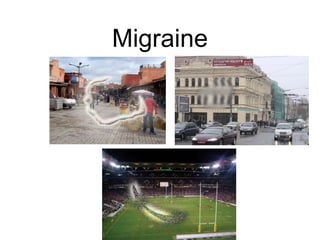
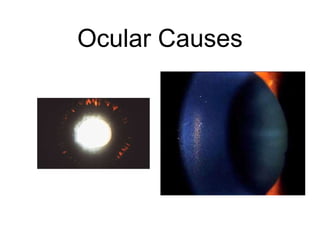
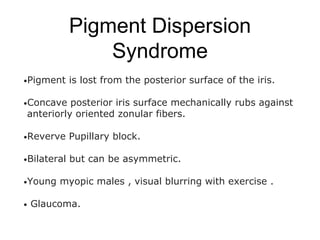
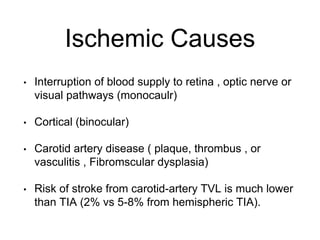
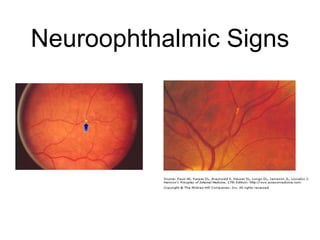
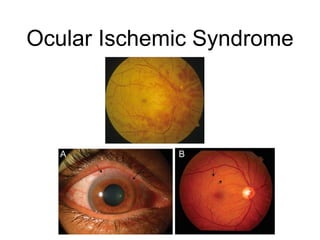
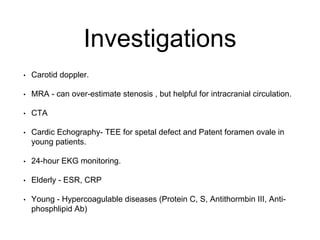
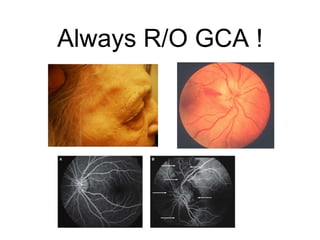
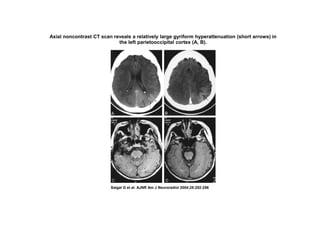
The document discusses transient visual loss (TVL), its common symptoms, causes (both ocular and non-ocular), and emphasizes the importance of a thorough clinical history and examination. It highlights ischemic causes, migraine-associated TVL, and the potential for serious conditions such as carotid artery disease. Various diagnostic approaches and treatments, including medication and surgical options, are also detailed for addressing TVL.