1. The document provides an overview of approaches to evaluating vision loss, including determining whether it is monocular or binocular and transient or persistent.
2. Examinations should include visual acuity, color vision, visual fields, pupils, and examination of the eyes and optic discs.
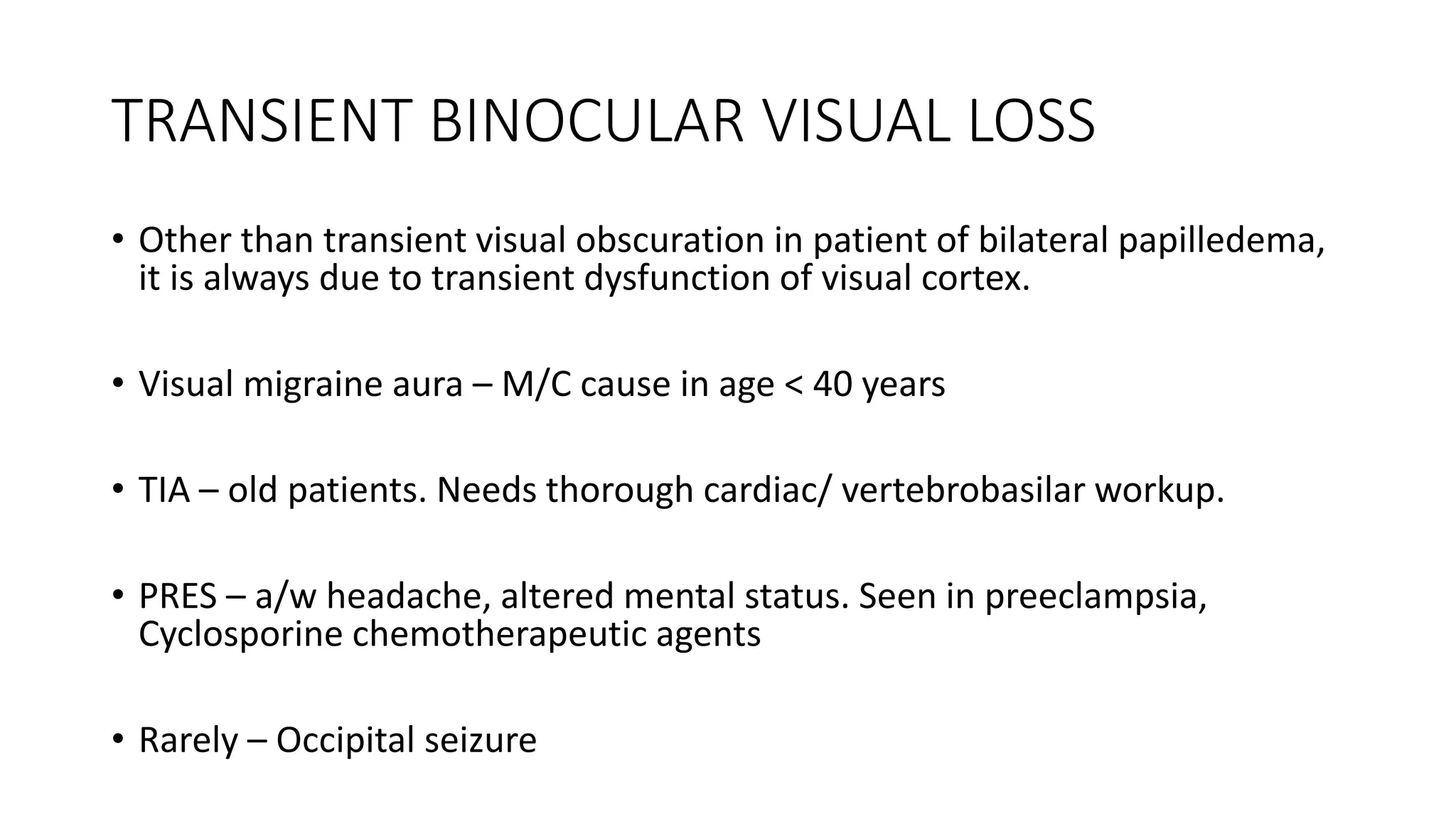
3. Causes of transient and acute vision loss are discussed, including optic neuropathies, ischemic events, migraine, and PRES.
4. Progressive vision loss may be due to compressive lesions, glaucoma, or retinal disorders.