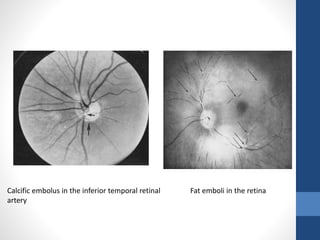
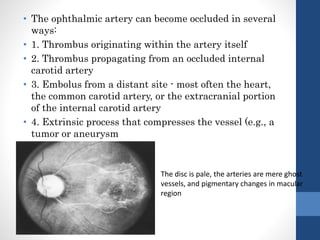
This document summarizes various neuro-ophthalmic manifestations of cerebrovascular diseases. It discusses atherosclerosis, strokes, raised intracranial pressure, cerebral aneurysms, cerebral venous thrombosis, migraines, embolisms, cervical arterial dissections, and effects on the internal carotid and vertebrobasilar arterial systems. Key signs involve visual field defects, transient vision loss, optic disc edema, retinal artery occlusions, and cranial nerve palsies. Imaging such as MRI and MRA are important for diagnosis and treatment involves managing risk factors, anticoagulation, and surgical intervention in some cases.