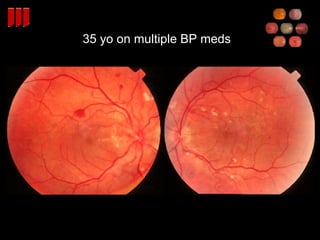
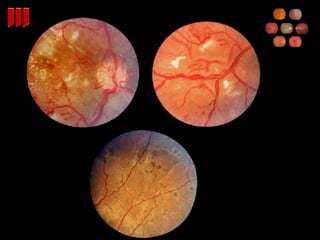
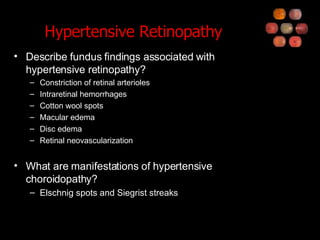
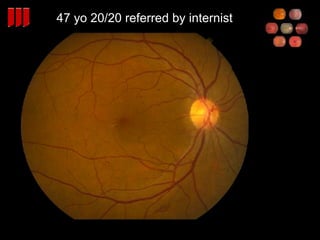
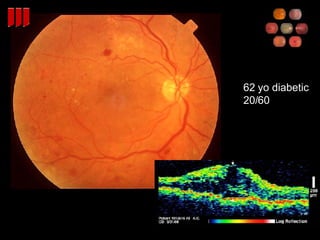
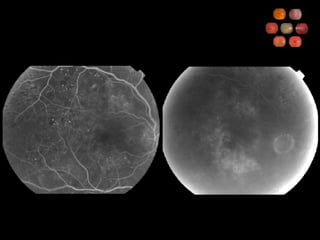
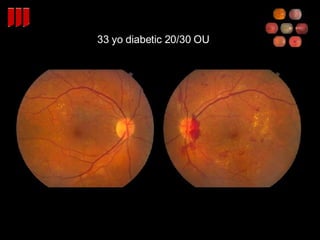
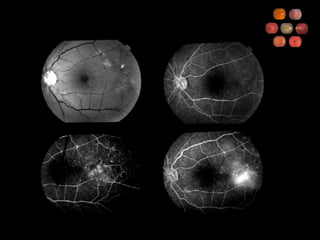
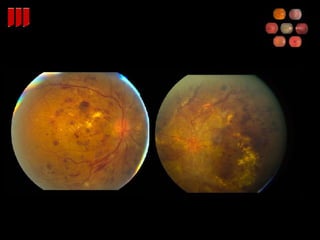
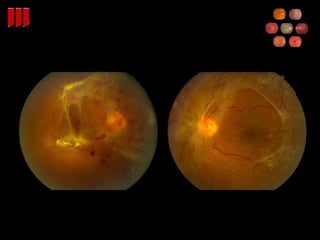
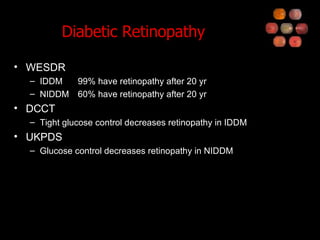
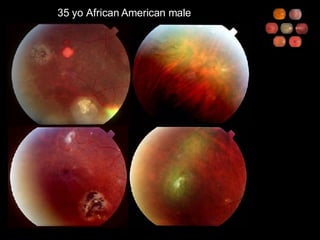
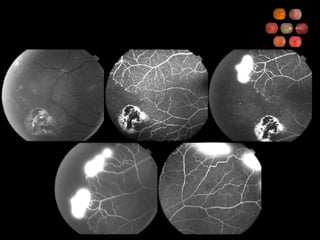
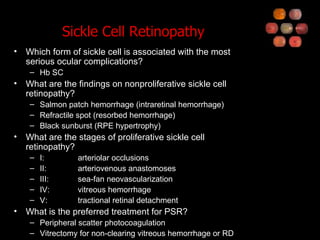
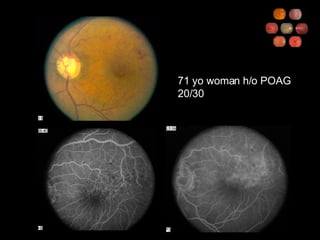
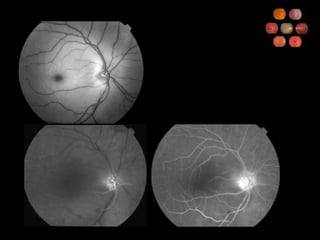
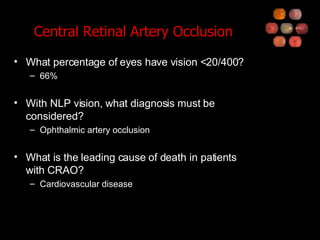
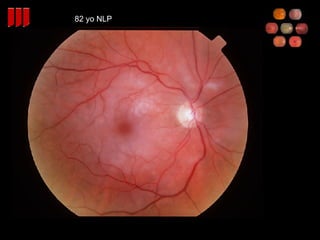
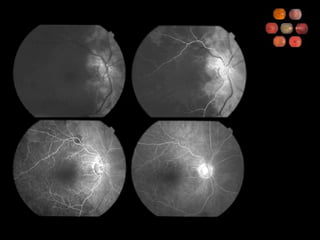
