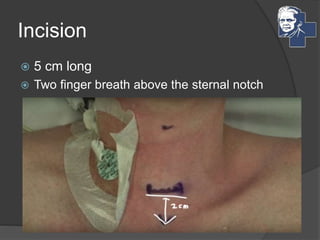
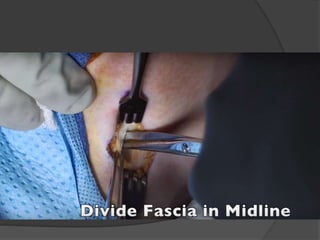
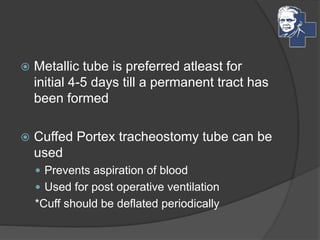
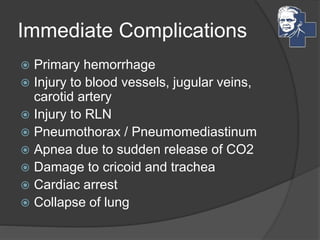
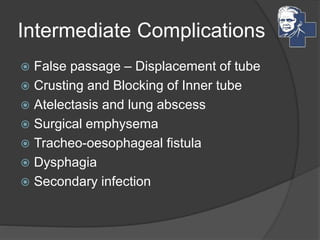
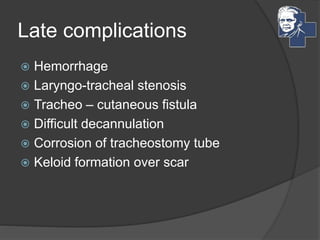
The document describes the procedure and indications for tracheostomy, which involves creating an opening in the trachea for airway access in cases of obstruction, pulmonary needs, or assisted ventilation. It outlines different causes leading to upper airway obstruction and details the types, techniques, and potential complications of tracheostomy, including considerations for infants and post-operative care. References to relevant literature and resources are also provided.