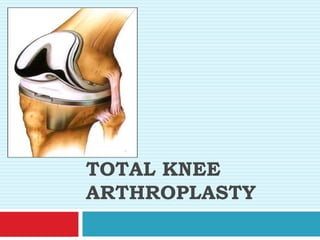
Total knee arthroplasty (TKA), also known as total knee replacement, involves replacing the knee joint with prosthetic components. It is commonly performed in older patients with severe knee osteoarthritis to relieve pain and improve physical function. The knee joint is made up of the femur, tibia, and patella bones. During TKA, the ends of the femur and tibia are reshaped and metal and plastic implants are attached. Rehabilitation after TKA follows three phases - maximum, moderate, and minimum protection - focusing on restoring range of motion, strengthening muscles, and retraining walking. The goals of TKA are to reduce pain and improve quality of life.