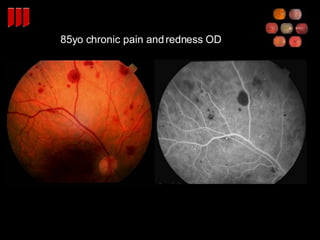
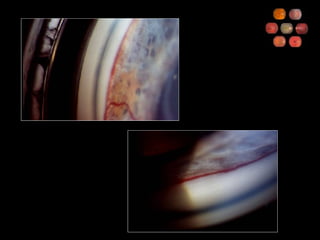
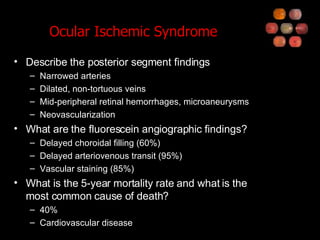
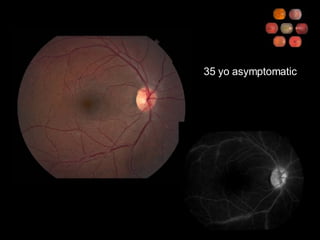
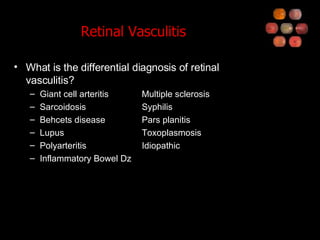
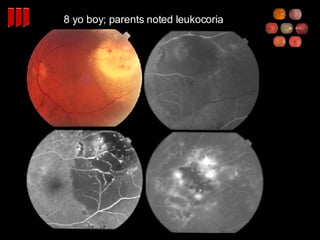
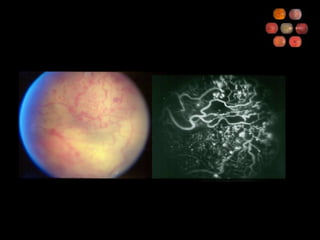
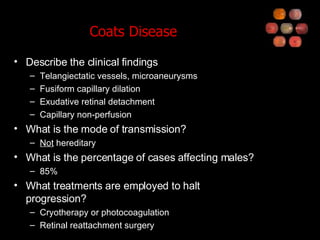
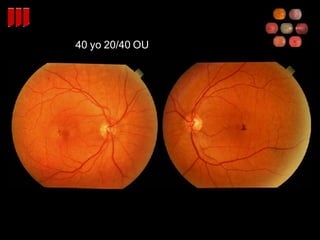
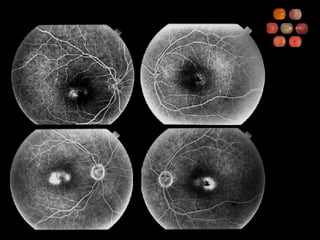
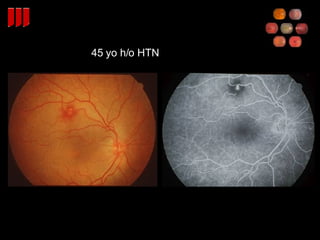
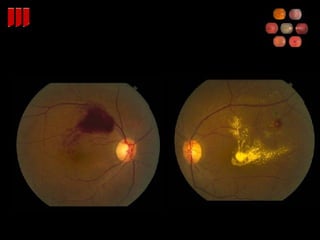
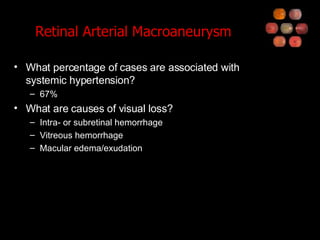
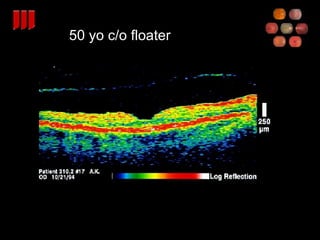
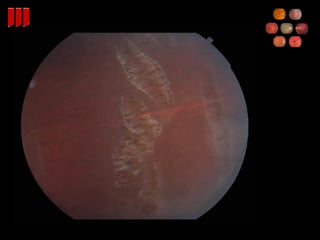
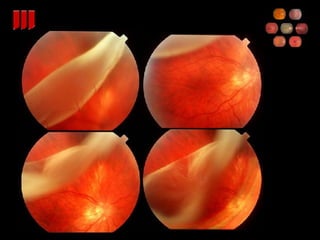
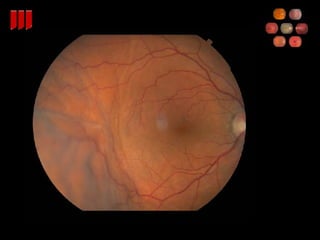
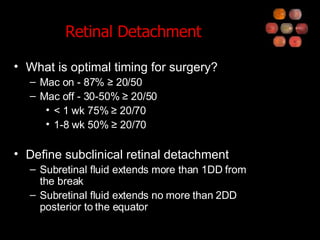
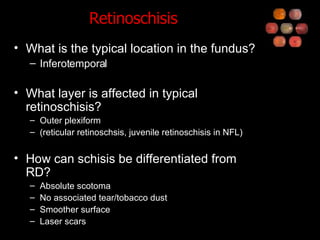
