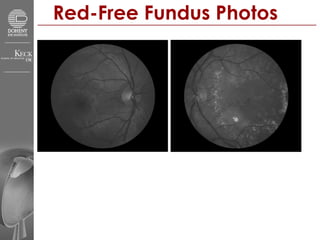
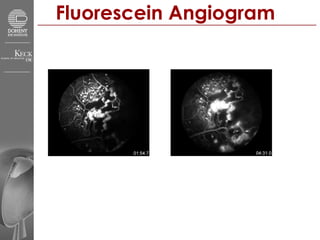
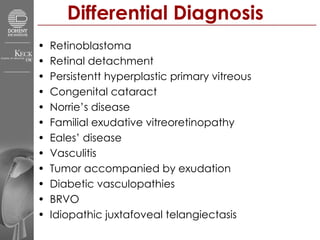
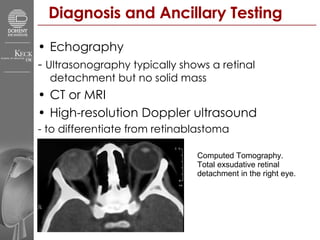
This document summarizes a presentation on Coats' disease in a 16-year-old male patient. Key details include fundus photos and angiogram images showing lipid-rich subretinal exudates in the posterior pole of the left eye. Coats' disease is described as an idiopathic condition characterized by telangiectatic and aneurysmal retinal blood vessels leading to intraretinal and subretinal exudation. Clinical features, pathogenesis, differential diagnosis, diagnostic testing, and treatment approaches are briefly outlined.