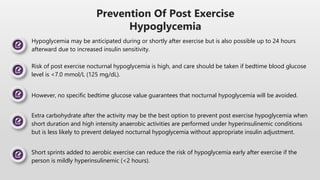
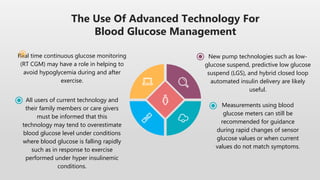
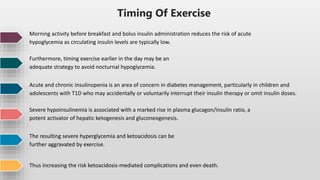
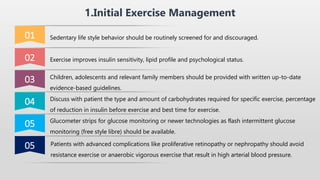
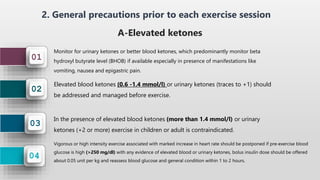
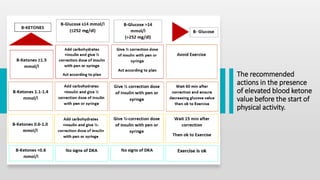
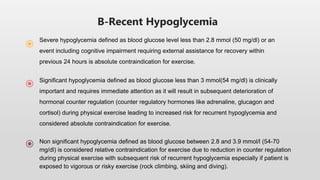
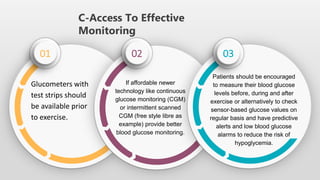
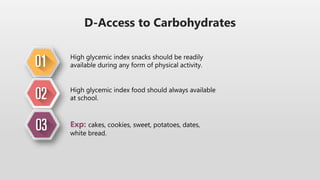
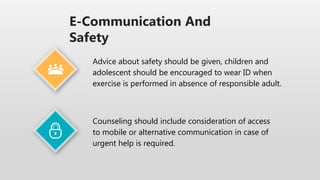
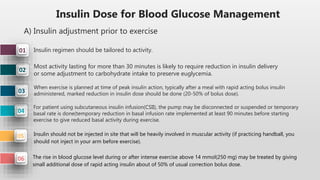
This document provides guidelines for exercise in diabetes. It discusses monitoring blood glucose levels before, during, and after exercise. It recommends adjusting insulin doses based on the timing and intensity of exercise to prevent hypoglycemia. The guidelines cover carbohydrate intake, types of exercise, and using technology like CGM to help manage blood sugars. Precautions are discussed for different situations like recent hypoglycemia or elevated ketones.
![B)Insulin Adjustments For The Afternoon Or Late
Evening After Exercise
03
02
01
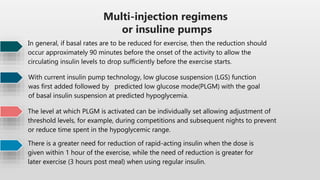
Similarly, morning exercise tends to lower insulin needs in the early afternoon. Two or more
activity sessions in a single day (camps, tournaments, intensive training) promotes increased
risk for hypoglycemia, and in particular nocturnal hypoglycemia.
In CSII treatment, a temporary basal reduction of approximately 20% at bedtime for 6 hours
helps reduce the risk of nocturnal hypoglycemia.
In Multiple Daily Injections (MDI) treatment, a 20% dose reduction of basal analogue (e.g., insulin
glargine, detemir, neutral protamine Hagedorn [NPH]) on the day of exercise together with a
carbohydrate snack at bedtime, corresponding to 0.4 g carbohydrates/kg reduces the risk of
hypoglycemia.
The risk of nocturnal hypoglycemia is increased after afternoon exercise.](https://image.slidesharecdn.com/exerciseindiabetes-221102132950-aa43c6db/85/Exercise-in-diabetes-pptx-12-320.jpg)