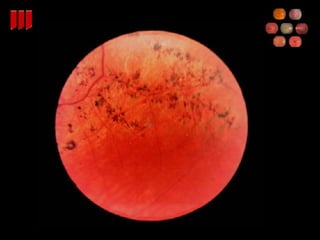
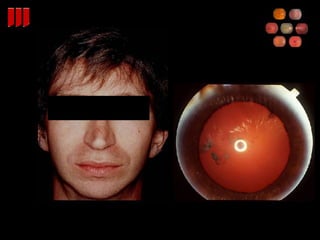
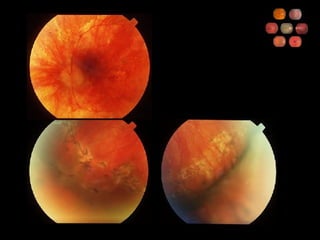
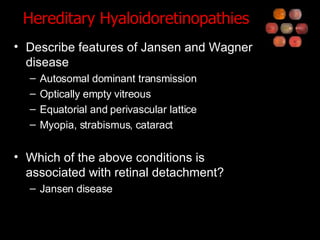
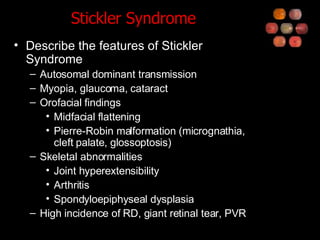
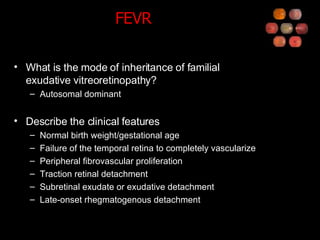
The document describes various retinal conditions and findings. It discusses hypertensive retinopathy, diabetic retinopathy, sickle cell retinopathy, retinopathy of prematurity, central retinal artery occlusion, ocular ischemic syndrome, Coats disease, lattice degeneration, retinal detachment, retinoschisis, hereditary hyaloidoretinopathies including Stickler syndrome and familial exudative vitreoretinopathy. It provides details on clinical findings, risk factors, treatments, and prognosis for each condition.