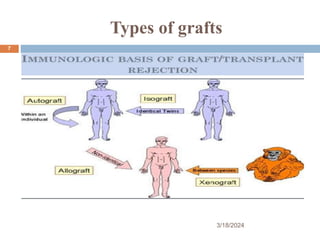
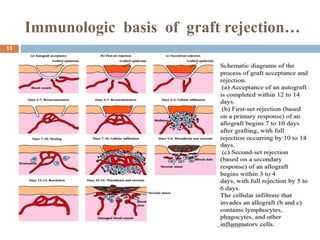
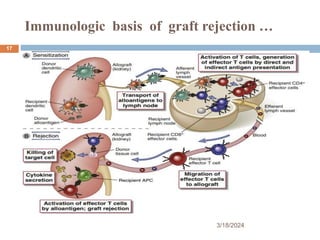
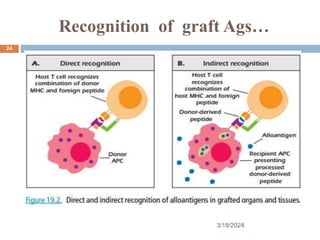
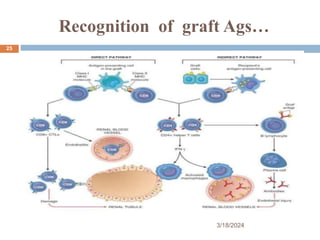
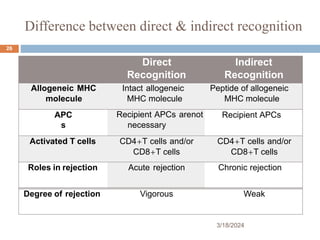
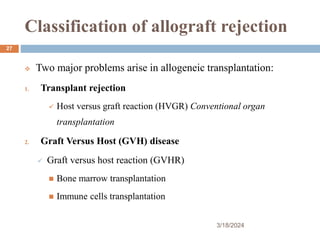
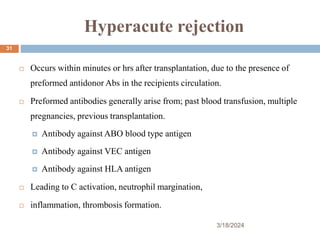
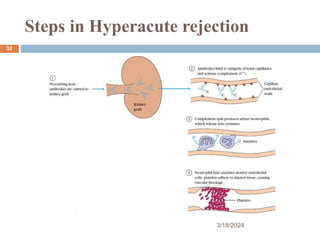
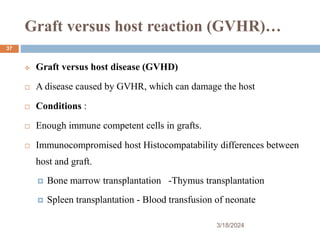
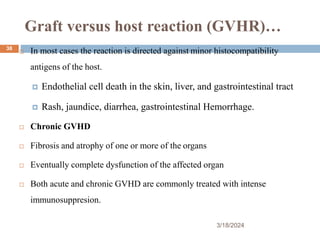
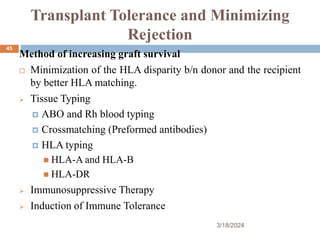
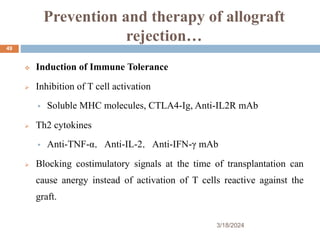
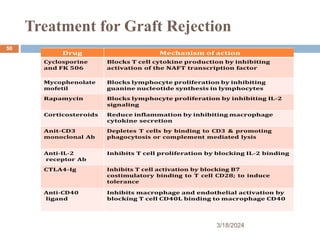
Transplantation and graft rejection involves complex immune mechanisms. There are different types of grafts including autografts, isografts, allografts, and xenografts which elicit varying immune responses. Major histocompatibility antigens are the main antigens that cause fast and strong rejection through direct or indirect antigen recognition. Graft rejection is classified as hyperacute, acute, or chronic rejection based on timing and mechanisms involving antibodies, T cells, and inflammation. Prevention strategies aim to minimize rejection by controlling these immune responses.