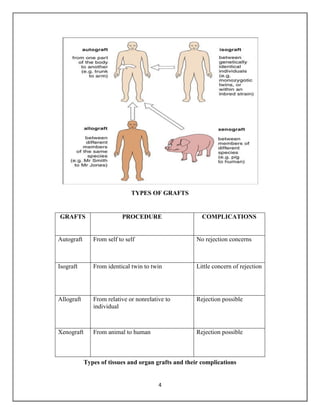
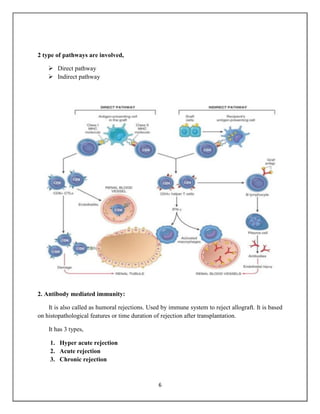
Transplantation involves moving cells, tissues, or organs from one individual to another, with kidney transplants being the most common in the UK. The immune system's response can lead to graft rejection, which depends on the genetic compatibility between donor and recipient. Types of grafts include autografts, allografts, isografts, and xenografts, each with varying risks of rejection, and management involves immunosuppressive drugs to reduce rejection rates.